An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager

Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Sleeping hours: what is the ideal number and how does age impact this?
Affiliations.
- 1 Healthy Active Living and Obesity Research Group, Children's Hospital of Eastern Ontario Research Institute, Ottawa, ON, Canada, [email protected].
- 2 Department of Pediatrics, University of Ottawa, Ottawa, ON, Canada, [email protected].
- 3 School of Human Kinetics, University of Ottawa, Ottawa, ON, Canada, [email protected].
- 4 School of Epidemiology and Public Health, University of Ottawa, Ottawa, ON, Canada, [email protected].
- PMID: 30568521
- PMCID: PMC6267703
- DOI: 10.2147/NSS.S163071
The objective of this narrative review paper is to discuss about sleep duration needed across the lifespan. Sleep duration varies widely across the lifespan and shows an inverse relationship with age. Sleep duration recommendations issued by public health authorities are important for surveillance and help to inform the population of interventions, policies, and healthy sleep behaviors. However, the ideal amount of sleep required each night can vary between different individuals due to genetic factors and other reasons, and it is important to adapt our recommendations on a case-by-case basis. Sleep duration recommendations (public health approach) are well suited to provide guidance at the population-level standpoint, while advice at the individual level (eg, in clinic) should be individualized to the reality of each person. A generally valid assumption is that individuals obtain the right amount of sleep if they wake up feeling well rested and perform well during the day. Beyond sleep quantity, other important sleep characteristics should be considered such as sleep quality and sleep timing (bedtime and wake-up time). In conclusion, the important inter-individual variability in sleep needs across the life cycle implies that there is no "magic number" for the ideal duration of sleep. However, it is important to continue to promote sleep health for all. Sleep is not a waste of time and should receive the same level of attention as nutrition and exercise in the package for good health.
Keywords: guidelines; life cycle; population heath; public health; recommendations; sleep.
PubMed Disclaimer
Conflict of interest statement
Disclosure The authors report no conflicts of interest in this work.
Normal self-reported sleep durations in…
Normal self-reported sleep durations in children aged 0–12 years. Note: The mean reference…
Normal actigraphy-determined sleep duration values…
Normal actigraphy-determined sleep duration values in children aged 3–18 years. Note: The mean…
Sleep duration estimates of Canadians…
Sleep duration estimates of Canadians (dashed line) compared with the sleep duration recommendation…
Similar articles
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, Moraleda C, Rogers L, Daniels K, Green P. Crider K, et al. Cochrane Database Syst Rev. 2022 Feb 1;2(2022):CD014217. doi: 10.1002/14651858.CD014217. Cochrane Database Syst Rev. 2022. PMID: 36321557 Free PMC article.
- Lack of sleep as a contributor to obesity in adolescents: impacts on eating and activity behaviors. Chaput JP, Dutil C. Chaput JP, et al. Int J Behav Nutr Phys Act. 2016 Sep 26;13(1):103. doi: 10.1186/s12966-016-0428-0. Int J Behav Nutr Phys Act. 2016. PMID: 27669980 Free PMC article.
- Implementing the 2009 Institute of Medicine recommendations on resident physician work hours, supervision, and safety. Blum AB, Shea S, Czeisler CA, Landrigan CP, Leape L. Blum AB, et al. Nat Sci Sleep. 2011 Jun 24;3:47-85. doi: 10.2147/NSS.S19649. Print 2011. Nat Sci Sleep. 2011. PMID: 23616719 Free PMC article.
- [Sleepiness among adolescents: etiology and multiple consequences]. Davidson-Urbain W, Servot S, Godbout R, Montplaisir JY, Touchette E. Davidson-Urbain W, et al. Encephale. 2023 Feb;49(1):87-93. doi: 10.1016/j.encep.2022.05.004. Epub 2022 Aug 12. Encephale. 2023. PMID: 35970642 Review. French.
- Consensus recommendations on sleeping problems in Phelan-McDermid syndrome. San José Cáceres A, Landlust AM, Carbin JM; European Phelan-McDermid Syndrome consortium; Loth E. San José Cáceres A, et al. Eur J Med Genet. 2023 Jun;66(6):104750. doi: 10.1016/j.ejmg.2023.104750. Epub 2023 Mar 23. Eur J Med Genet. 2023. PMID: 36963463 Review.
- Assessing the influence of sleep and sampling time on metabolites in oral fluid: implications for metabolomics studies. Scholz M, Steuer AE, Dobay A, Landolt HP, Kraemer T. Scholz M, et al. Metabolomics. 2024 Aug 7;20(5):97. doi: 10.1007/s11306-024-02158-3. Metabolomics. 2024. PMID: 39112673 Free PMC article.
- The Effect of a Cognitive Dual Task on Gait Parameters among Healthy Young Adults with Good and Poor Sleep Quality: A Cross-Sectional Analysis. Dalbah J, Zadeh SAM, Kim M. Dalbah J, et al. J Clin Med. 2024 Apr 27;13(9):2566. doi: 10.3390/jcm13092566. J Clin Med. 2024. PMID: 38731095 Free PMC article.
- Trends and regional distribution in health-related quality of life across sex and employment status: a repeated population-based cross-sectional study. Ahn SK, Seo HJ, Choi MJ. Ahn SK, et al. J Occup Health. 2024 Jan 4;66(1):uiae017. doi: 10.1093/joccuh/uiae017. J Occup Health. 2024. PMID: 38604179 Free PMC article.
- Sleep behavioral outcomes of school-based interventions for promoting sleep health in children and adolescents aged 5 to 18 years: a systematic review. Gaskin CJ, Venegas Hargous C, Stephens LD, Nyam G, Brown V, Lander N, Yoong S, Morrissey B, Allender S, Strugnell C. Gaskin CJ, et al. Sleep Adv. 2024 Mar 29;5(1):zpae019. doi: 10.1093/sleepadvances/zpae019. eCollection 2024. Sleep Adv. 2024. PMID: 38584765 Free PMC article. Review.
- Associations Among Sleep, Emotional Eating, and Body Dissatisfaction in Adolescents. White ML, Triplett OM, Morales N, Van Dyk TR. White ML, et al. Child Psychiatry Hum Dev. 2024 Apr 5. doi: 10.1007/s10578-024-01692-4. Online ahead of print. Child Psychiatry Hum Dev. 2024. PMID: 38578582
- Chaput JP, Gray CE, Poitras VJ, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6 Suppl 3):S266–S282. - PubMed
- Chaput JP, Gray CE, Poitras VJ, et al. Systematic review of the relationships between sleep duration and health indicators in the early years (0–4 years) BMC Public Health. 2017;17(Suppl 5):855. - PMC - PubMed
- St-Onge MP, Grandner MA, Brown D, et al. Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American Heart Association. Circulation. 2016;134(18):e367–386. - PMC - PubMed
- Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9–17. - PMC - PubMed
- Gruber R, Carrey N, Weiss SK, et al. Position statement on pediatric sleep for psychiatrists. J Can Acad Child Adolesc Psychiatry. 2014;23(3):174–195. - PMC - PubMed
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Dove Medical Press
- Europe PubMed Central
- PubMed Central

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
When you buy through our links, we may earn a commission. Products or services may be offered by an affiliated entity. Learn more.
How Much Sleep Do You Need?

Staff Writer
Eric Suni has over a decade of experience as a science writer and was previously an information specialist for the National Cancer Institute.
Want to read more about all our experts in the field?

Dr. Abhinav Singh
Sleep Medicine Physician
Dr. Singh is the Medical Director of the Indiana Sleep Center. His research and clinical practice focuses on the entire myriad of sleep disorders.
Sleep Foundation
Fact-Checking: Our Process
The Sleep Foundation editorial team is dedicated to providing content that meets the highest standards for accuracy and objectivity. Our editors and medical experts rigorously evaluate every article and guide to ensure the information is factual, up-to-date, and free of bias.
The Sleep Foundation fact-checking guidelines are as follows:
- We only cite reputable sources when researching our guides and articles. These include peer-reviewed journals, government reports, academic and medical associations, and interviews with credentialed medical experts and practitioners.
- All scientific data and information must be backed up by at least one reputable source. Each guide and article includes a comprehensive bibliography with full citations and links to the original sources.
- Some guides and articles feature links to other relevant Sleep Foundation pages. These internal links are intended to improve ease of navigation across the site, and are never used as original sources for scientific data or information.
- A member of our medical expert team provides a final review of the content and sources cited for every guide, article, and product review concerning medical- and health-related topics. Inaccurate or unverifiable information will be removed prior to publication.
- Plagiarism is never tolerated. Writers and editors caught stealing content or improperly citing sources are immediately terminated, and we will work to rectify the situation with the original publisher(s)
- Although Sleep Foundation maintains affiliate partnerships with brands and e-commerce portals, these relationships never have any bearing on our product reviews or recommendations. Read our full Advertising Disclosure for more information.
Table of Contents
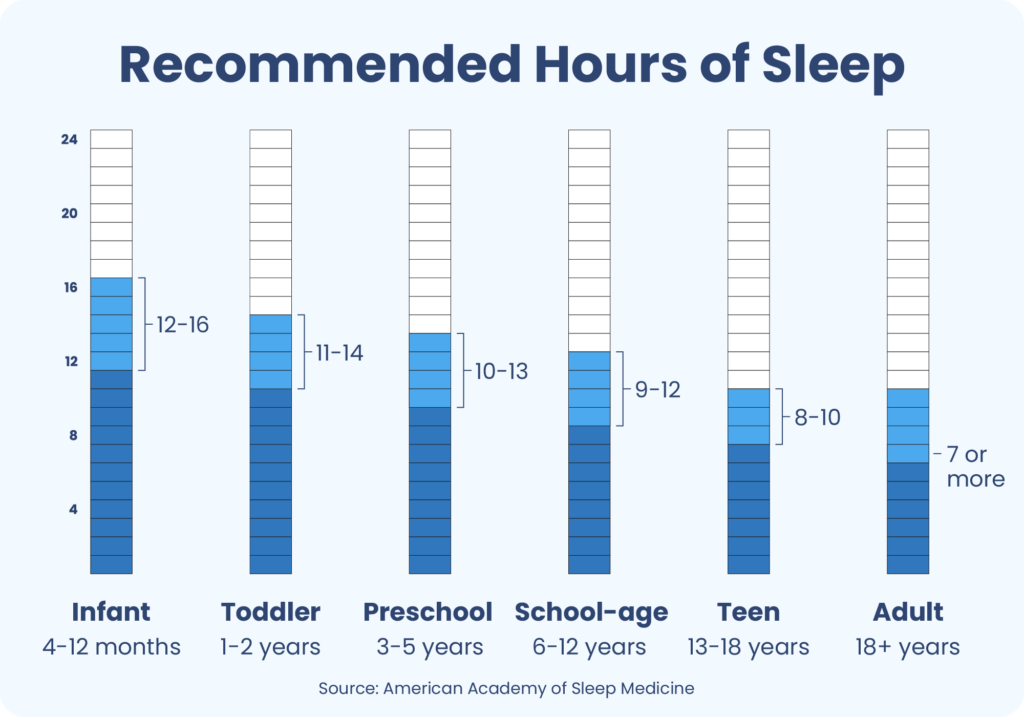
Recommended Sleep Times By Age Group
How much sleep is really necessary, how were the recommendations created, make sleep a priority.
- Most healthy adults need at least seven hours of sleep each night.
- Infants, young children, and teenagers should get more sleep to support growth and development.
- Prioritize getting enough sleep each night to stay happy, healthy, and sharp.
Healthy adults need at least seven hours of sleep per night. Babies, young children, and teens need even more sleep to enable their growth and development.
Knowing the general recommendations for how much sleep you need is a first step. Next, it is important to reflect on your individual needs based on factors like your activity level and overall health. And finally, of course, it is necessary to apply healthy sleep tips so that you can actually get the full night’s sleep that is recommended.
Essential Products for Better Sleep

Best Sleep Mask
Manta Pro Sleep Mask

Best Earplugs for Sleep
Loop Quiet Earplugs

Best Melatonin Supplements
Sleep Is the Foundation Sleep Support Melatonin Capsules

Best Sleep Coaching Program
Sleep Doctor Adult Sleep Coaching
| Age group | Age range | |
|---|---|---|
| Infant | 4-12 months | 12-16 hours (including naps) |
| Toddler | 1-2 years | 11-14 hours (including naps) |
| Preschool | 3-5 years | 10-13 hours (including naps) |
| School-age | 6-12 years | 9-12 hours |
| Teen | 13-18 years | 8-10 hours |
| Adult | 18 years and older | 7 hours or more |
Different age groups need different amounts of sleep. In each group, the guidelines present a recommended range Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source of nightly sleep duration for healthy individuals. In some cases, sleeping an hour more or less than the general range may be acceptable based on a person’s circumstances.
Sleep recommendations for newborns are not available because sleep needs in this age group vary widely Trusted Source UpToDate More than 2 million healthcare providers around the world choose UpToDate to help make appropriate care decisions and drive better health outcomes. UpToDate delivers evidence-based clinical decision support that is clear, actionable, and rich with real-world insights. View Source and can range from as few as 11 hours to as many as 19 hours per 24-hour period.
These guidelines serve as a rule-of-thumb for how much sleep babies , children, and adults need Trusted Source National Library of Medicine, Biotech Information The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information. View Source while acknowledging that the ideal amount of sleep can vary from person to person. Some people need more or less sleep each night than those reflected in the ranges.
Deciding how much sleep you need means considering your overall health, daily activities, and typical sleep patterns. Some questions that you help assess your individual sleep needs include:
- Are you productive, healthy, and happy on seven hours of sleep? Or have you noticed that you require more hours of sleep to get into high gear?
- Do you have coexisting health issues that might require more rest?
- Do you have a high level of daily energy expenditure? Do you frequently play sports or work in a labor-intensive job?
- Do your daily activities require alertness to do them safely? Do you drive every day and/or operate heavy machinery? Do you ever feel sleepy when doing these activities?
- Are you experiencing or do you have a history of a sleep disorder ?
- Do you depend on caffeine to get you through the day?
- When you have an open schedule, do you tend to sleep in more?
You can use your answers to these questions to hone in on your optimal amount of sleep.
Sleep Better One Night at a Time

Sleep Doctor 28-Day Sleep Wellness Program
The American Academy of Sleep Medicine organized a panel of sleep experts to create these recommendations. The panel members reviewed hundreds of high-quality research studies about sleep duration and key health outcomes like cardiovascular disease, depression, pain, and diabetes.
After studying the evidence, the panel used several rounds of voting and discussion to narrow down the ranges for the amount of sleep needed at different ages. The final recommendations have been endorsed by other medical organizations, such as the Sleep Research Society, the American Academy of Pediatrics, and more.
Once you have a nightly sleep goal based on the hours of sleep that you need, it is time to start planning for how to make that a reality.
Start by making sleep a priority in your schedule. This means budgeting for the hours you need so that work or social activities do not trade off with sleep. While cutting sleep short may be tempting in the moment, it does not pay off in the long run because sleep is essential for you to perform at your best, both mentally and physically.
Getting more sleep is a key part of the equation, but remember that it is not just about sleep quantity. Quality sleep matters too, and it is possible to get the hours that you need but not feel refreshed because your sleep is fragmented or non-restorative. Fortunately, improving your bedroom setting and sleep-related habits, is an established way to get better rest. Examples of improvements include:
- Improving your sleep hygiene , which includes sticking to the same sleep schedule every day, even on weekends
- Practicing a relaxing bedtime routine to make it easier to fall asleep quickly
- Choosing the best mattress that is supportive and comfortable, and outfitting it with the best pillows and bedding .
- Minimizing potential disruptions from light and sound while optimizing your bedroom temperature
- Disconnecting from electronic devices like mobile phones and laptops for a half-hour or more before bed
- Carefully monitoring your intake of caffeine and alcohol and avoiding consumption in the hours before bed
If you are a parent or caregiver, many of the same tips apply to help children and teens get the recommended amount of sleep. Teens in particular face a number of unique sleep challenges to getting the sleep they need .
If you or a family member are experiencing symptoms such as significant sleepiness during the day, insomnia , leg cramps , snoring , or another symptom that is preventing you from sleeping well, you should consult your primary care doctor or find a sleep professional to determine the underlying cause.
You can try using our sleep diary to track your sleep habits. This can provide insight about your sleep patterns and needs. It can also be helpful to bring with you to the doctor if you have ongoing sleep problems.
- New Research Evaluates Accuracy of Sleep Trackers
- Listening to Calming Words While Asleep Boosts Deep Sleep
- Distinct Sleep Patterns Linked to Health Outcomes
- Association Between Sleep Duration and Disturbance with Age Acceleration
About Our Editorial Team

Eric Suni, Staff Writer

Medically Reviewed by
Dr. Abhinav Singh, Sleep Medicine Physician MD
References 3 sources.
Paruthi, S., Brooks, L. J., D’Ambrosio, C., Hall, W. A., Kotagal, S., Lloyd, R. M., Malow, B. A., Maski, K., Nichols, C., Quan, S. F., Rosen, C. L., Troester, M. M., & Wise, M. S. (2016). Consensus statement of the American Academy of Sleep Medicine on the recommended amount of sleep for healthy children: Methodology and discussion. Journal of Clinical Sleep Medicine, 12(11), 1549–1561.
Kirsch, D. (2022, September 12). Stages and architecture of normal sleep. In S. M. Harding (Ed.). UpToDate., Retrieved March 1, 2023, from
Consensus Conference Panel, Watson, N. F., Badr, M. S., Belenky, G., Bliwise, D. L., Buxton, O. M., Buysse, D., Dinges, D. F., Gangwisch, J., Grandner, M. A., Kushida, C., Malhotra, R. K., Martin, J. L., Patel, S. R., Quan, S. F., Tasali, E., Non-Participating Observers, Twery, M., Croft, J. B., Maher, E., … Heald, J. L. (2015). Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Journal of Clinical Sleep Medicine, 11(6), 591–592.
Learn More About How Sleep Works

Can You Learn a Language While Sleeping?

