- Research article
- Open access
- Published: 24 October 2019

A scoping review of the literature on the current mental health status of physicians and physicians-in-training in North America
- Mara Mihailescu ORCID: orcid.org/0000-0001-6878-1024 1 &
- Elena Neiterman 2
BMC Public Health volume 19 , Article number: 1363 ( 2019 ) Cite this article
28k Accesses
70 Citations
11 Altmetric
Metrics details
This scoping review summarizes the existing literature regarding the mental health of physicians and physicians-in-training and explores what types of mental health concerns are discussed in the literature, what is their prevalence among physicians, what are the causes of mental health concerns in physicians, what effects mental health concerns have on physicians and their patients, what interventions can be used to address them, and what are the barriers to seeking and providing care for physicians. This review aims to improve the understanding of physicians’ mental health, identify gaps in research, and propose evidence-based solutions.
A scoping review of the literature was conducted using Arksey and O’Malley’s framework, which examined peer-reviewed articles published in English during 2008–2018 with a focus on North America. Data were summarized quantitatively and thematically.
A total of 91 articles meeting eligibility criteria were reviewed. Most of the literature was specific to burnout ( n = 69), followed by depression and suicidal ideation ( n = 28), psychological harm and distress ( n = 9), wellbeing and wellness ( n = 8), and general mental health ( n = 3). The literature had a strong focus on interventions, but had less to say about barriers for seeking help and the effects of mental health concerns among physicians on patient care.
Conclusions
More research is needed to examine a broader variety of mental health concerns in physicians and to explore barriers to seeking care. The implication of poor physician mental health on patients should also be examined more closely. Finally, the reviewed literature lacks intersectional and longitudinal studies, as well as evaluations of interventions offered to improve mental wellbeing of physicians.
Peer Review reports
The World Health Organization (WHO) defines mental health as “a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community.” [ 41 ] One in four people worldwide are affected by mental health concerns [ 40 ]. Physicians are particularly vulnerable to experiencing mental illness due to the nature of their work, which is often stressful and characterized by shift work, irregular work hours, and a high pressure environment [ 1 , 21 , 31 ]. In North America, many physicians work in private practices with no access to formal institutional supports, which can result in higher instances of social isolation [ 13 , 27 ]. The literature on physicians’ mental health is growing, partly due to general concerns about mental wellbeing of health care workers and partly due to recognition that health care workers globally are dissatisfied with their work, which results in burnout and attrition from the workforce [ 31 , 34 ]. As a consequence, more efforts have been made globally to improve physicians’ mental health and wellness, which is known as “The Quadruple Aim.” [ 34 ] While the literature on mental health is flourishing, however, it has not been systematically summarized. This makes it challenging to identify what is being done to improve physicians’ wellbeing and which solutions are particularly promising [ 7 , 31 , 33 , 37 , 38 ]. The goal of our paper is to address this gap.
This paper explores what is known from the existing peer-reviewed literature about the mental health status of physicians and physicians-in-training in North America. Specifically, we examine (1) what types of mental health concerns among physicians are commonly discussed in the literature; (2) what are the reported causes of mental health concerns in physicians; (3) what are the effects that mental health concerns may have on physicians and their patients; (4) what solutions are proposed to improve mental health of physicians; and (5) what are the barriers to seeking and providing care to physicians with mental health concerns. Conducting this scoping review, our goal is to summarize the existing research, identifying the need for a subsequent systematic review of the literature in one or more areas under the study. We also hope to identify evidence-based interventions that can be utilized to improve physicians’ mental wellbeing and to suggest directions for future research [ 2 ]. Evidence-based interventions might have a positive impact on physicians and improve the quality of patient care they provide.
A scoping review of the academic literature on the mental health of physicians and physicians-in-training in North America was conducted using Arksey and O’Malley’s [ 2 ] methodological framework. Our review objectives and broad focus, including the general questions posed to conduct the review, lend themselves to a scoping review approach, which is suitable for the analysis of a broader range of study designs and methodologies [ 2 ]. Our goal was to map the existing research on this topic and identify knowledge gaps, without making any prior assumptions about the literature’s scope, range, and key findings [ 29 ].