How to Become a Morning Person

How Memory and Sleep Are Connected

What Causes Excessive Sleepiness?

What Causes Restless Sleep?

Biphasic Sleep: What It Is And How It Works

Polyphasic Sleep: Benefits and Risks

Sleep Inertia: How to Combat Morning Grogginess

REM Rebound: Causes and Effects

Do Moon Phases Affect Your Sleep?

Why Do We Need Sleep?

Alpha Waves and Sleep

How Age Affects Your Circadian Rhythm

How Is Sleep Different For Men and Women?

Circadian Rhythm

Chronotypes: Definition, Types, & Effect on Sleep

Sleep Drive and Your Body Clock

8 Health Benefits of Sleep

Daylight Saving Time: Everything You Need to Know

How To Get a Good Night’s Sleep in a Hotel

Does Napping Impact Your Sleep at Night?

Does Daytime Tiredness Mean You Need More Sleep?

Why Do I Wake Up at 3 am?

Sleep Debt: The Hidden Cost of Insufficient Rest

Sleep Satisfaction and Energy Levels

How Sleep Works: Understanding the Science of Sleep

What Makes a Good Night's Sleep

What Happens When You Sleep?

Sleep and Social Media
Adenosine and Sleep: Understanding Your Sleep Drive

Oversleeping

Hypnagogic Hallucinations

Hypnopompic Hallucinations

What All-Nighters Do To Your Cognition

Long Sleepers

How to Wake Up Easier

Sleep Spindles

Does Your Oxygen Level Drop When You Sleep?

100+ Sleep Statistics

Short Sleepers

How Electronics Affect Sleep

Myths and Facts About Sleep

What’s the Connection Between Race and Sleep Disorders?

Sleep Latency

Microsleep: What Is It, What Causes It, and Is It Safe?

Light Sleeper: What It Means and What To Do About It
Other articles of interest, best mattresses, sleep testing and solutions, bedroom environment, sleep hygiene.
- Best Cooling Mattresses
- Best Hybrid Mattresses
- Best Mattresses for Back Pain
- Best Mattresses for Heavy People
- Best Mattresses for Side Sleepers
- Best Mattresses for Stomach Sleeping
- Best Mattress in a Box
- Best Mattresses on a Budget
- Best Memory Foam Mattresses
- Best Online Mattresses
- Best Sofa Beds and Sofa Sleepers
- Best Lumbar Pillows for Sleep
- Best Pillows for Back Sleeping
- Best Pillows for Neck Pain
- Best Pillows for Side Sleepers
- Best Pregnancy Pillows
- Best CBD Oils for Sleep and Insomnia
- Best CBD Oils for Pets
- Best Essential Oils for Sleep
- Best Silk Pillowcases for Your Hair & Skin
- Best Sleep Gadgets to Help You Sleep
- Best Weighted Blankets
- Best Weighted Blankets for Kids
- Best and Worst Cities for Sleep
- Depression and Sleep Statistics
- Fascinating Animal Sleep Facts
Sleep Statistics: Understanding Sleep and Sleep Disorders

Ryan Fiorenzi, BS, Certified Sleep Science Coach - Updated on July 12th, 2023
Over the past ten years, sleep research has accelerated at a pace never seen before. Organizations like the Sleep Research Society , the Centers for Disease Control and Prevention , the Mayo Clinic and the National Institutes of Health have shed more light on the importance of sleep. It is now known as the " third pillar " of good health.
To keep track of key findings, we track updates from trusted sources as they are published. Our goal is to simplify the key facts that come out of that research into our resources throughout the site and the statistics below. If you feel we have missed something that you think should be included, please let us know.
General Sleep Statistics
Average sleep times.
- Americans sleep 6.8 hours per day on average, which hasn't changed much from Gallup polls in the 1990s and 2000s, but is down more than an hour from 1942. 1
- 59% of Americans get 7 or more hours of sleep at night. In 1942, 84% met the standard of getting 7-9 hours per night of sleep. 1
- The older the age group, the more they report sleeping. Americans aged 65 and over report getting the most sleep, while 18-29-year-old report the least.
| Group | Sleep 6 hours or less | Sleep 7 hours or more |
|---|---|---|
| 18-29 year olds | ||
| 30-49 year olds | ||
| 50-64 year olds | ||
| 65+ year olds | ||
| Men | ||
| Women | ||
| Employed | ||
| Not employed | ||
| Less than $30,000 annual household income | ||
| Between $30,000 to $75,000 annual household income | ||
| $75,000 or more annual household income | ||
| Have children under 18 | ||
| Don't have children under 18 |
Source: Gallup, Dec. 5-8, 2013
Sleep Needs Statistics
Sleep needs by age as defined by the June 13, 2016, American Academy of Sleep Medicine (AASM) recommendations that the American Academy of Pediatrics (AAP) has endorsed. 2
| Age | Recommended Amount of Sleep |
|---|---|
| Infants aged 4-12 months | 12-16 hours a day (including naps) |
| Children aged 1-2 years | 11-14 hours a day (including naps) |
| Children aged 3-5 years | 10-13 hours a day (including naps) |
| Children aged 6-12 years | 9-12 hours a day |
| Teens aged 13-18 years | 8-10 hours a day |
| Adults aged 18 years or older | 7–8 hours a day |
- Women on average sleep five to 28 minutes longer than men. 3 The NIH found a variety of factors tied to this including differences in average lifestyle and employment.
- On average, women need 20 minutes more sleep per night. 4
Sleep Deprivation Statistics
- Adults need 7 hours or more of sleep per night for optimal health. 5 The statistics below define short sleep as less than 24 hours of sleep in 24 hours.
Prevalence of Short Sleep Duration (<7 hours) for Adults Aged ≥18 Years, by County, United States, 2014

- About one in four people aged 18 to 24 say that they don't sleep well because of technology. 5
- Sleep deprivation increases the expectation of gains and decreases the estimation of possible losses when gambling. 6
- Decision making in "high-stakes, real-world situations" is impaired when someone is experiencing sleep loss. 7
- Shift Work Sleep Disorder is a recognized medical condition for 20% of U.S. shift workers. 8
- 45% of Americans claim that poor sleep has made an impact on their daily life at least once in the last 7 days. 33
- More than 50% of Americans have taken a nap in the last 7 days. 23% took a nap 1-2 days, 13% took a nap 3-4 days, 17% took a nap at least 5 days. This may suggest that many Americans undersleep, though many countries take afternoon "siestas," and some sleep researchers theorize that humans may be wired to sleep in 2 sessions per day (in 2 sleep phases).

Sleep Disorders Statistics
Sleep disorders are very common. The NIH compiled the data below to support clinical practice guidelines for sleep disorders. 9
| Disorder | Prevalence |
|---|---|
| Insomnia | 10-15% |
| Hypersomnia | Not Known |
| Obstructive sleep apnea* | 14% |
| Restless legs syndrome* | 2% |
| Delayed sleep-wake phase disorder | 10% |
| Advanced sleep-wake phase disorder | 1% |
| Shift worker disorder | 2% |
Insomnia is a sleep disorder that leads to habitual sleeplessness or an inability to sleep.
- The yearly workplace cost in the US due to insomnia is an estimated $63.2 billion. 10
- One in four women suffers from insomnia. 11 This makes them twice as likely as men to have insomnia. 12
- Approximately 6% of adults suffer from insomnia. 13
Hypersomnia
Hypersomnia is a sleep disorder that leads to excessive daytime sleepiness or time spent sleeping.
- 4% to 6% of the general population has hypersomnia. 14
- Sleep apnea syndrome leads to hypersomnia, and there is a higher prevalence of this disorder in men. 15
- Narcolepsy only affects 0.026% of the general population. It is caused by the inability to regulate sleep-wake cycles normally. 16
Obstructive Sleep Apnea
Obstructive sleep apnea syndrome (OSAS) is a potentially serious sleeping disorder that causes people to repeatedly stop and start breathing during sleep.
- 5% to 20% of the adult population is affected by OSAS when assessed with sleep tests. 17
- It is seen in 1% to 3% of children of preschool age. 18
- OSAS prevalence is as high as 10% to 20% in children who habitually snore. 19
Restless Legs Syndrome
Restless legs syndrome (RLS) is a disorder characterized by overwhelming urges to move the legs to relieve unpleasant twitching or tickling sensations.
- 11% to 29% of pregnant women are affected by RLS.
- 25% to 50% of patients with end-stage renal disease have Restless Legs Syndrome
- Limb twitching during sleep occurs in 80% of patients with RLS. 20
Delayed Sleep-Wake Phase Disorder
Delayed sleep-wake phase disorder (DSWPD) is characterized by a delayed day and night cycle, often causing someone to fall asleep and wake later in the day.
Note that statistics vary widely on this condition as the consistency around definitions and diagnostic criteria tend to vary widely.
- 51% of patients with DSWPD have had a lifetime history of depression .
- 59% of adolescents with this disorder demonstrated poor academic performance, and 45% had behavioral problems. 21
- A prevalence of up to 8 percent has been reported in American teenagers. 22
Advanced Sleep-Wake Phase Disorder
Advanced Sleep Phase Disorder (ASPD), otherwise known as Advanced Sleep Phase Syndrome (ASPS), is a sleep disorder characterized by a shift in the circadian rhythm. This shift typically causes someone to go to bed earlier and wake up earlier. This is characterized by the correct quantity of sleep at undesired times of the day. Approximate averages are 8-9 pm bedtimes and 4-5 am awakenings. This disorder is not yet commonly understood.
- There is a 50% chance of passing ASPD on to children. 23
Shift Worker Disorder
Shift work sleep disorder (SWSD) is a sleep disorder characterized by excessive sleepiness and insomnia in people whose work schedules overlap with normal sleep times.
- 20% of the working population in Europe and North America is engaged in shiftwork 24
- The sleep-wake disturbance is severe enough to warrant diagnosis as SWSD in about 5 to 10 percent of night-shift workers.
- 37.5% of post-night-shift drives have been considered unsafe during testing. 25

Obesity and Sleep Statistics
Being overweight can affect sleep, and poor sleep can make it more likely to put on weight. Researchers from Johns Hopkins University School of Medicine studied 77 overweight volunteers with either prediabetes or type 2 diabetes. Many had issues getting high-quality sleep. Half of the group went on a weight-loss diet and exercise program, and the other half just followed the diet. After 6 months, both groups lost an average of 15 pounds and reduced their belly fat by 15%. The researchers concluded that a reduction in belly fat is a good way to improve sleep. 35
Sleep apnea is a sleep disorder where a sleeper will experience apneas or pauses in breathing while sleeping. Sufferers of sleep apnea often snore loudly, stop breathing during the night many times, often wake up with a dry mouth and/or headache, are tired during the day, and have trouble focusing. The chances of sleep apnea are increased by being overweight, as fat around the upper airway can block the airway, especially when sleeping on the back.
- A 20-year review of children ages 6-17 years with obesity-associated diseases found that hospital discharges for sleep apnea increased 436%.
- 18 million adult Americans have sleep apnea.
- A 1999 study from the University of Chicago found that sleep debt accumulated over a few days can slow metabolism and disrupt hormone levels. 11 healthy young adults were restricted to 4-6 hours of sleep per night. Their ability to process sugar in the blood had reduced, in some cases, to the level of diabetics. 33
- The Wisconsin Sleep Cohort Study concluded that short sleep was associated with 15.5% lower leptin levels and 14.9% elevated grehlin levels. Leptin is the hormone that suppresses appetite, and ghrelin stimulates appetite, increased food intake, and promotes fat storage. 34
- Oregan State University researchers found that people who exercise 150 minutes per week slept better and felt more alert during the day compared to those who don't. 35
- Researchers Guglielmo Beccuti and Silvana Pannain explain that recent epidemiological and laboratory evidence confirms previous findings of an association between sleep loss and an increased risk of obesity. Sleep loss has been shown to result in decreased insulin sensitivity, increased evening levels of cortisol (the stress hormone that prevents sleep), increased levels of ghrelin (increasing appetite), and decreased levels of leptin (reducing the feeling of satiation). They further explain that the worldwide prevalence of obesity has doubled since 1980, and this epidemic has been paralleled by a trend of reduced sleep. 36
- A 6-year Italian study found that every extra hour of sleep decreased the incidence of obesity by 30%. 36
- Lack of sleep can negatively affect eating habits. One study found an increased caloric intake in 12 normal-weight healthy adults after 4 hours of sleep. 37
- Another study reported a 14% increase in caloric intake, especially for carbohydrates in 10 healthy adults who had slept 4.5 hours. 38
Anxiety Disorders & Sleep Statistics
Sleep issues are very common with people with anxiety disorders and depression. Some anxiety disorders such as generalized anxiety disorder and post-traumatic stress disorder have even included nightmares or insomnia in their definitions.
Anxiety usually functions as an alarm bell for potential danger, but in anxiety disorders the alarms may be intense, frequent, or even continuous. This level of arousal leads to issues with sleep.
- 24% to 36% of insomnia sufferers have an anxiety disorder, while 27% to 42% of those with hypersomnia have anxiety disorders. 40
- In another study, researchers found that insomnia appeared before the anxiety disorder in 18% of the subjects. 38.6% of the time, insomnia and the anxiety disorder appeared around the same time. 43.5% of the time, anxiety appeared before insomnia. 40
- In a study published in the Archives of General Psychiatry, researchers found that 68% of subjects had difficulty falling asleep, while 77% had restless sleep. 41
Odds ratios for specific anxiety disorders associated with lifetime sleep disturbances (adapted from Breslau et al 39 ). 40
| Anxiety Disorder | Insomnia Alone | Hypersomnia Alone | Both |
|---|---|---|---|
| 7.0 (2.8-17.2) | 4.5 (1.5-15.3) | 4.8 (1.5-15.2) | |
| 5.3 (2.0-13.6) | 4.3 (1.3-14.8) | 8.5 (3.1-23.5) | |
| 5.4 (2.0-14.8) | 1.2 (0.1-9.7) | 13.1 (4.8-35.7) | |
| 1.5 (1.0-2.3) | 29 (1.8-4.8) | 4.0 (2.5-6.5) | |
| 2.4 (1.6-3.5)/td> | 3.3 (2.0-5.4) | 4.5 (2.8-3.7) |
- The majority of patients with panic disorder experience nocturnal panic attacks. Up to 18% of panic attacks happen while asleep. Ambulatory heart rate changes in patients with panic attacks. 42
- It's been estimated that 60% to 70% of patients had general anxiety disorder (GAD), suggesting that insomnia is one of the core facets of GAD. 43
- Sufferers of post-traumatic stress disorder (PTSD) commonly complain of nightmares and insomnia. It's been estimated that 96% of Holocaust survivors had insomnia and 83% had recurrent nightmares. 44
- One study found that PTSD sufferers estimate that they lay awake more than half of the night. 45
Depression and poor sleep occur so commonly together that researchers aren't sure if one is causing the other or if they're just associated. Both insomnia and sleeping too much could be signs of depression.
- It's estimated that 75% of patients with depression also have insomnia. 46
- According to the National Sleep Foundation , those with insomnia have a 10 times greater risk of developing depression than those with enough restful sleep.
- According to the journal Lancet Psychiatry , people with mental health disorders showed improvement from the increased amount and quality of sleep.
- Night owls are more likely to be depressed compared to early birds, and researchers aren't sure why.
- A Japanese study from 2006 analyzed data from 24,686 people aged 20 and above and found that people who sleep less than 6 hours and more than 8 hours tend to be depressed, creating a U-shaped association with symptoms of depression. 47
- Jones, Jeffrey. (December 19, 2013). https://news.gallup.com/poll/166553/less-recommended-amount-sleep.aspx
- American Academy of Pediatrics Endorsement of Childhood Sleep Guidelines. https://www.aap.org/en-us/about-the-aap/aap-press-room/pages/American-Academy-of-Pediatrics-Supports-Childhood-Sleep-Guidelines.aspx
- Burgard SA, Ailshire JA. Gender and Time for Sleep among U.S. Adults. Am Sociol Rev . 2013;78(1):51-69. doi:10.1177/0003122412472048
- Dr. Jim Horne. " Who REALLY needs more sleep - men or women? One of Britain's leading sleep experts says he has the answer." Daily Mail, January 26, 2010. https://www.dailymail.co.uk/health/article-1246029/Who-REALLY-needs-sleep--men-women-One-Britains-leading-sleep-experts-says-answer.html
- TIME Mobility Poll, in cooperation with Qualcomm. August 2012. https://www.qualcomm.com/media/documents/files/time-mobility-poll-in-cooperation-with-qualcomm.pdf
- Sleep Deprivation Can Threaten Competent Decision-making. American Academy of Sleep Medicine. May 5, 2007. https://www.sciencedaily.com/releases/2007/05/070501075246.htm
- Oxford University Press. https://academic.oup.com/journals
- Shift Work Sleep Disorder. https://my.clevelandclinic.org/health/diseases/12146-shift-work-sleep-disorder
- Gupta R, Das S, Gujar K, Mishra KK, Gaur N, Majid A. Clinical Practice Guidelines for Sleep Disorders. Indian J Psychiatry . 2017;59(Suppl 1):S116-S138. doi:10.4103/0019-5545.196978.
- Kessler RC, Berglund PA, Coulouvrat C, Hajak G, Roth T, Shahly V, Shillington AC, Stephenson JJ, Walsh JK. Insomnia and the performance of US workers: results from the America insomnia survey. Sleep . 2011 Sep 1;34(9):1161-71. doi: 10.5665/SLEEP.1230. Erratum in: Sleep. 2011;34(11):1608. Erratum in: Sleep. 2012 Jun;35(6):725.
- Kessler, R.C., Berglund, P.A., Coulouvrat, C., Hajak, G., Roth, T., Shahly, V., et al. (2011). "Insomnia and the performance of US workers: results from the America insomnia survey. https://www.ncbi.nlm.nih.gov/pubmed/21886353 34(9): 1161-1171.
- Deirdre Conroy, PH.D. (June 13, 2016). https://healthblog.uofmhealth.org/health-management/3-reasons-women-are-more-likely-to-have-insomnia
- Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med . 2007;3(5 Suppl):S7-S10.
- Billiard M., Dauvilliers Y. Narcolepsy In: Billiard M, ed. Sleep: Physiology Investigations and Medicine. New York, NY: Kluwer Academic/Plenum Publishers. 2003:403–406.
- Billiard M. Hypersomnias. In: Billiard M, ed. Sleep: Physiology Investigations and Medicine. New York, NY: Kluwer Academic/Plenum Publishers.
- Guilleminault C, Tilkian A, Dement WC. The sleep apnea syndromes. Annu Rev Med. 1976;27:465-84. doi: 10.1146/annurev.me.27.020176.002341.
- Weaver TE, George CFP, “Cognition and Performance in Patients with Obstructive Sleep Apnea,” in Kryger M, Roth T, Dement W (ed.), Principles and Practice of Sleep Medicine (5th Edition), St. Louis: Elsevier Saunders, 2011, pages 1194-1205.
- Mindell JA, Owens JA. Diagnosis and Management of Sleep Problems. A Clinical Guide to Pediatric Sleep. Philadelphia. PA: Lippincott Williams and Wilkins, 2003.
- Marcus CL. Pathophysiology of childhood obstructive sleep apnea: current concepts. Resp Physiol. 2000;119:143-154.
- Mansur A, Castillo PR, Rocha Cabrero F, et al. Restless Legs Syndrome. [Updated 2021 Apr 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430878/
- Thorpy MJ, Korman E, Spielman AJ, Glovinsky PB. Delayed sleep phase syndrome in adolescents. J Adolesc Health Care . 1988 Jan;9(1):22-7. doi: 10.1016/0197-0070(88)90014-9
- Saxvig IW, Pallesen S, Wilhelmsen-Langeland A, Molde H, Bjorvatn B. Prevalence and correlates of delayed sleep phase in high school students. Sleep Med . 2012 Feb;13(2):193-9. doi: 10.1016/j.sleep.2011.10.024.
- Paine SJ, Fink J, Gander PH, Warman GR. Identifying advanced and delayed sleep phase disorders in the general population: a national survey of New Zealand adults. Chronobiol Int. 2014 Jun;31(5):627-36. doi: 10.3109/07420528.2014.885036.
- Kurt S (December 2007). "IARC Monographs Programme finds cancer hazards associated with shiftwork, painting and firefighting" (Press release). International Agency for Research on Cancer.
- Lee ML, Howard ME, Horrey WJ, Liang Y, Anderson C, Shreeve MS, O'Brien CS, Czeisler CA. High risk of near-crash driving events following night-shift work. Proc Natl Acad Sci U S A . 2016 Jan 5;113(1):176-81. doi: 10.1073/pnas.1510383112.
- Division of Population Health. https://www.cdc.gov/NCCDPHP/dph/
- National Center for Chronic Disease Prevention and Health Promotion. https://www.cdc.gov/chronicdisease/
- Watson NF, Badr MS, Belenky G, et al.; Consensus Conference Panel. Joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep . 2015;38:1161–1183.
- Zhang X, Holt JB, Lu H, et al. Multilevel regression and poststratification for small area estimation of population health outcomes: a case study of chronic obstructive pulmonary disease prevalence using BRFSS. Am J Epidemiol. 2014;179(8):1025-1033.
- Paruthi S, Brooks LJ, D’Ambrosio C, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med . 2016;12(6):785–786.
- CDC - Data and Statistics. Short Sleep Duration Among US adults. https://www.cdc.gov/sleep/data_statistics.html
- Wheaton AG, Olsen EO, Miller GF, Croft JB. Sleep duration and injury-related risk behaviors among high school students — United States, 2007–2013. MMWR Morb Mortal Wkly Rep. 2016;65:337–341. https://www.cdc.gov/mmwr/volumes/65/wr/mm6513a1.htm
- "Sleep Health Index." SleepFoundation.org. 2018. https://www.sleepfoundation.org/shi
- Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med . 2004;1(3):e62. doi:10.1371/journal.pmed.0010062
- Godman, Heidi. "Losing Weight and Belly Fat Improves Sleep." Harvard Health Publishing, November 12, 2012, https://www.health.harvard.edu/blog/losing-weight-and-belly-fat-improves-sleep-201211145531
- Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care . 2011;14(4):402-412. doi:10.1097/MCO.0b013e3283479109
- Brondel L, Romer MA, Nougues PM, Touyarou P, Davenne D. Acute partial sleep deprivation increases food intake in healthy men. Am J Clin Nutr. 2010 Jun;91(6):1550-9. doi: 10.3945/ajcn.2009.28523.
- Tasali E, Broussard J, Day A, et al. Sleep curtailment in healthy young adults is associated with increased ad lib food intake [meeting abstract]. Sleep . 2009; 32 (Suppl):A163.
- Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry . 1996 Mar 15;39(6):411-8. doi: 10.1016/0006-3223(95)00188-3.
- Staner L. Sleep and anxiety disorders. Dialogues Clin Neurosci . 2003;5(3):249-258. doi:10.31887/DCNS.2003.5.3/lstaner.
- Sheehan DV, Ballenger J, Jacobsen G. Treatment of endogenous anxiety with phobic, hysterical, and hypochondriacal symptoms. Arch Gen Psychiatry . 1980 Jan;37(1):51-59. doi: 10.1001/archpsyc.1980.01780140053006.
- Taylor CB, Sheikh J, Agras WS, Roth WT, Margraf J, Ehlers A, Maddock RJ, Gossard D. Ambulatory heart rate changes in patients with panic attacks. Am J Psychiatry . 1986 Apr;143(4):478-82. doi: 10.1176/ajp.143.4.478.
- Ohayon MM. Prevalence of DSM-IV diagnostic criteria of insomnia: distinguishing insomnia related to mental disorders from sleep disorders. J Psychiatr Res . 1997; 31 :333–346.
- Kuch K, Cox BJ. Symptoms of PTSD in 124 survivors of the Holocaust. Am J Psychiatry. 1992 Mar;149(3):337-40. doi: 10.1176/ajp.149.3.337.
- Pillar G, Malhotra A, Lavie P. Post-traumatic stress disorder and sleep-what a nightmare! Sleep Med Rev. 2000 Apr;4(2):183-200. doi: 10.1053/smrv.1999.0095.
- Nutt D, Wilson S, Paterson L. Sleep disorders as core symptoms of depression. Dialogues Clin Neurosci . 2008;10(3):329-336. doi:10.31887/DCNS.2008.10.3/dnutt
- Kaneita Y, Ohida T, Uchiyama M, Takemura S, Kawahara K, Yokoyama E, Miyake T, Harano S, Suzuki K, Fujita T. The relationship between depression and sleep disturbances: a Japanese nationwide general population survey. J Clin Psychiatry. 2006 Feb;67(2):196-203. doi: 10.4088/jcp.v67n0204.
Related Content
Does Exercise Improve Sleep?
Published: March 22, 2023
Omega-3s for Better Sleep
Published: July 12, 2023
Sleep Disorders
Sleep Needs by Age and Gender
Published: February 22, 2023
Appointments at Mayo Clinic
- Adult health
How many hours of sleep are enough for good health?
The amount of sleep you need depends on various factors — especially your age. While sleep needs vary significantly among individuals, consider these general guidelines for different age groups:
| Age group | Recommended amount of sleep |
|---|---|
| Infants 4 months to 12 months | 12 to 16 hours per 24 hours, including naps |
| 1 to 2 years | 11 to 14 hours per 24 hours, including naps |
| 3 to 5 years | 10 to 13 hours per 24 hours, including naps |
| 6 to 12 years | 9 to 12 hours per 24 hours |
| 13 to 18 years | 8 to 10 hours per 24 hours |
| Adults | 7 or more hours a night |
In addition to age, other factors can affect how many hours of sleep you need. For example:
- Sleep quality. If your sleep is frequently interrupted, you're not getting quality sleep. The quality of your sleep is just as important as the quantity.
- Previous sleep deprivation. If you're sleep deprived, the amount of sleep you need increases.
- Pregnancy. Changes in hormone levels and physical discomfort can result in poor sleep quality.
- Aging. Older adults need about the same amount of sleep as younger adults. As you get older, however, your sleeping patterns might change. Older adults tend to sleep more lightly, take longer to start sleeping and sleep for shorter time spans than do younger adults. Older adults also tend to wake up multiple times during the night.
For kids, getting the recommended amount of sleep on a regular basis is linked with better health, including improved attention, behavior, learning, memory, the ability to control emotions, quality of life, and mental and physical health.
For adults, getting less than seven hours of sleep a night on a regular basis has been linked with poor health, including weight gain, having a body mass index of 30 or higher, diabetes, high blood pressure, heart disease, stroke, and depression.
If you're concerned about the amount of sleep you or your child is getting, talk to your doctor or your child's doctor.
Eric J. Olson, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Sleep and psoriatic arthritis
- Brain basics: Understanding sleep. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Understanding-Sleep. Accessed March 31, 2021.
- Paruthi S, et al. Recommended amount of sleep for pediatric populations: A consensus statement of the American Academy of Sleep Medicine. Journal of Clinical Sleep Medicine. 2016; doi.org/10.5664/jcsm.5866.
- Landon MB, et al., eds. Maternal physiology. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed March 31, 2021.
- Cirelli C. Insufficient sleep: Definition, epidemiology, and adverse outcomes. https://www.uptodate.com/contents/search. Accessed March 31, 2021.
- Kryger MH, et al., eds. Normal sleep. In: Atlas of Clinical Sleep Medicine. 2nd ed. Saunders Elsevier; 2014. https://www.clinicalkey.com. Accessed March 31, 2021.
- Watson NF, et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. 2015; doi.org/10.5664/jcsm.4758.
- Alzheimer's sleep problems
- Can psoriasis make it hard to sleep?
- Hidradenitis suppurativa and sleep: How to get more zzz's
- I have atopic dermatitis. How can I sleep better?
- Lack of sleep: Can it make you sick?
- Mayo Clinic Minute: Meditation is good medicine
- Mayo Clinic Minute: Sleep Spoiler - Tips for a Good Night's Rest
- Melatonin side effects
- Napping do's and don'ts
- Prescription sleeping pills: What's right for you?
- Antihistamines for insomnia
- OTC sleep aids
- Sleeping positions that reduce back pain
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Expert Answers
- How many hours of sleep are enough
Help transform healthcare
Your donation can make a difference in the future of healthcare. Give now to support Mayo Clinic's research.
- ABOUT THE PROJECT
- ONGOING PROJECTS
- PUBLICATIONS
- SURVEY METHODS
- SPOTLIGHT ON:
- DRUGS AND ALCOHOL
- PHYSICAL ACTIVITY
- SEDENTARY BEHAVIOR
- SEE ALL FINDINGS
- WOMEN’S FINANCIAL SECURITY
- HOME OWNERSHIP
- EMERGENCY FUNDS
- HEALTH INSURANCE
- INVESTMENTS
- LIFE INSURANCE
- LONG TERM CARE
- VOLUNTEERISM
- CIVIC ENGAGEMENT
- RELIGIOUS ORGANIZATIONS
- WORKING FOR PAY
- AFFILIATE INTERVIEWS
- DIRECTORS’ BLOG POSTS
- EXPERT PERSPECTIVES
- PERSONAL PERSPECTIVES
- STANFORD CENTER ON LONGEVITY >
- Research Update on Diet
- Research Update on Sleep
Research Update 1
By Marie Conley Smith
I n a world full of opportunities, stressors, inequalities, and distractions, maintaining a healthy lifestyle can be challenging, and sleep is often the first habit to suffer. Good sleep hygiene is a huge commitment: it takes up about a third of the day, every day, and works best when kept on a consistent schedule. It does not help that the primary short-term symptoms of insufficient sleep can be self-medicated away with caffeine. However, the effects of sleep loss can range from inconvenient to downright dangerous; people have trouble learning and being productive, take risks more readily, and are more likely to get into accidents. These effects also last longer than it takes to get them, as recovering from each night of poor sleep takes multiple days. When it comes to sleep, every night counts. In this update, we will discuss what Stanford researchers have to say about sleep and why we need it, who is getting too little of it, and some of the latest findings that may help us sleep better.
We have not cracked the code on sleep
Despite this progress, scientists have not been able to crack the code of why sleep is critical to brain function. There is also little consensus about how sleep stages actually affect quality of sleep and how they affect us when we are awake.
Part of the challenge of cracking the code on sleep is how difficult it is to study. The gold standard of sleep study, polysomnography, developed by Dement in the 1960s, 1 is the most reliable tool for measuring many sleep characteristics and detecting sleep disorders such as obstructive sleep apnea and narcolepsy. However, it is expensive and time-consuming to run, which means that usually only a night or two is recorded. This snapshot of sleep may not reflect what normally occurs for a given person, and makes it difficult to draw conclusions about their behavior and performance in the days surrounding the sleep measurement.
The recent explosion in consumer wearable devices is a promising trend for researchers because of their potential to measure thousands of people’s sleep in their natural environments. They have not yet been widely adopted as measurement tools by scientists, however, as it is unclear if they provide the level of precision and measurement consistency required for a scientific study. Researchers at Stanford have called for these devices to be cleared by the FDA before using them to assign a diagnosis. 2 The “holy grail” would be a wearable device that could track sleep accurately while also providing performance information about the rest of the day, which would allow researchers to recognize more nuanced relationships between how people sleep and how it affects their lives.

The short- and long-term effects of insufficient sleep
We all know anecdotally what it is like to get too little sleep; it might be described with words and phrases like “tired,” “cranky,” “sluggish,” and “need caffeine.” Review of the scientific literature reveals how wide-ranging these effects can be. With too little sleep, people have a harder time learning 3 and concentrating, and are more likely to take risks. 4,5 The likelihood of getting into an auto accident increases. 6 Sleep deprivation has a bidirectional relationship with depression, 7,8 in that insomnia often both precedes and follows a depressive episode. Short sleep also interferes with other Healthy Living behaviors: people are more likely to crave sweet and fatty foods 9 and to choose foods that are calorically dense, 10 are more prone to injury during exercise, 11 and have an increased risk of obesity. 12
Sleep deprivation can even affect mundane daily activities. In 2017, then Stanford PhD candidate Tim Althoff and Professor Jamie Zeitzer of the Stanford Center for Sleep Sciences and Medicine took up the sleep measurement challenge by collaborating with Microsoft Research to examine the effects of sleep deprivation through a common daily activity: using an online search engine. 13 They paired users’ Microsoft Band sleep data with their Bing searches among users who had agreed to share their activity for study. By linking quantity and timing of sleep with typing speed during the searches, they were able to draw a number of conclusions about how sleep quality affects performance.
In this study, the researchers captured the sleep duration and search engine interactions of over 31,000 people. The researchers measured the amount of time between keystrokes as people typed their search engine entries, and used this as a measure of daily performance (that is, how well people did after a night of sleep). They were able to track the people who had multiple nights of insufficient sleep (defined as 6 hours of sleep or fewer) to see if their typing speed changed. They found that, on average, one night of insufficient sleep resulted in worse performance for three days, and two nights of insufficient sleep negatively impacted performance for six days. In other words, it took people almost an entire week to recover their performance after two consecutive nights of insufficient sleep. The implication is that the impact of sleep loss can persist for days.
Recent Stanford solutions for better sleep
Ongoing research at Stanford has led both to treatments for sleep disorders and to recommendations for best sleep practices for the public.

There are a few clinics and organizations that offer CBTI remotely in an effort to give more people access. There are apps such as SleepRate , which features content designed by Stanford researchers, Somryst , which was recently approved by the FDA, and Sleepio , which is offered by several large employers as an employee benefit. The Cleveland Sleep Clinic offers a 6-week online program called “ Go! to Sleep ,” and the U.S. Department of Veterans Affairs offers one of the same duration called “ Path to Better Sleep .” A physician should be consulted before starting any of these programs to ensure there are not any underlying disorders that need to be addressed.
Ultrashort light flash therapy Professor Jamie Zeitzer was interested in helping people who had a hard time sleeping because their circadian rhythm was not in sync with their desired sleep schedule. He discovered that ultrashort bursts of light directed into a person’s closed eyes while they were sleeping was very effective at shifting the time a person starts getting sleepy. Sleep doctors had already been using continuous light to help people reset their internal clock while they were awake; this new short-flash method shows great promise not only because of its effectiveness, but because it can be administered passively while people are sleeping. The approach involves wearing a sleep mask that emits the bright flashes and has been shown to only wake individuals who are particularly sensitive to light.