Stage 1: identify the research question
Following the guidelines for scoping reviews [ 2 ], we developed a broad research question for our literature search, asking what does the academic literature tell about mental health issues among physicians, residents, and medical students in North America ? Burnout and other mental health concerns often begin in medical training and continue to worsen throughout the years of practice [ 31 ]. Recognizing that the study and practice of medicine plays a role in the emergence of mental health concerns, we focus on practicing physicians – general practitioners, specialists, and surgeons – and those who are still in training – residents and medical students. We narrowed down the focus of inquiry by asking the following sub-questions:
What types of mental health concerns among physicians are commonly discussed in the literature?
What are the reported causes of mental health problems in physicians and what solutions are available to improve the mental wellbeing of physicians?
What are the barriers to seeking and providing care to physicians suffering from mental health problems?
Stage 2: identify the relevant studies
We included in our review empirical papers published during January 2008–January 2018 in peer-reviewed journals. Our exclusive focus on peer-reviewed and empirical literature reflected our goal to develop an evidence-based platform for understanding mental health concerns in physicians. Since our focus was on prevalence of mental health concerns and promising practices available to physicians in North America, we excluded articles that were more than 10 years old, suspecting that they might be too outdated for our research interest. We also excluded papers that were not in English or outside the region of interest. Using combinations of keywords developed in consultation with a professional librarian (See Table 1 ), we searched databases PUBMed, SCOPUS, CINAHL, and PsychNET. We also screened reference lists of the papers that came up in our original search to ensure that we did not miss any relevant literature.
Stage 3: literature selection
Publications were imported into a reference manager and screened for eligibility. During initial abstract screening, 146 records were excluded for being out of scope, 75 records were excluded for being outside the region of interest, and 4 papers were excluded because they could not be retrieved. The remaining 91 papers were included into the review. Figure 1 summarizes the literature search and selection.
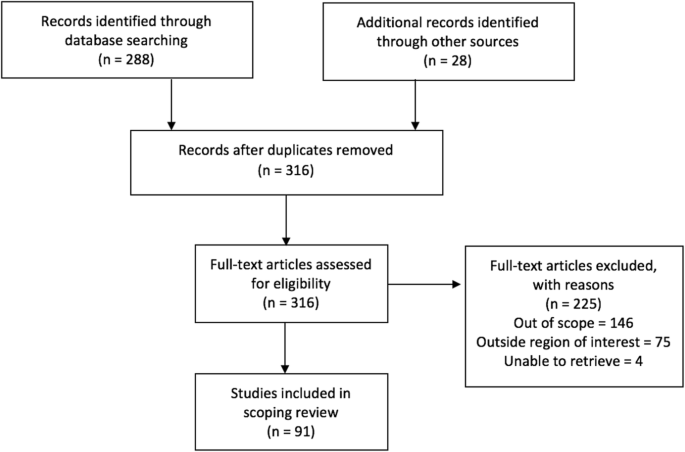
PRISMA Flow Diagram
Stage 4: charting the data
A literature extraction tool was created in Microsoft Excel to record the author, date of publication, location, level of training, type of article (empirical, report, commentary), and topic. Both authors coded the data inductively, first independently reading five articles and generating themes from the data, then discussing our coding and developing a coding scheme that was subsequently applied to ten more papers. We then refined and finalized the coding scheme and used it to code the rest of the data. When faced with disagreements on narrowing down the themes, we discussed our reasoning and reached consensus.
Stage 5: collating, summarizing, and reporting the results
The data was summarized by frequency and type of publication, mental health topics, and level of training. The themes inductively derived from the data included (1) description of mental health concerns affecting physicians and physicians-in-training; (2) prevalence of mental health concerns among this population; (3) possible causes that can explain the emergence of mental health concerns; (4) solutions or interventions proposed to address mental health concerns; (5) effects of mental health concerns on physicians and on patient outcomes; and (6) barriers for seeking and providing help to physicians afflicted with mental health concerns. Each paper was coded based on its relevance to major theme(s) and, if warranted, secondary focus. Therefore, one paper could have been coded in more than one category. Upon analysis, we identified the gaps in the literature.