Lumos Sleep Mask
Professor Zeitzer and his team administered these ultrashort light flashes to teenagers, whose natural circadian systems have shifted so that their sleep and wake times are considerably later than children or adults. The time structure of our society, and schools in particular, does not take this into account. Professor Zeitzer administered the light flashes to see if it would help teens go to bed earlier. 20 They found that, while the teenagers were getting sleepy earlier, the light flashes alone were not enough to get the teenagers to bed earlier. With a second group of teens, they combined the light therapy with cognitive behavioral therapy (CBT) sessions. The CBT sessions served to inform the teens about sleep health and hygiene and helped them schedule their activities to allow for their desired sleep hours. After this combined therapy trial, the teens went to bed an average of 50 minutes earlier, getting an average of 43 more minutes of sleep per night. The researchers found the CBT component to be integral to behavior change – without the added education and support, the teens were not motivated enough to change their behavior and would simply push past their sleepiness.
This ultrashort light flash therapy can be used by anyone who may want to shift their sleep schedule; for example, to rebound from jet lag or to cope with a consistent graveyard shift at work. There is no evidence that other groups would require accompanying CBT like the teens, as long as they are self-motivated to change their sleep schedule. Zeitzer plans to test this technology next with older adults who wish to push their sleep time later. A company has spun out of this work, which Zeitzer advises but in which he has no financial interest, called Lumos . They are currently developing their product, and are hoping to make this intervention widely available.
Data Spotlight on: Black Americans

While most Americans have seen improvements in sleep over the past decade, Black Americans continue to sleep significantly less than other groups. This trend has been examined both by researchers and the popular press. 21,22 Researchers have found that Black Americans, in addition to getting shorter sleep, are also more likely to get poor quality sleep – spending less time in the most restorative stages of sleep 23,24 – and to develop obstructive sleep apnea. 25 Black Americans are also disproportionately affected by diseases that have been associated with poor sleep, such as obesity, diabetes, 26 and cardiovascular disease. 25
The exact reason(s) for Black Americans’ poor sleep is still unclear, though researchers have proposed potential contributing factors, largely related to the social inequality Black Americans face in the U.S.:
Experiences of discrimination : the stress of racial discrimination has been associated with spending lesstime in deep sleep and more time in light sleep among Black Americans. 24
Living environment : neighborhood quality has been linked to sleep quality, 27 and Stanford researchersfound that racial and income disparities persist in neighborhoods. 28 They found that while middle-income white families are more likely to live in resource-rich neighborhoods with other middle-income families, middle-income black families tend to live in markedly lower-income, resource-poorneighborhoods.
Work and income inequality : for example, shift work can cause irregular working hours. This leadspeople to suffer “social jetlag,”; a discrepancy in sleep hours between work and free days, 29 leading tosymptoms of sleep deprivation.
Lack of access to resources : particularly sleep-related healthcare and education.
Some of these factors are being addressed directly. Professor Girardin Jean-Louis from New York University and his team have devoted themselves to addressing the access to healthcare and education issue among local black communities in New York by tailoring online materials about obstructive sleep apnea to the culture, language, and barriers of specific communities. 30 Professor Jamie Zeitzer and his team at Stanford recently completed an initial clinical trial of a drug (suvorexant), which was found to help people who work at night get three more hours of sleep during the day. 31 Professor Zeitzer’s ultrashort light flash therapy (discussed above) may also help with shift work. These interventions could help to improve sleep for Black Americans, but they may not make up the whole picture; it could be that the underlying social inequality needs to be addressed in order to fully close the sleep gap.
Thanks to Jamie Zeitzer and Ken Smith for their insights and edits on this report.
- Deak, M., & Epstein, L. J. (2009). The history of polysomnography. Sleep Medicine Clinics , 4 (3), 313–321.
- Cheung, J., Zeitzer, J. M., Lu, H., & Mignot, E. (2018). Validation of minute-to-minute scoring for sleep and wake periods in a consumer wearable device compared to an actigraphy device. Sleep Science and Practice , 2 (1), 11. https://doi.org/10.1186/s41606-018-0029-8
- Gao, C., Terlizzese, T., & Scullin, M. K. (2019). Short sleep and late bedtimes are detrimental to educational learning and knowledge transfer: An investigation of individual differences in susceptibility. Chronobiology International , 36 (3), 307–318. https://doi.org/10.1080/07420528.2018.1539401
- O’Brien, E. M., & Mindell, J. A. (2005). Sleep and risk-taking behavior in adolescents. Behavioral Sleep Medicine , 3 (3), 113–133. https://doi.org/10.1207/s15402010bsm0303_1
- Rusnac, N., Spitzenstetter, F., & Tassi, P. (2019). Chronic sleep loss and risk-taking behavior: Does the origin of sleep loss matter? Behavioral Sleep Medicine , 17 (6), 729–739. https://doi.org/10.1080/15402002.2018.1483368
- Bioulac, S., Micoulaud-Franchi, J.-A., Arnaud, M., Sagaspe, P., Moore, N., Salvo, F., & Philip, P. (2017). Risk of motor vehicle accidents related to sleepiness at the wheel: A systematic review and meta-analysis. Sleep , 40 (10). https://doi.org/10.1093/sleep/zsx134
- Franzen, P. L., & Buysse, D. J. (2008). Sleep disturbances and depression: Risk relationships for subsequent depression and therapeutic implications. Dialogues in Clinical Neuroscience , 10 (4), 473–481.
- Tsuno, N., & Ritchie, K. (2005). Sleep and Depression. The Journal of Clinical Psychiatry , 16.
- Lv, W., Finlayson, G., & Dando, R. (2018). Sleep, food cravings and taste. Appetite , 125 , 210–216. https://doi.org/10.1016/j.appet.2018.02.013
- Pardi, D., Buman, M., Black, J., Lammers, G. J., & Zeitzer, J. M. (2017). Eating decisions based on alertness levels after a single night of sleep manipulation: A randomized clinical trial. Sleep , 40 (2). https://doi.org/10.1093/sleep/zsw039
- Chennaoui, M., Arnal, P. J., Sauvet, F., & Léger, D. (2015). Sleep and exercise: A reciprocal issue? Sleep Medicine Reviews , 20 , 59–72. https://doi.org/10.1016/j.smrv.2014.06.008
- Cappuccio, F. P., Taggart, F. M., Kandala, N. B., Currie, A., Peile, E., Stranges, S., & Miller, M. A. (2008). Meta-analysis of short sleep duration and obesity in children and adults. Sleep , 31 (5), 619-626.
- Althoff, T., Horvitz, E., White, R. W., & Zeitzer, J. (2017, April). Harnessing the web for population-scale physiological sensing: A case study of sleep and performance. In Proceedings of the 26th international conference on World Wide Web (pp. 113-122).
- Roth, T. (2007). Insomnia: Definition, prevalence, etiology, and consequences. Journal of Clinical Sleep Medicine , 3 (5 Suppl), S7–S10.
- Qaseem, A., Kansagara, D., Forciea, M. A., Cooke, M., & Denberg, T. D. (2016). Management of chronic insomnia disorder in adults: A clinical practice guideline from the American College of Physicians. Annals of Internal Medicine , 165 (2), 125–133. https://doi.org/10.7326/M15-2175
- Jacobs, G. D., Pace-Schott, E. F., Stickgold, R., & Otto, M. W. (2004). Cognitive behavior therapy and pharmacotherapy for insomnia: A randomized controlled trial and direct comparison. Archives of Internal Medicine , 164 (17), 1888–1896. https://doi.org/10.1001/archinte.164.17.1888
- Manber, R., Bei, B., Simpson, N., Asarnow, L., Rangel, E., Sit, A., & Lyell, D. (2019). Cognitive behavioral therapy for prenatal insomnia: A randomized controlled trial. Obstetrics & Gynecology , 133 (5), 911–919. https://doi.org/10.1097/AOG.0000000000003216
- Ong, J. C., Crawford, M. R., Dawson, S. C., Fogg, L. F., Turner, A. D., Wyatt, J. K., Crisostomo, M. I., Chhangani, B. S., Kushida, C. A., Edinger, J. D., Abbott, S. M., Malkani, R. G., Attarian, H. P., & Zee, P. C. (2020). A randomized controlled trial of CBT-I and PAP for obstructive sleep apnea and comorbid insomnia: Main outcomes from the MATRICS study. Sleep . https://doi.org/10.1093/sleep/zsaa041
- Karlin, B. E., Trockel, M., Taylor, C. B., Gimeno, J., & Manber, R. (20130415). National dissemination of cognitive behavioral therapy for insomnia in veterans: Therapist- and patient-level outcomes. Journal of Consulting and Clinical Psychology , 81 (5), 912. https://doi.org/10.1037/a0032554
- Kaplan, K. A., Mashash, M., Williams, R., Batchelder, H., Starr-Glass, L., & Zeitzer, J. M. (2019). Effect of light flashes vs sham therapy during sleep with adjunct cognitive behavioral therapy on sleep quality among adolescents: A randomized clinical trial. JAMA Network Open , 2 (9), e1911944. https://doi.org/10.1001/jamanetworkopen.2019.11944
- Resnick, B. (2015, October 27). The Racial Inequality of Sleep . The Atlantic. https://www.theatlantic.com/health/archive/2015/10/the-sleep-gap-and-racial-inequality/412405/
- Resnick, B., & Barton, G. (2018, April 12). Black Americans don’t sleep as well as white Americans. That’s a problem. Vox. https://www.vox.com/science-and-health/2018/4/12/17224328/sleep-gap-black-white-minority-america-health-consequences
- Beatty, D. L., Hall, M. H., Kamarck, T. A., Buysse, D. J., Owens, J. F., Reis, S. E., Mezick, E. J., Strollo, P. J., & Matthews, K. A. (2011). Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh SleepSCORE project. Health Psychology , 30 (3), 351–359. https://doi.org/10.1037/a0022976
- Tomfohr, L., Pung, M. A., Edwards, K. M., & Dimsdale, J. E. (2012). Racial differences in sleep architecture: The role of ethnic discrimination. Biological Psychology , 89 (1), 34–38. https://doi.org/10.1016/j.biopsycho.2011.09.002
- Olafiranye, O., Akinboboye, O., Mitchell, J., Ogedegbe, G., & Jean-Louis, G. (2013). Obstructive sleep apnea and cardiovascular disease in blacks: A call to action from association of black cardiologists. American Heart Journal , 165 (4), 468–476. https://doi.org/10.1016/j.ahj.2012.12.018
- Jackson, C. L., Redline, S., Kawachi, I., & Hu, F. B. (2013). Association between sleep duration and diabetes in black and white adults. Diabetes Care , 36 (11), 3557–3565. https://doi.org/10.2337/dc13-0777
- Hale, L., Hill, T. D., & Burdette, A. M. (2010). Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Preventive Medicine , 51 (3–4), 275–278. https://doi.org/10.1016/j.ypmed.2010.06.017
- Reardon, S. F., Fox, L., & Townsend, J. (2015). Neighborhood income composition by household race and income, 1990–2009. The ANNALS of the American Academy of Political and Social Science , 660 (1), 78–97. https://doi.org/10.1177/0002716215576104
- Wittmann, M., Dinich, J., Merrow, M., & Roenneberg, T. (2006). Social jetlag: Misalignment of biological and social time. Chronobiology International , 23 (1–2), 497–509. https://doi.org/10.1080/07420520500545979
- Jean-Louis, G., Robbins, R., Williams, N. J., Allegrante, J. P., Rapoport, D. M., Cohall, A., & Ogedegbe, G. (2020). Tailored Approach to Sleep Health Education (TASHE): A randomized controlled trial of a web-based application. Journal of Clinical Sleep Medicine . https://doi.org/10.5664/jcsm.8510
- Zeitzer, J. M., Joyce, D. S., McBean, A., Quevedo, Y. L., Hernandez, B., & Holty, J.-E. (2020). Effect of suvorexant vs placebo on total daytime sleep hours in shift workers: A randomized clinical trial. JAMA Network Open , 3 (6), e206614. https://doi.org/10.1001/jamanetworkopen.2020.6614
News & Articles
How much sleep do you really need.
October 1, 2020 / Sleep and You
Getting enough sleep is doable and important for your health. Read on for how many hours to strive for at every age.
Sleep is essential to feeling rested and alert. Getting the right amount for your mind and body feels great and helps you wake up feeling refreshed and ready to go. Every person is different when it comes to the exact amount of sleep that’s optimal for them, but most people fall within a range, depending on their age. These guidelines can help you determine how much sleep you really need, while providing some easy ways to achieve it.
How Many Hours of Sleep Do You Need?
There is no precise number of minutes or hours of sleep at night that guarantees you will wake up feeling totally refreshed. But based on your age and lifestyle, what’s recommended for you likely falls within a certain range. To help yourself stay alert during the day, try sticking with these guidelines.
Newborns: From 0-3 months, babies need between 14 and 17 hours of sleep. This includes daytime naps, since newborns rarely sleep through the night. Older infants (4-11 months) need about 12 to 15 hours of sleep each day.
Toddlers: Between the first and second year of life, toddlers need between 11 and 14 hours of sleep each night.
Children: Preschoolers (3-5 years) should get 10 to 13 hours, while school-age kids (6-13 years) should strive for nine to 11 hours each night.
Teenagers: As kids get older, their need for sleep decreases slightly. Teens (14-17 years) require about eight to 10 hours of nightly sleep.
Adults: Between the ages of 18 and 64, adults should aim for seven to nine hours of nightly sleep. If you’re older than 65, you may need a little less: seven to eight hours is recommended.
Build in Some Flex Time
Some people can function well on the lower end of the range and others will need every minute of the upper limit. In fact, an additional hour or two on either side of a given range may be appropriate, depending on the person. Still, straying too far from the recommended amount could lead to a variety of health issues. For example, shortchanging sleep has been associated with weight gain, reduced immunity, high blood pressure, and depression.
The negative effects of too little or too much sleep aren’t just physical—they can also interfere with your mental health. Your outlook, mood, and attention span all depend on getting the right amount of sleep, and without it, your job performance (not to mention your personal life) can suffer.
Easy Ways to Get More Sleep
If getting enough sleep seems like an uphill battle, there are a few tips you can try. To start, head to bed at the same time every night, to allow your body to settle into a regular sleep-wake schedule. Just the way kids benefit from a set schedule, adults who stick to a regular pre-sleep routine that includes reading, meditation, journaling, and a warm bath may find it easier to wind down in the evening.
To help get quality sleep, avoid alcohol, caffeine, and spicy and fried foods right before bedtime. Aim for a bedroom temperature between 60 and 67 °F , make sure it’s dark, and block any bothersome noises with a pair of earplugs. For a fuller list of sleep tips, read them here .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Curr Health Sci J
- v.43(1); Jan-Mar 2017
Research on Sleep Quality and the Factors Affecting the Sleep Quality of the Nursing Students
1 Uludag University Faculty of Health Sciences, Bursa, Turkey
F. TANRIKULU
2 Sakarya University Faculty of Health Sciences, Sakarya, Turkey
Purpose: This research has been conducted in order to examine the quality of sleep and the factors affecting the sleep quality.Material/Methods: The sample of this descriptive research is comprised of 223 volunteer students studying at Uludağ University Faculty of Health Sciences Department of Nursing. Research datas have been collected through personal features survey and Pittsburg Sleep Quality Index(PSQI). Results: The average result derived from the sample is 6.52±3.17. To briefly explain the average of the component scores: subjective sleep quality 1.29±0.76, sleep latency 1,55±0.94, sleep duration 0.78±0.99, habitual sleep activity 0.47±0.90, sleep disturbances 0.99±0.09, use of sleeping medication 0.12±0.48, daytime dysfunction 1.29±0.90. It has been observed that there is a meaningful discrepancies between average PSQI results and smoking habits of the students, total daily sleeping hours, efficient waking up times, average daily coffee consumption(p<0.05). According to the analyses there is no meaningful discrepancies between the age,gender, where the students live,snoozing during the morning classes, the existence of chronic diseases and daily average tea consumption.(p>0.05)Conclusions: According to the findings in the light of this research; nursing students have low sleep quality.
Introduction
Sleep, which is directly related to health and quality of life, is a basic need for a human being to continue his bio-psycho-social and cultural functions [ 1 ]. Sleep affects the quality of life and health,which is also perceived as an important variable[ 2 , 3 ]. Feeling energetic and fit after sleeping is descriped as the sleep quality [ 4 ]. The fact that, nowadays the complaints about sleep disorder being prevalent, low sleep quality being an indicator of many medical diseases and there is strong relationship between physical ,psychological wellness and sleep; sleep quality is an important concept in the clinic practices and related researches on sleep [ 5 ].
Sleeping disorders is a common health problem among adolescants and young adults [ 6 ]. There is a general belief that university students do not sleep enough [ 7 ]. It has been reported that the the amount and the quality of the sleep of university students has been changed in past few decades and the sleep disorders has been inclined [ 8 ]. In the related researches is found that sleeping disorder among university students in various frequencies and amounts [ 9 , 10 , 11 ]. Low quality of sleep harms not only the academic success but also behavioral and emotional problems [ 12 ], negative emotional status, increase in alcohol and smoking habits[ 13 , 14 ]. In another research, it has been found that, there is a link between sleep quality and pschological wellbeing; more psychological diseases are observed among university students with low sleep quality [ 15 ]. Additionally it is recorded in the medical literature that, sleep quality is affected from the external factors such as gender, academic success, academic background, general health, socio-economic status and the stress level of the person [ 1 , 4 , 7 , 16 ].
Nursing students may have sleep issues due to their program being though, time and effort-requiring [ 3 , 11 ]. Because of this matter, students who cannot sleep enough may have various physical,social, psychological problems. Therefore, it is much more important to indicate the sleep quality of the students and the factors affecting. There is a demand for this kind of research since there is only limited amount of related research
Aim of Study
This research is conducted in order to examine the sleep quality of the Nursing students and the factors affecting it.
Material and Method
The research sample of this descriptive and cross-sectional research is derived from the population of students studying at Uludag University Faculty of Health Sciences Department of Nursing in the Spring Semester of 2016-2017 academic year (N=450). The sample of the research is 223 volunteer students.
In the research data collection process, personal features survey and Pittsburg Sleep Quality Index(PSQI) has been used. Survey,which is prepared by the researchers scanning the related medical literature, comprises of 11 survey questions. These questions are aimed to indicate the introductory information of the students and the varibles affecting the sleep quality(age, gender, semester, aree of residence, existence of chronic diseases, caffeine consumption level, smoking habits).
Pittsburg Sleep Quality Index(PSQI) usef for examination of the sleep quality of the students; is a scale which assesses the sleep quality and the sleeping disorder in the last one month. Pittsburg Sleep Quality Index (PSQI) is devised by the Buysee et al. [ 17 ] is adapted to Turkish by the Agargun et al. [ 18 ] and internal consistency coefficient is calculated as 0.80. In the examination process of PSQI,19 issues are scored. PSQI has 7 internal components such as subjective sleep quality, duration of sleep, habitual sleeping activity, sleep disturbance, sleep delay, use of sleeping drugs and daytime dysfunctions. Each component is scored between 0-3. Total score varies between 0-21, total PSQI score being <5 shows high sleep quality, >5 indicates low sleep quality [ 18 ].
Statistical Analysis
In the data assessment process; frequency, percentage, arithmetic average and Cronbach’s alpha is measured. The total score average of the sample was calculated and the normality test was applied to determine the normal distribution of the sample scores According to this analysis, it is observed that the sample scores does not comply with the normal distribution(Kolmogorov-Smirnov Z=0.143, p<0.05);nonparametric tests such as Mann-Whitney U and Kruskall Wallis were used to examine the difference between the independent variables and sample averages.Scores are provided as average±standard deviation and p<0.05 is considered as statistically meaningful results
Ethical Concerns
For the use of the assessment, written permissions are taken via e-mail. For the purpose of the conduct of the survey, written approval from the research commission of the related institution is taken(Decision no: 2017/7). Before application and the approval was obtained from them, students were informed about the research and data collection tools.
According to the research, average age of the stundets is 20.03±1,73, 68,6% of them are women. 50.2% of the students are in I. year, 19.7% are in II. year, 18.4% in III. year,%11.7 of them are in IV. year. 17% of the students have smoking habits, 56.5% of the sleep 6-7 hours per day. 26% of the students consumes 4-7 cups of tea per day, 19.3% of them uses 2-3 cups of coffee, 46.6% of them wake up energetic after sleep, 19.9% of them have no chronic disease, 41.3% of them snooze during morning lectures.
The total PSQI average of the students is calculated as 6.52±3.17 and the ratio of the students with sleep quality average higher than 5 is 56.1%.(Table 56.1%.(Table1, 1 , Table Table2) 2 ) The students internal component score averages are given below: subjective sleep quality 1.29±0.76, sleep latency 1,55±0,94, sleep duration 0.78±0.99, habitual sleep activity 0.47±0.9, sleep disturbances 0.99±0.09, sleeping drug use 0.12±0.48 and daytime dysfunctions 1.29±0.9(Table 1 )
PSQI total and internal component score averages of the sample
| PSQI Components | X ±SS |
| Subjective Sleep Quality | 1.29 ±0.76 |
| Sleep Latency | 1.55 ± 0.94 |
| Sleep Duration | 0.78 ± 0.99 |
| Habitual Sleeping Activity | 0.47 ± 0.90 |
| Sleep Disturbances | 0.99 ± 0.09 |
| Sleeping Drug Usage | 0.12 ± 0.48 |
| Daytime Dysfunctions | 1.29 ± 0.90 |
| Total PSQI | 6.52 ±3.17 |
PSQIscore averages of the sample
| n | % | |
| 5 and below | 98 | 43.9 |
| above 5 | 125 | 56.1 |
Although total PSQI score average being above 5, only 56.1% of the students' PSQI averages were above 5.According to this result nearly half of the students’ sleep quality can be considered as low sleep quality (Table (Table2 2 ).
In Table Table3 3 personal features of the nursing stdents, the relationship between these features and PSQI scores. According to the table,a statistically meaningful relationship between PSQI score averages amd smoking habit, total daily sleeping hours, waking up energetic and daily average coffee consumption(p<0.05); no meaningful relationship is found between PSQI scores and age, gender, semester level, area of residence, preexistence of chronic diseases, snoozing during morning lectures, daily average tea consumption(p>0.05)
>Table 3. Personal feature distribution of the sample students and the relationship between personal features and PSQI scores (n:223)
| Personal Features | n | % | Test Results |
| Gender | U*=1.36 | ||
| Male | 70 | 31.4 | p=0.174 |
| Female | 153 | 68.6 | |
| Age (Gender) | 20.03±1.73 | r **=0.094 | |
| p=0.160 | |||
| Semester Year | |||
| 1.Year | 112 | 50.2 | |
| 2.Year | 44 | 19.7 | KW***=6.050 |
| 3.Year | 41 | 18.4 | p=0.109 |
| 4.Year | 26 | 11.7 | |
| Area of Residence | |||
| With Family | 65 | 29.1 | KW***=3.58 |
| İn Dormitory | 120 | 53.8 | p=0.310 |
| Alone at Home | 10 | 4.5 | |
| Sharing flat | 28 | 12.6 | |
| Preexistence of Chronic Diseases | |||
| Yes | 18 | 8.1 | U*=1.21 |
| No | 205 | 91.9 | p=0.226 |
| Smoking Habits | |||
| Smoking | 38 | 17 | U*=2.54 |
| Non-smoking | 185 | 83 | p=0.011 |
| Snoozing during the Lecture Hours | |||
| Yes | 92 | 41.3 | KW***=1.59 |
| No | 35 | 15.7 | p=0.45 |
| Sometimes | 96 | 43 | |
| Waking Up Energetic | |||
| Yes | 29 | 13 | KW***=26.43 |
| No | 90 | 40.4 | p=0.00 |
| Sometimes | 104 | 46.6 | |
| Total Sleeping Hours | |||
| 4-5 hours | 29 | 13 | KW***=40.06 |
| 6-7 hours | 126 | 56.5 | p=0.000 |
| 8-9 hours | 57 | 25.6 | |
| 9 hours and above | 11 | 4.9 | |
| Tea Consumption | KW***=2.92 | ||
| 0-3 cups | 151 | 67.7 | p=0.231 |
| 4-7 cups | 58 | 26 | |
| 8 cups and above | 14 | 6.3 | |
| Coffee consumption | KW***=10.75 | ||
| 0-1 Cup | 172 | 77.1 | p=0.005 |
| 2-3 Cup | 43 | 19.3 | |
| 4 Cups and above | 83 | 3.6 | |
*Mann Whitney U Analysis
**Correlation Analysis
***Kruskal Wallis Analysis
According to the results of this research which we conducted in order examine the affecting nursing students’ sleep quality and the factors affecting; 56.1% of the students have PSQI average of 5 and lower. In the light of this research, we can infer that more than half of the students have low sleep quality.In a similar research in the United States of America, it is observed than 71% of the students have at least one sleeping disorder [ 19 ]. According to a similar research conducted by Karatay and colleagues [ 4 ] 56% of the nursing students have low sleep. According to Aysan and colleagues’ research [ 3 ] students with sleep quality scores higher than 5 comprises 59% of the sample. Similar research in the medical literature points out that university students have low quality of sleep [ 10 , 16 , 20 , 21 , 22 , 23 ]. Our research results justifies the results of researches given above. It is understood from the results of our research that low sleep quality is an important issue for the nursing students. Extraordinarly apart from our research, according to some similar researches conducted in Turkey less than half of the university students studying in Turkey have sleeping disorders [ 14 , 16 ]. We interpret that, this difference may be caused by the choice of a different sample of students.
According to the results of the study, there was a significant difference between students' sleep quality and smoking habits, total sleep hours, resting status in the morning and average daily coffee consumption (Table (Table3). 3 ). It is reported that sleeping is important in terms of the health of young adults [ 3 ] and it is said that young people need sleep for an average of 9-10 hours per [ 4 , 24 ]. In this study, students who wake up well-rested and sleeping 6-7 hours per day have higher sleep quality.These findings also supports the medical literature.According to Karatay et al. [ 4 ], Sari et al. [ 14 ] and Vail-Smith and colleagues’ [ 8 ] studies,smoking students have lower sleep quality compared to non-smokers.It is known that cigarette contains nicotine which has stimulant effect and it is known that smoking before sleep especially makes it difficult to fall asleep and affects sleep quality negatively. On the other side according to Shcao et al. [ 25 caffeine containing drinks harms sleep quality. Our study also show parallelism with these findings.
According to the results of this research, it is found that there was no relation between the sleep quality and the age, sex, class level, area of residence, sleepiness in morning classes, presence of chronic diseases and average daily tea consumption (Table (Table3). 3 ). Age and gender have been found to be among the factors that may affect sleep quality of individuals, though some studies have shown that some factors such as age, gender, class level and place of residence do not affect sleep quality [ 3 , 16 ]. In this study, it is interpreted that the age factor to be ineffective in sleep quality may be caused by the are in a similar age group.According to researches examining the correlation between gender and sleep quality, females have lower sleep quality than males [ 3 , 5 , 7 ]. Additionally, first year students’ sleep quality may be harmed by these factors; such as their first year curriculum being though, being deprived of family attention, adaptation efforts for a new social environment.Furthermore, considering that the environmental factor on sleep quality is also very effective, it can be assumed that the students living in dormitory stay more crowded rooms and the sleep quality is lower than the other students.Consequently, our research does not justify the medical literature.
Lund and colleagues[ 26 ] pointed out that physical and psychological problems have negative effects of sleep quality.In our study, it is observed that preexistence of chronic diseases does not effect sleep quality. In Saygili and colleagues’ research [ 16 ] students with chronic diseases have lower sleep quality. Sari and colleagues [ 14 ] showed that students confirming to have chronic illnesses have lower sleep quality but this result does not reflect a statistically meaningful relationship between sleep quality and existence of a chronic disease.It is known that chronic diseases related to the respiratory system, especially asthma, are frequently caused by sleep problems and affect sleep quality negatively [ 16 ]. The results are not consistent with the literature due to the fact that students who included in the study have declared illnesses which have ambiguous relationship with the sleep quality; since the variety of the chronic diseases are not questioned in this research.
According to the findings in the light of this research; nursing students have low sleep quality. Additionally, students who do not smoke, sleeps 6-7 hours per day and consuming beverages with caffeine less have a better quality of sleep.To raise awaeness among university students and about the concept of sleep quality and the factors affecting the sleep quality and to increase the quality of sleep quality; panel discussions,seminars and conferences focusing on the relationship between alcohol/caffeine consumption, smoking and the quality of sleep are suggested.
Acknowledgments
All authors had equal contribution
Individual Circadian Clocks Might Be the Next Frontier of Personalized Medicine