Characteristics of included literature
The initial search yielded 316 records of which 91 publications underwent full-text review and were included in our scoping review. Our analysis revealed that the publications appear to follow a trend of increase over the course of the last decade reflecting the growing interest in physicians’ mental health. More than half of the literature was published in the last 4 years included in the review, from 2014 to 2018 ( n = 55), with most publications in 2016 ( n = 18) (Fig. 2 ). The majority of papers ( n = 36) focused on practicing physicians, followed by papers on residents ( n = 22), medical students ( n = 21), and those discussing medical professionals with different level of training ( n = 12). The types of publications were mostly empirical ( n = 71), of which 46 papers were quantitative. Furthermore, the vast majority of papers focused on the United States of America (USA) ( n = 83), with less than 9% focusing on Canada ( n = 8). The frequency of identified themes in the literature is broken down into prevalence of mental health concerns ( n = 15), causes of mental health concerns ( n = 18), effects of mental health concerns on physicians and patients ( n = 12), solutions and interventions for mental health concerns ( n = 46), and barriers to seeking and providing care for mental health concerns ( n = 4) (Fig. 3 ).
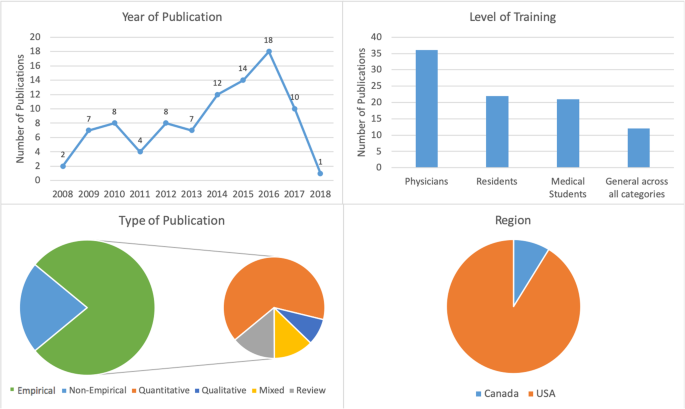
Number of sources by characteristics of included literature
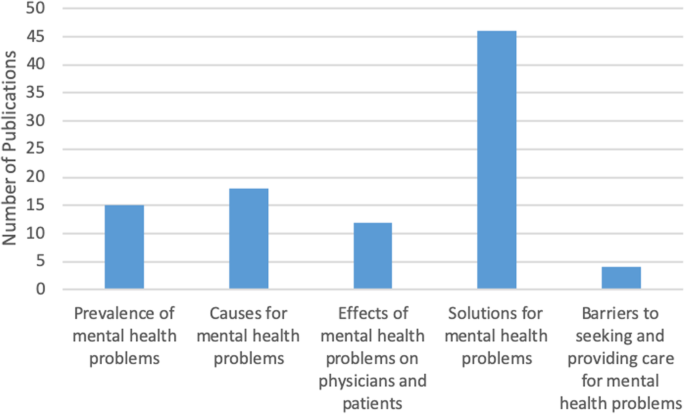
Frequency of themes in literature ( n = 91)
Mental health concerns and their prevalence in the literature
In this thematic category ( n = 15), we coded the papers discussing the prevalence of specific mental health concerns among physicians and those comparing physicians’ mental health to that of the general population. Most papers focused on burnout and stress ( n = 69), which was followed by depression and suicidal ideation ( n = 28), psychological harm and distress ( n = 9), wellbeing and wellness ( n = 8), and general mental health ( n = 3) (Fig. 4 ). The literature also identified that, on average, burnout and mental health concerns affect 30–60% of all physicians and residents [ 4 , 5 , 8 , 9 , 15 , 25 , 26 ].
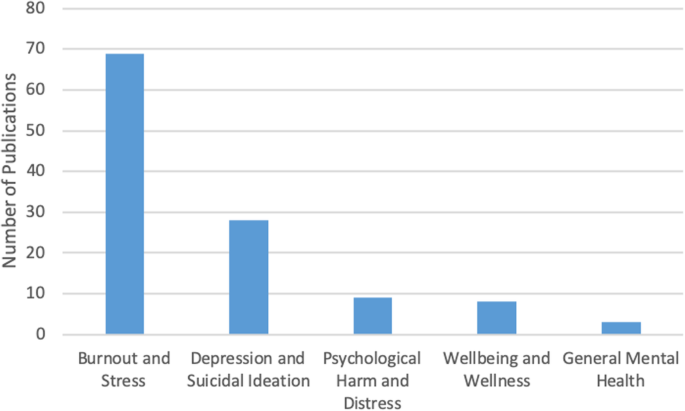
Number of sources by mental health topic discussed ( n = 91)
There was some overlap between the papers discussing burnout, depression, and suicidal ideation, suggesting that work-related stress may lead to the emergence of more serious mental health problems [ 3 , 12 , 21 ], as well as addiction and substance abuse [ 22 , 27 ]. Residency training was shown to produce the highest rates of burnout [ 4 , 8 , 19 ].