F or as long as Seemay Chou can remember, she has gone to bed at midnight and woken around 4:30 a.m. Chou long assumed that meant she was a bad sleeper. Not that she felt bad. In fact, sleeping just four hours a night left her feeling full of energy and with free time to get more done at her job leading a research lab that studies bacteria. “It feels really good for me to sleep four hours,” she says. “When I’m in that rhythm, that’s when I feel my best.”
Still, in an effort to match the slumber schedules of the rest of the world, she would sometimes drug herself–with melatonin, alcohol or marijuana edibles–into getting more sleep. It backfired. “If I sleep seven or eight hours, I feel way worse,” she says. “Hung over, almost.”
Although the federal government recommends that Americans sleep seven or more hours per night for optimal health and functioning, new research is challenging the assumption that sleep is a one-size-fits-all phenomenon. Scientists have found that our internal body clocks vary so greatly that they could form the next frontiers of personalized medicine. By listening more closely to the ticking of our internal clocks, researchers expect to uncover novel ways to help everybody get more out of their sleeping and waking lives.
Searching for a good night’s rest? Find it by signing up for TIME’s guide to the scientific secrets of sleep.
Human sleep is largely a mystery. We know it’s important; getting too little is linked to heightened risk for metabolic disorders, Type 2 diabetes, psychiatric disorders, autoimmune disease, neurodegeneration and many types of cancer. “It’s probably true that bad sleep leads to increased risks of virtually every disorder,” says Dr. Louis Ptacek, a neurology professor at the University of California, San Francisco (UCSF). But details about what’s actually going on during shut-eye are sparse. “We know almost nothing about sleep and how it’s regulated,” says Ptacek.
Some people are morning larks, rising early, and others are night owls, who like staying up late. Those patterns are regulated by the body’s circadian rhythm, a 24-hour internal clock. People can manipulate their circadian rhythm through all kinds of external factors, like setting an alarm clock or exposing themselves to light. But the ideal sleep duration has long been thought to be universal. “There are many people who think everyone needs eight to eight and a half hours of sleep per night and there will be health consequences if they don’t get it,” says Ptacek. “But that’s as crazy as saying everybody has to be 5 ft. 10 in. tall. It’s just not true.”
Ptacek and his wife Ying-Hui Fu, also a professor of neurology at UCSF, are pioneers in the relatively new field of sleep genetics. About a decade ago, Fu discovered the first human gene linked to natural short sleep; people who had a rare genetic mutation seemed to get the same benefits from six hours of sleep a night as those without the mutation got from eight hours. In 2019, Fu and Ptacek discovered two more genes connected to natural short sleep, and they’ll soon submit a paper describing a fourth, providing even more evidence that functioning well on less sleep is a genetic trait.
The researchers are now collecting data on short sleepers in order to figure out just how rare these mutations are. “If we can get a better understanding of why their sleep is more efficient, we can then come back and help everybody sleep more efficiently,” Fu says. Among the participants is Chou, who also happens to work at UCSF. One day at a faculty meeting, she and Ptacek chatted about his work. She immediately recognized herself when he described short sleepers. “I had never heard of this. But once I started reading about it, it was sort of an epiphany.”
Chou doesn’t know yet if she has the identified genetic variants. But after the researchers interviewed her about her family’s sleeping patterns, she realized her mom is also a short sleeper. “I have memories of when I was younger, and my dad being frustrated with her for staying up really late, but she always seemed fine,” she says. The researchers took blood samples from both women.
Doctors once dismissed short sleepers like Chou as depressed or suffering from insomnia. Yet short sleepers may actually have an edge over everyone else. Research is still early, but Fu has found that besides being more efficient at sleep, they tend to be more energetic and optimistic and have a higher tolerance for pain than people who need to spend more time in bed. They also tend to live longer. Chou says the first three hold true for her; by nature, she is sunny and positive, and though she often finds bruises on her body, she usually doesn’t remember getting them. “I find it annoying how much people complain about little physical pains,” she says.
So far, these are just intriguing observations. But by studying genetic short sleepers, Fu and Ptacek believe they’ll eventually learn lessons for the rest of us. “As we identify more and more genes and we think about the pathways in which they function, at some point, a picture is going to emerge, and we will begin to have an understanding of how sleep is regulated in greater detail,” Ptacek says. This, they hope, will lead to targeted treatments, like pills or vitamins, to improve sleep efficiency in everyone.
Researchers are also looking beyond sleep to other circadian bodily processes that might benefit from a personalized or targeted approach. While a master clock in the brain acts like a conductor, setting time for the whole body, the rest of the body is like orchestra players with clocks of their own. “All your organs have rhythms,” says Steven Lockley, an associate professor of medicine at Harvard Medical School who studies circadian rhythms and sleep. “There’s a clock in your heart, a clock in the lungs, a clock in the kidneys.” Just about everything in the body–metabolism, hormones, the immune system, reproductive function and the way DNA is translated–is influenced by a circadian rhythm, he says.
And not everybody’s is the same. People’s internal clocks are often hours off from one another, Lockley says. “The range of individual differences is much bigger than anyone really understands yet.”
The body’s complex clock system has implications for both healthy people and those with medical conditions, and scientists are already seeing glimpses of how they can time certain tests and treatments to get more accurate or potent results. A cholesterol reading, for example, might be affected by what time of day you go to the doctor’s office, because the liver (which makes cholesterol) has a circadian rhythm. “The time of day at which you measure something could make someone look clinically abnormal, even though they’re not,” Lockley says.
Medicine might also be more effective if taken at a certain time. Because they’re metabolized in the liver, “drugs change their effects throughout the day,” Lockley says. Other circadian bodily processes, like cell function, can also affect how medication acts. Early research suggests certain drugs–including some for colorectal cancer, pain and asthma–perform better or are less toxic when taken at different times of day.
Exercise, which can be as powerful as medicine for some conditions, is good for you whenever you do it. “But I do think that the time of day may have an influence, on top of the effects of exercise, on our metabolic health,” says Juleen Zierath, professor of physiology at Karolinska Institute in Sweden. In one small study published in 2018 in the journal Diabetologia, Zierath and her team started 11 men with Type 2 diabetes on a high-intensity interval training program. The men exercised either in the morning (around 8 a.m.) or the afternoon (4 p.m.) for two weeks, then switched schedules. The researchers expected that regardless of the time of day, men in both groups would see improvements in blood-sugar levels. But “when they exercised in the morning, they actually had slightly higher levels of blood sugar [than baseline], which we didn’t expect at all,” Zierath says. It’s not clear to what extent the type of exercise and other variables matter, but the study provides an intriguing hint that time of day might make a difference for exercise.
Scientific knowledge is nascent when it comes to optimizing testing and treatment by the clock. Our understanding of individual circadian time is even more primitive. But Lockley believes it’s the key to personalized medicine; he and others are exploring ways to measure a person’s internal circadian time through simple clinical tests. “Hopefully in the next five to 10 years, you’d go to the doctor, give a breath test or a pee sample, and the doctor would know your biological time,” he says. “Then all your test results and treatments could be based on your real internal time, which is going to be very different between you and me based on our internal clocks.”
For now, even the understanding that our bodies often operate according to different clocks is a big scientific advance. It’s already changed the way Chou sleeps, lives and works. “I’ve just become more comfortable with accepting my sleep,” she says. She now asks her employees about their sleep schedules to anticipate when each will be at their peak. She also informs everyone about her own abbreviated schedule, so they know she doesn’t expect an immediate response to an email she sends at 4:05 a.m. “That’s just when my brain is working,” she says.
More Must-Reads from TIME
- Breaking Down the 2024 Election Calendar
- Heman Bekele Is TIME’s 2024 Kid of the Year
- The Reintroduction of Kamala Harris
- A Battle Over Fertility Law in China
- For the Love of Savoring Sandwiches : Column
- The 1 Heart-Health Habit You Should Start When You’re Young
- Cuddling Might Help You Get Better Sleep
- The 50 Best Romance Novels to Read Right Now
Write to Mandy Oaklander at [email protected]
Search form
Sleep on it: how the brain processes many experiences — even when ‘offline’.

(AI-generated image, created and edited by Michael S. Helfenbein)
Humans and other animals encounter and remember countless experiences each day; when we sleep, groups of cells in the brain known as neuronal ensembles replay these experiences to consolidate them into memories and “preplay” futures ones, which enables faster encoding of new experiences into memories later on.
Better understanding how these neuronal ensembles represent, or depict, these experiences would offer important insights into how memory and the mind function. But most studies to date have focused solely on animals undergoing just one or a small handful of sequential experiences — and it remains unclear how exactly the brain is able to process numerous experiences simultaneously during sleep.
In a new study, Yale scientists revealed a generative coding capacity in the brain’s hippocampus — an area responsible for memory and learning — which enables the brain to bundle together the representations of some 15 unrelated experiences that occurred across one full day within single sub-second events, known as frames, during sleep.
This computer-like capacity for parallel processing of different chains of information helps explain why humans and other animals are able to process a cascade of experiences and either keep separate or combine their meanings.
The findings were published in the journal Nature Neuroscience .
“ The brain mechanisms we uncovered are relevant for how we form and express internally generated representations about the world, like memories, imagining, and insight,” said George Dragoi , an associate professor of psychiatry and of neuroscience at Yale School of Medicine and corresponding author of the study.
An increasing amount of neuroscience research is exploring how neuronal ensembles represent experiences in the brain, a complex process that has implications for learning and memory, cognitive mapping, and spatial navigation. The fact that most studies involve animals undergoing a single experience, however, has prevented researchers from assembling a more complete picture.
“ In real life we are continuously experiencing new contexts and events that all need to be encoded distinctly and remembered later without a major interference between them,” Dragoi said. “The way the brain solves this problem is not known and experiments attempting to address this topic are essentially missing.
“ Computational models have proposed that exposure to multiple experiences would lead to a ‘catastrophic interference’ between the brain representations of new and older experiences, causing the individual to forget the latter,” Dragoi said. “That, of course, is not how daily life works.”
For the new study, the researchers recorded the neuronal activity of hippocampal neurons in rats that were allowed to move freely through 15 different spatial contexts over 19 ½ hours, a time span that included periods of extended sleep, during a single day. (The periods of sleep were used to investigate “offline” activity in the animals’ brains, in terms of preplay and replay of experiences.)
Using innovative data analysis, they identified several coding schemes in the hippocampus that boost its network capacity and efficiency during sleep and allow the brain to process representations of several experiences without interference.
Specifically, they found that the brain is able to “flicker” between time-compressed representations from two or more distinct experiences within the same sleep preplay and replay events, a feature that greatly increases network capacity for parallel information processing without interference during sleep. In addition, independent experiences can be bound together into longer preplay/replay episodes representing sequential aspects of day-long experiences in the order in which they occurred compressed into replay episodes less than a second in duration.
The researchers also identified a kind of serial position effect in this process, whereby the first and most recent experiences had the strongest representations during the animals’ sleep, a phenomenon similar to the effect observed in human memory in which people tend to recall the first and last events in a series of events or items.
Other authors of the paper are Kefei Liu and Jeremie Sibille, a former associate research scientist and postdoctoral associate, respectively, in Dragoi’s lab at Yale School of Medicine.
Health & Medicine
Media Contact
Bess Connolly : [email protected] ,

Harnessing the entirety of India’s human capital

Did Colombia’s nationwide preschool expansion benefit students?

COVID-19: New research shows how the virus enters our cells

The science behind the latest mpox global health emergency
- Show More Articles
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- CAREER FEATURE
- 17 July 2023
- Correction 25 October 2023
How better sleep can improve productivity
- Nikki Forrester 0
Nikki Forrester is a science journalist based in Davis, West Virginia.
You can also search for this author in PubMed Google Scholar
Sleep has a profound impact on human health, improving attention, memory, emotional regulation and work performance, and reducing the risk of disease 1 , 2 . But over the past few decades, the amount of sleep that people get has declined substantially. A 2012 study 3 of some 690,000 children from 20 countries found that nightly sleep duration fell by more than an hour from 1905 to 2008. Nearly one-third of adults in the United States sleep for less than six hours per night 2 , and sleep duration has dropped since the 1960s for adults in Japan, Russia, Finland, Germany, Belgium and Austria 4 .
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 619 , 659-661 (2023)
doi: https://doi.org/10.1038/d41586-023-02307-z
Updates & Corrections
Correction 25 October 2023 : This Career feature erroneously stated that ref. 3 was published in 2017.
Matricciani, L. et al. Sleep Health 3 , 317–323 (2017).
Article PubMed Google Scholar
Sheehan, C. M., Frochen, S. E., Walsemann, K. M. & Ailshire, J. A. Sleep 42 , zsy221 (2019).
Article Google Scholar
Matricciani, L., Olds, T. & Petkov, J. Sleep Med. Rev. 16 , 203–211 (2012).
Bin, Y. S., Marshall, N. S. & Glozier, N. Sleep Med. Rev. 16 , 223–230 (2012).
Tandon, A., Kaur, P., Dhir, A. & Mäntymäki, M. Comput. Human Behav. 113 , 106487 (2020).
Berger, H. Archiv f. Psychiatrie 87 , 527–570 (1929).
Loomis, A. L., Harvey, E. N. & Hobart, G. A. J. Exp. Psychol. 21 , 127–144 (1937).
Patel, A. K., Reddy, V., Shumway, K. R. & Araujo, J. F. StatPearls (Treasure Island, 2023).
Google Scholar
Miller, K. E. & Gehrman, P. R. Curr. Biol. 29 , R806–R807 (2019).
Cai, D. J., Mednick, S. A., Harrison, E. M., Kanady, J. C. & Mednick, S. C. Proc. Natl Acad. Sci. USA 106 , 10130–10134 (2009).
Rao, R. & Tripathi, R. in Sleep and Neuropsychiatric Disorders 811–833 (Springer, 2022).
Silvani, M. I., Werder, R. & Perret, C. Front. Physiol. 13 , 943108 (2022).
Yang, P.-Y., Ho, K.-H., Chen, H.-C. & Chien, M.-Y. J. Physiother. 58 , 157–163 (2012).
Hirotsu, C., Tufik, S. & Levy Andersen, M. Sleep Sci. 8 , 143–152 (2015).
McCarthy, M. E. & Waters, W. F. Sleep 20 , 115–123 (1997).
Van Dongen, H. P. A., Maislin, G., Mullington, J. M. & Dinges, D. F. Sleep 26 , 117–126 (2003).
Rusch, H. L. et al. Ann. NY Acad. Sci. 1445 , 5–16 (2018).
Dube, N., Khan, K., Loehr, S., Chu, Y. & Veugelers, P. Int. J. Behav. Nutrition Phys. Activity 14 , 97 (2017).
Landolt, H.-P. Biochem. Pharmacol. 75 , 2070–2079 (2008).
Datta, K. et al. Natl Med. J. India 34 , 143–150 (2021).
Dickson, G. T. & Schubert, E. Front. Psychol. 11 , 1695 (2020).
Download references
Related Articles

Training: Networking for researchers
- Research management

‘There’s a lot of privilege masquerading as merit’: why inclusion matters in academia
Career Q&A 19 AUG 24

Gender bias might be working at level of whole disciplines
Nature Index 19 AUG 24

How to win funding to talk about your science
Career Feature 15 AUG 24

These labs have prepared for a big earthquake — will it be enough?
News 18 AUG 24

Chatbots in science: What can ChatGPT do for you?
Career Column 14 AUG 24

Friends or foes? An academic job search risked damaging our friendship

Cash for catching scientific errors
Technology Feature 19 AUG 24
The need for equity in Brazilian scientific funding
Correspondence 13 AUG 24
Canadian graduate-salary boost will only go to a select few
Faculty Positions in the Center for Nonhuman Primate Research in the School of Life Sciences
SLS invites applications for multiple tenure-track/tenured faculty positions at all academic ranks.
Hangzhou, Zhejiang, China
School of Life Sciences, Westlake University
Faculty Position, Center of Excellence in Neuro-Oncology Sciences (CENOS)
Memphis, Tennessee
St. Jude Children's Research Hospital (St. Jude)
Postdoctoral Fellow Position
Birmingham, Alabama (US)
University of Alabama at Birmingham (UAB)
Postdoctoral Scholar - Pharmaceutical Sciences
The University of Tennessee Health Science Center (UTHSC)
Postdoctoral Scholar- Speech Language Pathologist
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
What Is Sleep Efficiency—And How Can You Improve It?
Doctors explain why it's an important factor in getting the rest you need.

Sleep efficiency refers to the amount of time you spend actually asleep versus the time you spend in bed intending to sleep, explains Zachary Strumpf , M.D., a pulmonary, critical care, and sleep medicine physician at University Hospitals in Cleveland, Ohio.
“It’s different than getting a better night’s sleep and reflects how effective you are at falling and staying asleep,” he says. Sleep efficiency is expressed as a percentage, and it can vary from person to person.
Having a good sleep efficiency doesn’t necessarily mean that you’re getting good sleep, however, says Nishay Chitkara , M.D., director of sleep medicine at NYC Health + Hospitals/Bellevue.
“For example, if one is sleeping only five hours per night, the sleep efficiency may be great, but the time asleep is not sufficient,” he says. You need to get enough sleep, as well, and address any problems that are causing sleep disruption.
This is crucial, as a third of Americans don’t even get seven hours of sleep a night, the minimum recommended amount for adults, according to the Centers for Disease Control and Prevention .
Sleep efficiency can be affected by many things, including diet, exercise levels, sleep schedules, and sleep environments, Dr. Chitkara says. It’s important to know how to calculate sleep efficiency and what you can do to improve it, which will contribute to feeling more rested.
How Do You Calculate Sleep Efficiency?
SLEEP EFFICIENCY IS the ratio of the time you spend asleep relative to the time you dedicate to sleep, Dr. Chitkara explains. To calculate it, divide the total minutes you’re asleep by the total minutes spent in bed trying to go to sleep.
If you usually go right to sleep after climbing into bed, your sleep efficiency is likely good, Dr. Strumpf says.
Generally, sleep efficiency of 85 to 90 percent or greater suggests that you have little trouble falling and staying asleep, he says. But if it’s lower than 80 percent, you likely have poor sleep efficiency.
“A lower sleep efficiency likely needs improvement, since it could indicate that someone is not sleeping well, has poor sleep habits, or may have a medical condition that interferes with healthy sleep,” Dr. Chitkara says.
Sleep efficiency can also decline with age, Dr. Strumpf says. Research shows that sleep efficiency below 80 percent increases mortality risk for older people, and pain, sleep medication use, and bad dreams are the main factors for their poor sleep efficiency. Men between the ages of 65 and 96 were more likely to have low sleep efficiency when they were single or had a painful illness.
It might seem like taking sleep medications would increase sleep efficiency, but Dr. Strumpf says they can actually alter various aspects of sleep depending on the person. "Certain medications can increase or decrease a person’s sleep efficiency or alter the proportion of time spent in REM sleep," he says.
Working with a sleep doctor includes recommending medications and reviewing the effects they could have on your sleep, Dr. Strumpf says.

How to Improve Your Sleep Efficiency
YOU CAN GENERALLY improve your sleep efficiency by optimizing your sleep hygiene, Dr. Chitkara says. “Sleep hygiene is the set of practices that are conducive to good sleep.”
These practices include:
- Maintaining a regular sleep schedule—that is, going to bed and waking up at the same times daily
- Getting seven to eight hours of sleep a night
- Avoiding caffeine late in the day
- Going alcohol-free three to four hours before sleep
- Avoiding watching TV or scrolling your phone an hour prior to sleep
- Cutting out napping
Spending less time in bed when you’re not ready to fall asleep is another way to increase sleep efficiency, Dr. Strumpf says.
“However, a higher sleep efficiency is not the only thing to target for restful sleep,” he says. You also need adequate sleep duration, meaning staying asleep for a long stretch, ideally at least seven hours.
“Ensuring adequate sleep duration and good sleep efficiency will allow your brain to naturally cycle through all the stages of sleep you need,” Dr. Strumpf says. These stages are controlled by the systems in the brain and usually can’t be influenced with behavioral changes.
Can Sleep Trackers Help?
SLEEP TRACKER APPS or other devices could help improve sleep efficiency by providing information and insights into your sleep habits, which you can use to make improvements, Dr. Chitkara says.
For instance, they can keep track of light, temperature, noise levels, and other environmental elements influencing your sleep, as well as caffeine intake and stress levels, he says. Trackers can also record health metrics, such as heart rate, movement, body temperature, and blood oxygen levels.
When to See a Doctor
ANY TIME YOU ’RE having trouble falling or staying asleep, waking up several times a night, or feeling excessively sleepy throughout the day, talk to your doctor, Dr. Strumpf urges. Your doctor may refer you to a sleep specialist.
It’s especially important to get evaluated if these symptoms last for more than three months or if your bed partner is complaining that their sleep is disrupted, Dr. Chitkara says.
Also get checked out if you notice any symptoms of sleep apnea, a dangerous condition where you constantly stop and start breathing when you sleep, Dr. Strumpf says. These signs include snoring, gasping or choking during sleep, or periods of not breathing when you’re asleep.

.css-sq6566{height:1.25rem;}@media(max-width: 48rem){.css-sq6566{overflow:unset;line-height:1.25rem;}}@media(min-width: 48rem){.css-sq6566{line-height:1.25rem;}}.css-sq6566:before{background-color:#D2232E;color:#fff;margin-right:0.625rem;width:1.25rem;height:1.25rem;content:'';display:block;} Health

What Body Composition Numbers Mean

The Maui Aftermath

How to Get Rid of Stubborn Belly Fat

What You Need to Know About Early Alzheimer’s

Does Ozempic Raise or Lower Testosterone?