Causes of mental health concerns
Papers discussing the causes of mental health concerns in physicians formed the second largest thematic category ( n = 18). Unbalanced schedules and increasing administrative work were defined as key factors in producing poor mental health among physicians [ 4 , 5 , 6 , 13 , 15 , 27 ]. Some papers also suggested that the nature of the medical profession itself – competitive culture and prioritizing others – can lead to the emergence of mental health concerns [ 23 , 27 ]. Indeed, focus on qualities such as rigidity, perfectionism, and excessive devotion to work during the admission into medical programs fosters the selection of students who may be particularly vulnerable to mental illness in the future [ 21 , 24 ]. The third cluster of factors affecting mental health stemmed from structural issues, such as pressure from the government and insurance, fragmentation of care, and budget cuts [ 13 , 15 , 18 ]. Work overload, lack of control over work environment, lack of balance between effort and reward, poor sense of community among staff, lack of fairness and transparency by decision makers, and dissonance between one’s personal values and work tasks are the key causes for mental health concerns among physicians [ 20 ]. Govardhan et al. conceptualized causes for mental illness as having a cyclical nature - depression leads to burnout and depersonalization, which leads to patient dissatisfaction, causing job dissatisfaction and more depression [ 19 ].
Effects of mental health concerns on physicians and patients
A relatively small proportion of papers (13%) discussed the effects of mental health concerns on physicians and patients. The literature prioritized the direct effect of mental health on physicians ( n = 11) with only one paper focusing solely on the indirect effects physicians’ mental health may have on patients. Poor mental health in physicians was linked to decreased mental and physical health [ 3 , 14 , 15 ]. In addition, mental health concerns in physicians were associated with reduction in work hours and the number of patients seen, decrease in job satisfaction, early retirement, and problems in personal life [ 3 , 5 , 15 ]. Lu et al. found that poor mental health in physicians may result in increased medical errors and the provision of suboptimal care [ 25 ]. Thus physicians’ mental wellbeing is linked to the quality of care provided to patients [ 3 , 4 , 5 , 10 , 17 ].
Solutions and interventions
In this largest thematic category ( n = 46) we coded the literature that offered solutions for improving mental health among physicians. We identified four major levels of interventions suggested in the literature. A sizeable proportion of literature discussed the interventions that can be broadly categorized as primary prevention of mental illness. These papers proposed to increase awareness of physicians’ mental health and to develop strategies that can help to prevent burnout from occurring in the first place [ 4 , 12 ]. Some literature also suggested programs that can help to increase resilience among physicians to withstand stress and burnout [ 9 , 20 , 27 ]. We considered the papers referring to the strategies targeting physicians currently suffering from poor mental health as tertiary prevention . This literature offered insights about mindfulness-based training and similar wellness programs that can increase self-awareness [ 16 , 18 , 27 ], as well as programs aiming to improve mental wellbeing by focusing on physical health [ 17 ].
While the aforementioned interventions target individual physicians, some literature proposed workplace/institutional interventions with primary focus on changing workplace policies and organizational culture [ 4 , 13 , 23 , 25 ]. Reducing hours spent at work and paperwork demands or developing guidelines for how long each patient is seen have been identified by some researchers as useful strategies for improving mental health [ 6 , 11 , 17 ]. Offering access to mental health services outside of one’s place of employment or training could reduce the fear of stigmatization at the workplace [ 5 , 12 ]. The proposals for cultural shift in medicine were mainly focused on promoting a less competitive culture, changing power dynamics between physicians and physicians-in-training, and improving wellbeing among medical students and residents. The literature also proposed that the medical profession needs to put more emphasis on supporting trainees, eliminating harassment, and building strong leadership [ 23 ]. Changing curriculum for medical students was considered a necessary step for the cultural shift [ 20 ]. Finally, while we only reviewed one paper that directly dealt with the governmental level of prevention, we felt that it necessitated its own sub-thematic category because it identified the link between government policy, such as health care reforms and budget cuts, and the services and care physicians can provide to their patients [ 13 ].
Barriers to seeking and providing care
Only four papers were summarized in this thematic category that explored what the literature says about barriers for seeking and providing care for physicians suffering from mental health concerns. Based on our analysis, we identified two levels of factors that can impact access to mental health care among physicians and physicians-in-training.