A Look at Chase Kalisz's Newest Quest

Smarter Workouts Got This Guy Shredded in 16 Weeks

Checking in With the Ultimate Men's Health Guys

10 Signs You're Dealing With a Sociopath

What You Should Know About the Mouth Taping Trend

How to Keep Your Brain Sharp as You Age
- Introduction
- Conclusions
- Article Information
Participants continued to live in their home environment without any prescribed diet or physical activity during the 28 consecutive days of the study. Error bars are SEs of the mean. The vertical dashed line separates the two 2-week sleep periods.
A-D, Data are in ascending order of change in sleep duration for the control group and sleep extension group. E, Data were from 74 participants. All available data were used. The line represents the line of best fit from the linear regression model. One participant in the control group and 3 participants in the sleep extension group had missing data in change in sleep duration (ie, missing mean data in at least 1 of 2 study periods). One participant in the control group and 4 participants in the sleep extension group had missing data in change in energy intake. Overall, 1 participant in the control group and 5 participants in the sleep extension group had missing data in either change in sleep duration or change in energy intake.
Trial Protocol
eMethods. Participants, Inclusion and Exclusion Criteria
eReferences
eTable 1. Effect of Treatment on Actigraphy-Based Time in Bed and Sleep Duration on All Days, Workdays and Free Days
eTable 2. Effect of Treatment on Actigraphy-Based Outcomes
eTable 3. Baseline Characteristics of Participants With Complete vs Incomplete Data
eTable 4. Self-Reported Outcomes by Visual Analog Scales
Data Sharing Statement
- Good Sleep, Better Life—Enhancing Health and Safety With Optimal Sleep JAMA Internal Medicine Invited Commentary April 1, 2022 Mark R. Rosekind, PhD; Rafael Pelayo, MD; Debra A. Babcock, MD
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Tasali E , Wroblewski K , Kahn E , Kilkus J , Schoeller DA. Effect of Sleep Extension on Objectively Assessed Energy Intake Among Adults With Overweight in Real-life Settings : A Randomized Clinical Trial . JAMA Intern Med. 2022;182(4):365–374. doi:10.1001/jamainternmed.2021.8098
Manage citations:
© 2024
- Permissions
Effect of Sleep Extension on Objectively Assessed Energy Intake Among Adults With Overweight in Real-life Settings : A Randomized Clinical Trial
- 1 Department of Medicine, The University of Chicago, Chicago, Illinois
- 2 Department of Public Health Sciences, The University of Chicago, Chicago, Illinois
- 3 Biotechnology Center, Department of Nutritional Sciences, University of Wisconsin–Madison, Madison
- Invited Commentary Good Sleep, Better Life—Enhancing Health and Safety With Optimal Sleep Mark R. Rosekind, PhD; Rafael Pelayo, MD; Debra A. Babcock, MD JAMA Internal Medicine
Question What is the effect of sleep extension on objectively assessed energy intake in adults with overweight in their usual home environment?
Findings In this randomized clinical trial of 80 adults with overweight and habitual sleep less than 6.5 hours per night, those randomized to a 2-week sleep extension intervention significantly reduced their daily energy intake by approximately 270 kcal compared with the control group. Total energy expenditure did not significantly differ between the sleep extension and control groups, resulting in a negative energy balance with sleep extension.
Meaning The findings suggest that improving and maintaining adequate sleep duration could reduce weight and be a viable intervention for obesity prevention and weight loss programs.
Importance Short sleep duration has been recognized as a risk factor for obesity. Whether extending sleep duration may mitigate this risk remains unknown.
Objective To determine the effects of a sleep extension intervention on objectively assessed energy intake, energy expenditure, and body weight in real-life settings among adults with overweight who habitually curtailed their sleep duration.
Design, Setting, and Participants This single-center, randomized clinical trial was conducted from November 1, 2014, to October 30, 2020. Participants were adults aged 21 to 40 years with a body mass index (calculated as weight in kilograms divided by height in meters squared) between 25.0 and 29.9 and had habitual sleep duration of less than 6.5 hours per night. Data were analyzed according to the intention-to-treat principle.
Interventions After a 2-week habitual sleep period at baseline, participants were randomized to either an individualized sleep hygiene counseling session that was intended to extend their bedtime to 8.5 hours (sleep extension group) or to continue their habitual sleep (control group). All participants were instructed to continue daily routine activities at home without any prescribed diet or physical activity.
Main Outcomes and Measures The primary outcome was change in energy intake from baseline, which was objectively assessed as the sum of total energy expenditure and change in body energy stores. Total energy expenditure was measured by the doubly labeled water method. Change in body energy stores was computed using regression of daily home weights and body composition changes from dual-energy x-ray absorptiometry. Sleep duration was monitored by actigraphy. Changes from baseline were compared between the 2 groups using intention-to-treat analysis.
Results Data from 80 randomized participants (mean [SD] age, 29.8 [5.1] years; 41 men [51.3%]) were analyzed. Sleep duration was increased by approximately 1.2 hours per night (95% CI, 1.0 to 1.4 hours; P < .001) in the sleep extension group vs the control group. The sleep extension group had a significant decrease in energy intake compared with the control group (−270 kcal/d; 95% CI, −393 to −147 kcal/d; P < .001). The change in sleep duration was inversely correlated with the change in energy intake ( r = −0.41; 95% CI, −0.59 to −0.20; P < .001). No significant treatment effect in total energy expenditure was found, resulting in weight reduction in the sleep extension group vs the control group.
Conclusions and Relevance This trial found that sleep extension reduced energy intake and resulted in a negative energy balance in real-life settings among adults with overweight who habitually curtailed their sleep duration. Improving and maintaining healthy sleep duration over longer periods could be part of obesity prevention and weight loss programs.
Trial Registration ClinicalTrials.gov Identifier: NCT02253368
Obesity is a major public health concern. 1 The obesity epidemic appears to coincide with a pattern of sleeping less that has been observed in society over the past several decades. For example, one-third of the US population reported not getting the recommended 7 to 9 hours of sleep per night. 2 - 4 Substantial evidence suggests that sleeping less than 7 hours per night on a regular basis is associated with adverse health consequences. 5 Particularly, insufficient sleep duration has been increasingly recognized as an important risk factor for obesity. 6 , 7 Prospective epidemiologic studies suggest that short sleep duration is an important risk factor for weight gain. 8 - 10 However, it remains unknown whether extending sleep duration can be an effective strategy for preventing or reversing obesity. Although sleep hygiene education is encouraged by obesity experts, 11 most health professionals and patients do not implement obtaining adequate sleep duration as part of the strategies to combat the obesity epidemic. 12
At the population level, the association between energy flux and body weight implicates that increased energy intake is the main factor in higher body weights in modern society. 13 According to dynamic prediction models, a sustained increase in energy intake of even 100 kcal/d would result in a weight gain of about 4.5 kg over 3 years. 14 , 15 Factors that underlie the observed persistent increase in energy intake and mean weight gain at the population level need to be better understood. One such factor is insufficient sleep duration. Short-term experimental laboratory studies have found that sleep restriction in healthy individuals is associated with an increased mean energy intake of about 250 to 350 kcal/d with minimal to no change in energy expenditure. 16 - 19 However, these laboratory studies do not represent real life. The magnitude of sleep restriction was extreme in most cases, and energy intake was ascertained from a single or a few meals. In a real-life setting in which participants continue their normal daily activities, multiple interacting factors (eg, social interactions and free-living physical activity) can influence energy intake or expenditure and weight.
To date, it remains unknown whether and to what extent an intervention that is intended to increase sleep duration in a real-life setting affects energy balance and body weight. We conducted a randomized clinical trial (RCT) to determine the effects of a sleep extension intervention on objectively assessed energy intake, energy expenditure, and body weight in real-life settings among adults with overweight who habitually curtailed their sleep duration.
This single-center, parallel-group RCT was conducted from November 1, 2014, to October 30, 2020. The protocol was approved by The University of Chicago Institutional Review Board, and participants provided written informed consent. The study protocol is available in Supplement 1 . We followed the Consolidated Standards of Reporting Trials ( CONSORT ) reporting guideline.
Adult men and women aged 21 to 40 years with a body mass index (calculated as weight in kilograms divided by height in meters squared) between 25.0 and 29.9 and a mean habitual sleep duration of less than 6.5 hours per night were eligible. Individuals were required to have stable self-reported sleep habits for the past 6 months. They were recruited from the community and completed an initial online survey followed by a face-to-face interview. Race and ethnicity data were self-reported at this time and included the following race and ethnicity categories: Asian, Black or African American, Hispanic, and White. Those who met the inclusion criteria underwent laboratory screening (polysomnography, oral glucose tolerance test, and blood tests) to determine eligibility. Habitual sleep duration was confirmed by a 1-week screening wrist actigraphy at home. Those who had obstructive sleep apnea confirmed by laboratory polysomnography (apnea-hypopnea index >5), insomnia or history of any other sleep disorder, or night shift and rotating shift work (current or in the past 2 years) were excluded. Detailed eligibility criteria are provided in the eMethods in Supplement 2 .
After a 2-week habitual sleep period at baseline, participants were randomized to either 2-week sleep extension (sleep extension group) or 2-week continued habitual sleep (control group) ( Figure 1 ). Participants continued their daily routine activities at home without any prescribed diet or physical activity.
To blind participants to the sleep extension intervention, we described the study in the recruitment materials as follows: “we will collect information about sleep habits and metabolism.” The sleep extension group was blinded to randomization until after the 2-week baseline assessments, and the control group was blinded until the end of the 4-week study. This approach allowed us to capture habitual sleep-wake patterns without influencing participants' usual behavior or creating selection bias with only participants interested in improving sleep habits. After study completion, all participants were provided with information about the health benefits of optimal sleep duration. Block randomization, stratified by sex, was performed using computer-generated random numbers. Before the trial, randomization assignments were prepared by a biostatistician (K.W.) using opaque, sealed, and numbered envelopes and were given to the research coordinator (E.K.).
Sleep-wake patterns were continuously monitored at home by wrist actigraphy throughout the 4-week study. Participants were asked to wear an accelerometer (motion)-based monitor (Actiwatch Spectrum Plus; Philips) and to press a built-in event marker button when they went to bed to sleep each night and when they got out of bed each morning. Sleep was automatically scored (Actiware, version 6.0.9; Philips) using validated algorithms as the sum of all epochs that were scored as sleep during the total time spent in bed. 20 , 21
During the 2-week baseline, all participants were instructed to continue their habitual sleep patterns at home. On the morning of day 15, participants met with study investigators (E.T. and E.K.) in the research center. Those who were randomized to the sleep extension group received individualized sleep hygiene counseling through a structured interview (E.T.) (eMethods in Supplement 2 ). 22 At the end of the interview, participants were provided with individualized recommendations to follow at home for 2 weeks, with the aim of extending their bedtime duration to 8.5 hours. On day 22, participants returned for a brief follow-up visit. Actigraphy data from the first intervention week were reviewed, and further sleep counseling was provided as needed.
To minimize any imbalance in contact with the investigators between the 2 groups, we asked participants in the control group to meet with the study investigators on days 15 and 22. Actigraphy data of these participants were downloaded, but the participants did not receive any specific sleep recommendations and were instructed to continue their daily routine and habitual sleep behaviors until the end of the study.
For each 2-week period, the energy intake was calculated from the sum of total energy expenditure and change in body energy stores using the principle of energy balance. 14 , 23 , 24 Total energy expenditure was measured by the doubly labeled water method. 25 - 29 For each 2-week period, the change in body energy stores was computed from the regression (slope, grams per day) of daily home weights and change in body composition (ie, fat mass and fat-free mass) using dual-energy x-ray absorptiometry. Participants were provided a cellular-enabled weight scale (BodyTrace; BodyTrace Inc) and instructed to take their nude weights twice every morning after awakening before eating or drinking. Weight values were hidden from the participants to minimize potential influence on behavior. Changes in body composition were converted to changes in energy stores using 9.5 kcal/g as the energy coefficient of fat mass and 1.0 kcal/g as the energy coefficient of fat-free mass. 30 Resting metabolic rate was measured by indirect calorimetry for 30 minutes after fasting and for 4 hours after eating a standardized breakfast. Thermic effect of the meal was calculated, which was previously described elsewhere. 31 Activity energy expenditure was calculated by subtracting the resting metabolic rate and thermic effect of the meal from the total energy expenditure. 31 , 32 Additional details are provided in the eMethods in Supplement 2 .
The primary outcome was change in energy intake from baseline. A total final sample size of 80 participants (40 per group) was originally planned and provided 80% power to detect a true difference in energy intake between groups of 207 kcal/d using a 2-sided α = .05 significance threshold (trial protocol in Supplement 1 ). An intention-to-treat analysis was conducted in Stata, version 16 (StataCorp LLC) using 2-tailed tests with statistical significance set at P < .05. Categorical data are presented as counts and percentages. Continuous data are presented as means and SDs. Linear mixed-effects models were fit to determine the treatment differences between the groups. 33 Models included the randomization group, 2-week baseline period (period 1) vs 2-week intervention (period 2) and their interaction, and random effects for each participant. The treatment effect (95% CI) was estimated by the treatment group and period interaction, which is equivalent to testing the difference in change from baseline (period 2 minus period 1) in the sleep extension group vs the control group. To confirm the robustness of primary findings, we fit additional models using the analysis of covariance approach with the period 2 value as the dependent variable, treatment group as the independent variable, and period 1 value as covariates.
In secondary analyses, mixed models that adjusted for sex or menstrual cycle were also fit; these covariates were chosen because of the known influence of menstrual cycle on short-term changes in weight. A Pearson correlation coefficient was calculated to assess the relationships between the changes from baseline in sleep duration and the changes from baseline in energy intake. No adjustments were made to P values or CIs for multiple comparisons. Baseline characteristics of participants with complete data were compared with those of participants with incomplete data using unpaired, 2-tailed t tests and Fisher exact tests. No imputation for missing values was performed.
Of the 210 adults who provided consent and were assessed for eligibility, 81 were randomized (41 to the control group and 40 to the sleep extension group) initially ( Figure 1 ). One participant in the control group revealed adhering to a weight loss regimen and thus did not meet the study inclusion criteria and was deemed ineligible after randomization. 34 The 80 participants had a mean (SD) age of 29.8 (5.1) years and consisted of 41 men (51.3%) and 39 women (48.7%). Baseline characteristics of participants were similar between randomization groups ( Table 1 ). None of the participants were using any antihypertensive or lipid-lowering agents or any prescription medication that can affect sleep or metabolism.
Figure 2 illustrates the mean nightly sleep duration by actigraphy in each group throughout the 4-week study. Participants in the sleep extension group had a significant increase from baseline in mean sleep duration by actigraphy compared with those in the control group (1.2 hours; 95% CI, 1.0-1.4 hours; P < .001). The findings were similar with regard to change in sleep duration when only participants' workdays (1.3 hours; 95% CI, 1.0-1.5 hours; P < .001) or free days (1.1 hours; 95% CI, 0.7-1.5 hours; P < .001) were considered (eTable 1 in Supplement 2 ). No difference was found in change in sleep efficiency (percentage of time spent asleep during time in bed) between the 2 groups (–0.6 hours; 95% CI, –2.1 to 1.0 hours; P = .48), confirming the success of the intervention (eTable 2 in Supplement 2 ).
Energy intake was statistically significantly decreased in the sleep extension group compared with the control group (−270.4 kcal/d; 95% CI, −393.4 to −147.4 kcal/d; P < .001). Figure 3 A through D illustrates the changes from baseline in energy intake and the changes from baseline in sleep duration in individual participants. There was a significant increase in energy intake from baseline in the control group (114.9 kcal/d; 95% CI, 29.6 to 200.2 kcal/d) and a significant decrease in energy intake from baseline in the sleep extension group (−155.5 kcal/d; 95% CI, −244.1 to −66.9 kcal/d) ( Table 2 ). Considering all participants, the change in sleep duration was inversely correlated with the change in energy intake ( r = −0.41; 95% CI, −0.59 to −0.20; P < .001) ( Figure 3 E). Each 1-hour increase in sleep duration was associated with a decrease in energy intake of approximately 162 kcal/d (−162.3 kcal/d; 95% CI, −246.8 to −77.7 kcal/d; P < .001).
No statistically significant treatment effect was found in total energy expenditure or other measures of energy expenditure ( Table 2 ). Participants in the sleep extension group had a statistically significant reduction in weight compared with those in the control group (−0.87 kg; 95% CI, −1.39 to −0.35 kg; P = .001). There was weight gain from baseline in the control group (0.39 kg; 95% CI, 0.02 to 0.76 kg) and weight reduction from baseline in the sleep extension group (−0.48 kg; 95% CI, −0.85 to −0.11 kg) ( Table 2 ).
The findings on energy intake, energy expenditure, and weight were similar after adjustment for the effects of sex or menstrual cycle. No statistically significant differences in baseline characteristics were found between the 75 participants (93.8%) who had complete data on energy intake (primary outcome) vs participants with missing data on energy intake. The proportion of participants with complete data on energy intake was not significantly different between the sleep extension and control groups (90.0% vs 97.5%; P = .36). When all reported outcomes were considered, no significant differences (except for depressive symptoms) in baseline characteristics were found between participants with complete data and participants with incomplete or missing data (eTable 3 in Supplement 2 ). The proportion of participants with complete data on all reported outcomes was similar between the sleep extension and control groups (82.5% vs 85.0%; P > .99).
In this RCT of adults with overweight who habitually curtailed their sleep duration, sleep extension reduced energy intake and resulted in a negative energy balance (ie, energy intake that is less than energy expenditure) in real-life settings. To our knowledge, this study provides the first evidence of the beneficial effects of extending sleep to a healthy duration on objectively assessed energy intake and body weight in participants who continued to live in their home environment. Modest lifestyle changes in energy intake or expenditure are increasingly promoted as viable interventions to reverse obesity.
According to the Hall dynamic prediction model, a decrease in energy intake of approximately 270 kcal/d, which we observed after short-term sleep extension, would predict an approximately 12-kg weight loss over 3 years if the effects were sustained over a long term. 14 , 15 However, this study cannot infer how long healthy sleep habits may be sustained. Nevertheless, these modeling predictions on weight change suggest that continued adequate sleep duration and beneficial effect on energy intake could translate into clinically meaningful weight loss and help reverse or prevent obesity. Thus, the findings of this study may have important public health implications for weight management and policy recommendations.
The findings of decreased energy intake, negative energy balance, and weight reduction resulting from sleep extension are in agreement with the findings of short-term laboratory sleep-restriction studies showing increased energy intake and weight gain 17 as well as the findings of prospective epidemiologic studies linking sleep restriction to obesity risk. 8 A recent meta-analysis of randomized controlled laboratory studies found that short-term sleep restriction over 1 to 14 days of duration in healthy individuals was associated with increases of mean energy intake by approximately 253 kcal/d, as assessed during a single meal. 17 Another meta-analysis of prospective cohort studies found that the risk of obesity increased by 9% for each 1-hour decrease in sleep duration. 8 We did not observe a statistically significant change in total energy expenditure by doubly labeled water method or mean daytime activity counts by actigraphy (eTable 2 in Supplement 2 ). Although some laboratory sleep-restriction studies reported an increase in total energy expenditure of approximately 92 to 111 kcal/d, using a whole-room calorimeter, 35 , 36 other studies observed no change. 16 , 37 We found a modest reduction in weight after sleep extension, and the composition of weight change was primarily in fat-free mass, which is consistent with the short-term changes in body composition. 38 , 39 If sleep is extended over longer periods, weight loss in the form of fat mass would likely increase over time. A few observations suggest that sleeping 7 to 8 hours per night is associated with greater success in weight loss interventions. 40 - 43
In this RCT, we found an overall increase in objective sleep duration of approximately 1.2 hours in participants who habitually slept less than 6.5 hours per night. The change in sleep duration from baseline varied between participants and from night to night in the real-life setting. Overall, the sleep extension group compared with the control group had significantly higher subjective scores in obtaining sufficient sleep, with more daytime energy and alertness and better mood (eTable 4 in Supplement 2 ). Similar to a previous study of sleep extension, 22 the present RCT used an individualized counseling approach. Another study used bedtime extension in habitual short sleepers in real-life conditions but obtained variable benefits on sleep, likely because of a lack of an individualized approach or appropriate blinding. 44 None of these previous studies objectively measured energy intake.
Future similarly rigorous intervention studies of longer duration and using objective assessments of energy balance under real-life conditions are warranted to elucidate the underlying mechanisms and to investigate whether sleep extension could be an effective, scalable strategy for reversing obesity in diverse populations. Along with a healthy diet and regular physical activity, healthy sleep habits should be integrated into public messages to help reduce the risk of obesity and related comorbidities.
This study has several strengths. The major strengths are the randomized design and the objective tracking of energy intake and sleep in real-life settings. Most epidemiologic studies linking short sleep duration to body weight relied on self-reported dietary intake. 45 We did not collect self-reported dietary data because this method is subject to bias and has been shown to be inaccurate compared with the doubly labeled water method. 46 , 47 Most experimental studies that measured energy intake used a single meal under unnatural laboratory conditions. We used a validated method to objectively track energy intake by the doubly labeled water method and change in energy stores. 23 , 48 , 49 In this trial, we objectively quantified energy intake after sleep extension while individuals continued their daily routine in their usual environment. Participant blinding and use of actigraphy allowed us to capture true habitual sleep patterns at baseline. 22 , 50 In addition, we excluded insomnia and sleep apnea.
This study also has several limitations. We enrolled adults with overweight and used selective eligibility criteria, which may limit generalizability to more diverse populations. The increase in energy intake and weight from baseline that we observed in the control group may have contributed to the significant treatment effects. However, in RCTs, performing a between-group comparison, rather than separate tests against baseline within the groups, is strongly recommended. 51 The study did not provide information on how long healthy sleep habits could be maintained over longer periods. 44 We did not systematically assess the factors that may have influenced sleep behavior, but limiting the use of electronic devices appeared to be a key intervention among the participants (eTable 4 in Supplement 2 ). The doubly labeled water method has a precision of 5%, which may translate into some degree of uncertainty in the energy intake calculations. Although whole-room calorimeters can measure energy expenditure with a higher precision of approximately 1% to 2%, they do not represent real-life measurement and are not feasible over longer periods. We did not assess the underlying biological mechanisms of food frequency and the circadian timing of food intake. Multiple interrelated factors could contribute to the finding of decreased energy intake after sleep extension. 6 , 52 Evidence from laboratory sleep restriction studies suggests that increased hunger, alterations in appetite-regulating hormones, and changes in brain regions related to reward-seeking behavior are potential mechanisms that promote overeating after sleep restriction. 6 , 45
This RCT found that short-term sleep extension reduced objectively measured energy intake and resulted in a negative energy balance in real-life settings in adults with overweight who habitually curtailed their sleep duration. The findings highlighted the importance of improving and maintaining adequate sleep duration as a public health target for obesity prevention and increasing awareness about the benefits of adequate sleep duration for healthy weight maintenance.
Accepted for Publication: November 14, 2021.
Published Online: February 7, 2022. doi:10.1001/jamainternmed.2021.8098
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2022 Tasali E et al. JAMA Internal Medicine .
Corresponding Author: Esra Tasali, MD, Department of Medicine, The University of Chicago, 5841 S Maryland Ave, Chicago, IL 60637 ( [email protected] ).
Author Contributions: Author Dr Tasali and Ms Wroblewski had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Tasali, Schoeller.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Tasali, Schoeller.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Tasali, Wroblewski.
Obtained funding: Tasali.
Administrative, technical, or material support: Tasali, Kahn, Kilkus, Schoeller.
Supervision: Tasali.
Other - research coordination duties: Kahn.
Conflict of Interest Disclosures: None reported.
Funding/Support: This study was funded by grants R01DK100426, CTSA-UL1 TR0002389, and UL1TR002389 from the National Institutes of Health and by the Diabetes Research and Training Center at The University of Chicago.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement : See Supplement 3 .
Additional Contributions: Timothy Shriver, MS, University of Wisconsin–Madison, assisted with doubly labeled water measurements. Maureen Costello, MS, The University of Chicago, assisted with dual-energy x-ray absorptiometry scans. Becky Tucker, BA, Harry Whitmore, RPSGT, and Kristin Hoddy, PhD, RD, The University of Chicago, assisted with data collection. We thank the nurses, dieticians, and technicians at the Clinical Research Center at The University of Chicago for their expert assistance in data collection. We also thank the staff of the Sleep Research Center at The University of Chicago for their support. These individuals received no additional compensation, outside of their usual salary, for their contributions. We thank the volunteers for participating in this study.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Olivia Rodrigo sleeps 13 hours a night on Guts World Tour. Is too much sleep bad for you?

Performing a world tour doesn't just take guts . According to Olivia Rodrigo , it also takes sleeping like a vampire .
“Well, I sleep so much on tour," the 21-year-old "Vampire" songstress, currently on her Guts World Tour , told Complex in an article published Friday. "I sleep for 13 hours a day sometimes. I’m so exhausted. So that passes a lot of the time."
Rodrigo isn't the only celebrity who can sleep well over 12 hours. In December, Dakota Johnson, 34, told The Wall Street Journal that she's "not functional" if she gets less than 10 hours of sleep and "can easily go 14 hours" asleep in one night.
"I don’t have a regular (wake-up) time," Johnson said. "It depends on what’s happening in my life. If I’m not working, if I have a day off on a Monday, then I will sleep as long as I can. Sleep is my number one priority in life."
But is there such a thing as too much sleep?
It all depends. Experts say the ideal amount of sleep varies among individuals, but pushing 13 or 14 hours on a regular basis is likely overdoing it. However, if someone is especially tired or sleep-derived, then that amount of sleep might be warranted every once in a while.
"There’s a range," Shelby Harris , a licensed clinical psychologist and the author of "The Women's Guide to Overcoming Insomnia: Get a Good Night's Sleep without Relying on Medication," previously told USA TODAY. "The majority of people fall somewhere between seven to nine hours of sleep a night ... but there are some people who are outliers, with some needing only six hours and others closer to 10."
More: Dakota Johnson says she sleeps up to 14 hours per night. Is too much sleep a bad thing?
How much sleep should you get, according to research?
For middle-aged to older people looking to get the best sleep possible, seven hours of consistent sleep may be the sweet spot, research suggests. The American Academy of Sleep Medicine advises adults get at least seven hours of sleep per night and teens get eight to 10.
Is there such a thing as too much sleep?
Though many struggle to get enough sleep, it's also possible to get too much.
Harris previously told USA TODAY that "too much" sleep varies for each individual, but more than 10 is likely overboard and can result in feeling "sleep drunk," or especially groggy or foggy, in the morning.
"Some people can feel fine if they’re naturally longer sleepers, but oftentimes people who are very long sleepers don’t usually feel like the sleep is refreshing," she said.
Oversleeping may also be a red flag of an underlying sleep disorder, such as hypersomnia or sleep apnea , Sarah Silverman , a licensed psychologist and behavioral sleep medicine specialist, previously told USA TODAY.
"Sleep is just like shoe size," she said. "One size does not fit all, and some people are going to need more than eight. Some people are going to need less than eight. But really, I'd say that the sweet spot is going to be the number of hours of sleep that allows you to feel your best."
More: Olivia Rodrigo flaunts her sass, sensitivity as GUTS tour returns to the US
Why does getting enough sleep matter?
As people sleep, their brains work to consolidate memories and process things learned during the day, particularly during what's called deep sleep, Barbara Sahakian, a professor in the psychiatry department at the University of Cambridge, previously told USA TODAY.
But too little or too much sleep can create chronic stress. It can also cause changes in the hippocampus, a part of the brain vital to learning and memory, Sahakian said.
More: Olivia Rodrigo's 'Guts' is a no-skip album but these 2 songs are the best of the bunch
How can you improve your sleep?
If you’re looking to improve your nighttime habits and feel well-rested , here are some tips to better your sleep hygiene :
- Stay consistent: A regular bed and wake-up time can help set your biological clock to become sleepy at the same time every day.
- Wind down: A period of “wind-down time” is another step to ensure you’re getting a good quality night of sleep. Try a relaxing meditation, a warm bath or shower, reading, or listening to calming music.
- Establish your sleeping space: The bedroom should be a cool, dark, quiet and comfortable place to ensure the best possible sleep experience. Dark shades and earplugs can help achieve this.
- Avoid alcohol, food, caffeine and electronics before bed: Eating before bed has been known to cause acid reflux, and caffeinated beverages (including soda, coffee, tea and chocolate) may keep you up at night. And while you may be tempted to end the night with a glass of wine, alcohol can impact your sleep. You should also avoid using electronics before bed and even leave them outside of the bedroom.
- Exercise regularly : Several studies have linked increased aerobic exercise and better quality sleep for individuals with insomnia.
Contributing: Saleen Martin, Daryl Austin and Clare Mulroy

COMMENTS
As shown in Figure 2, pooled mean estimates for overnight sleep duration declined from 9.68 hours (3-5 years age band) to 8.98 hours (6-8 years age band), 8.85 hours (9-11 years age band), 8.05 hours (12-14 years age band), and 7.4 hours (15-18 years age band). These normative sleep duration values may aid in the interpretation of ...
On average, how many hours do you sleep each night? For most healthy adults, guidelines suggest at least seven hours of slumber. But these are general recommendations and not strict rules. "Some people need less than seven hours, while others might need more," says Eric Zhou with the Division of Sleep Medicine at Harvard Medical School.
Strategic opportunities in sleep and circadian research: report of the Joint Task Force of the Sleep Research Society and American Academy of Sleep Medicine. Sleep. 2014;37(2):219-227. Crossref Google Scholar; 74. Jackson CL, Walker JR, Brown MK, Das R, Jones NL. A workshop report on the causes and consequences of sleep health disparities. Sleep.
The panel of National Sleep Foundation suggests sleep durations for various age groups and agrees that the appropriate sleep duration for young adults and adults would be 7-9 hours, and for ...
Sleep duration varies widely across the lifespan and shows an inverse relationship with age. Sleep duration recommendations issued by public health authorities are important for surveillance and help to inform the population of interventions, policies, and healthy sleep behaviors. However, the ideal amount of sleep required each night can vary ...
Citation 55, Citation 56 This may explain why the American Academy of Sleep Medicine and the Sleep Research Society recommends a threshold value for adults (≥7 hours per night) rather than a range (eg, 7-9 hours per night) (Table 1). However, excessive long sleep duration may be informative as it can be indicative of poor sleep efficiency ...
9-12 hours. Teen. 13-18 years. 8-10 hours. Adult. 18 years and older. 7 hours or more. Different age groups need different amounts of sleep. In each group, the guidelines present a recommended range of nightly sleep duration for healthy individuals.
Sleep deficit has been associated with lack of concentration and attention during class. 19 While a few studies report null effects, 20,21 most studies looking at the effects of sleep quality and ...
Prior research has found that a country's average bedtime, but not average wake time, predicts sleep duration, and that solar cues do influence sleep but are being attenuated in the real world ...
Americans sleep 6.8 hours per day on average, which hasn't changed much from Gallup polls in the 1990s and 2000s, but is down more than an hour from 1942. 1. 59% of Americans get 7 or more hours of sleep at night. In 1942, 84% met the standard of getting 7-9 hours per night of sleep. 1. The older the age group, the more they report sleeping.
Sleep duration remains steady in recent years with older adults spending on average seven hours sleeping per day [15, 16]. Consistent evidence shows that optimal sleep duration (~ 7 h/night) is ...
8 to 10 hours per 24 hours. Adults. 7 or more hours a night. In addition to age, other factors can affect how many hours of sleep you need. For example: Sleep quality. If your sleep is frequently interrupted, you're not getting quality sleep. The quality of your sleep is just as important as the quantity. Previous sleep deprivation.
Listen to the article. A study of half a million people has led scientists to new insights on the way we sleep. The joint British/Chinese study pinpointed the ideal number of sleep hours we need. Sleep needs vary with age but 7 hours is the ideal in for people aged 38 to 73. Sleeping well can significantly improve physical and mental health.
They were able to track the people who had multiple nights of insufficient sleep (defined as 6 hours of sleep or fewer) to see if their typing speed changed. They found that, on average, one night of insufficient sleep resulted in worse performance for three days, and two nights of insufficient sleep negatively impacted performance for six days.
Seven hours is the ideal amount of sleep for people in their middle age and upwards, with too little or too much little sleep associated with poorer cognitive performance and mental health, say ...
Teenagers: As kids get older, their need for sleep decreases slightly. Teens (14-17 years) require about eight to 10 hours of nightly sleep. Adults: Between the ages of 18 and 64, adults should aim for seven to nine hours of nightly sleep. If you're older than 65, you may need a little less: seven to eight hours is recommended.
In this study, students who wake up well-rested and sleeping 6-7 hours per day have higher sleep quality.These findings also supports the medical literature.According to Karatay et al. , Sari et al. and Vail-Smith and colleagues' studies,smoking students have lower sleep quality compared to non-smokers.It is known that cigarette contains ...
DARIEN, IL - In a new recommendation published in the June issue of SLEEP, the American Academy of Sleep Medicine (AASM) and Sleep Research Society (SRS) recommend that adults obtain seven or more hours of sleep per night to avoid the health risks of chronic inadequate sleep. In addition, the AASM and SRS do not place an upper limit on the number of hours of sleep recommended per night.
But the ideal sleep duration has long been thought to be universal. "There are many people who think everyone needs eight to eight and a half hours of sleep per night and there will be health ...
This study utilized quantitative research design to investigate the relationship of sleeping hours on the academic performance of SHS students during blended learning at NU-Nazareth. It aims to
For the new study, the researchers recorded the neuronal activity of hippocampal neurons in rats that were allowed to move freely through 15 different spatial contexts over 19 ½ hours, a time span that included periods of extended sleep, during a single day.
Sleep specialists offer some advice. Koalas can sleep for 20 hours a day, partly because they have a low-energy diet. Credit: Jens Metschurat/Alamy. Sleep has a profound impact on human health ...
Research shows that sleep efficiency below 80 percent increases mortality risk for older people, and pain, sleep medication use, and bad dreams are the main factors for their poor sleep efficiency ...
hours of sleep on average, mostly due to various activities like social media, video games, and homework (Amenabar, 2023; Creswell et al., 2023). The consequences of insufficient sleep among ...
For example, one-third of the US population reported not getting the recommended 7 to 9 hours of sleep per night. 2-4 Substantial evidence suggests that sleeping less than 7 hours per night on a regular basis is associated with adverse health consequences. 5 Particularly, insufficient sleep duration has been increasingly recognized as an ...
The result helps explain why all animals require sleep, not only to fix memories, but also to reset the brain and keep it working during waking hours. "We show that memory is a dynamic process ...
Expert-level sleep staging using an electrocardiography-only feed-forward neural network. Computers in Biology and Medicine , 2024; 176: 108545 DOI: 10.1016/j.compbiomed.2024.108545
Sleep deprivation is a real problem that many adults struggle with. More than one-third of adults in America consistently sleep less than seven hours per night, according to a 2016 study. Sleep ...
Chronic sleep deprivation can harm brain, metabolic and immune health. People ages 18 to 64 should have 7 to 9 hours of sleep per night, according to the BHC.
How much sleep should you get, according to research? For middle-aged to older people looking to get the best sleep possible, seven hours of consistent sleep may be the sweet spot, research suggests.