Individual level barriers stem from intrinsic barriers that individual physicians may experience, such as minimizing the illness [ 21 ], refusing to seek help or take part in wellness programs [ 14 ], and promoting the culture of stoicism [ 27 ] among physicians. Another barrier is stigma associated with having a mental illness. Although stigma might be experienced personally, literature suggests that acknowledging the existence of mental health concerns may have negative consequences for physicians, including loss of medical license, hospital privileges, or professional advancement [ 10 , 21 , 27 ].
Structural barriers refer to the lack of formal support for mental wellbeing [ 3 ], poor access to counselling [ 6 ], lack of promotion of available wellness programs [ 10 ], and cost of treatment. Lack of research that tests the efficacy of programs and interventions aiming to improve mental health of physicians makes it challenging to develop evidence-based programs that can be implemented at a wider scale [ 5 , 11 , 12 , 18 , 20 ].
Our analysis of the existing literature on mental health concerns in physicians and physicians-in-training in North America generated five thematic categories. Over half of the reviewed papers focused on proposing solutions, but only a few described programs that were empirically tested and proven to work. Less common were papers discussing causes for deterioration of mental health in physicians (20%) and prevalence of mental illness (16%). The literature on the effects of mental health concerns on physicians and patients (13%) focused predominantly on physicians with only a few linking physicians’ poor mental health to medical errors and decreased patient satisfaction [ 3 , 4 , 16 , 24 ]. We found that the focus on barriers for seeking and receiving help for mental health concerns (4%) was least prevalent. The topic of burnout dominated the literature (76%). It seems that the nature of physicians’ work fosters the environment that causes poor mental health [ 1 , 21 , 31 ].
While emphasis on burnout is certainly warranted, it might take away the attention paid to other mental health concerns that carry more stigma, such as depression or anxiety. Establishing a more explicit focus on other mental health concerns might promote awareness of these problems in physicians and reduce the fear such diagnosis may have for doctors’ job security [ 10 ]. On the other hand, utilizing the popularity and non-stigmatizing image of “burnout” might be instrumental in developing interventions promoting mental wellbeing among a broad range of physicians and physicians-in-training.
Table 2 summarizes the key findings from the reviewed literature that are important for our understanding of physician mental health. In order to explicitly summarize the gaps in the literature, we mapped them alongside the areas that have been relatively well studied. We found that although non-empirical papers discussed physicians’ mental wellbeing broadly, most empirical papers focused on medical specialty (e.g. neurosurgeons, family medicine, etc.) [ 4 , 8 , 15 , 19 , 25 , 28 , 35 , 36 ]. Exclusive focus on professional specialty is justified if it features a unique context for generation of mental health concerns, but it limits the ability to generalize the findings to a broader population of physicians. Also, while some papers examined the impact of gender on mental health [ 7 , 32 , 39 ], only one paper considered ethnicity as a potential factor for mental health concerns and found no association [ 4 ]. Given that mental health in the general population varies by gender, ethnicity, age, and sexual orientation, it would be prudent to examine mental health among physicians using an intersectional analysis [ 30 , 32 , 39 ]. Finally, of the empirical studies we reviewed, all but one had a cross-sectional design. Longitudinal design might offer a better understanding of the emergence and development of mental health concerns in physicians and tailor interventions to different stages of professional career. Additionally, it could provide an opportunity to evaluate programs’ and policies’ effectiveness in improving physicians’ mental health. This would also help to address the gap that we identified in the literature – an overarching focus on proposing solutions with little demonstrated evidence they actually work.
This review has several limitations. First, our focus on academic literature may have resulted in overlooking the papers that are not peer-reviewed but may provide interesting solutions to physician mental health concerns. It is possible that grey literature – reports and analyses published by government and professional organizations – offers possible solutions that we did not include in our analysis or offers a different view on physicians’ mental health. Additionally, older papers and papers not published in English may have information or interesting solutions that we did not include in our review. Second, although our findings suggest that the theme of burnout dominated the literature, this may be the result of the search criteria we employed. Third, following the scoping review methodology [ 2 ], we did not assess the quality of the papers, focusing instead on the overview of the literature. Finally, our research was restricted to North America, specifically Canada and the USA. We excluded Mexico because we believed that compared to the context of medical practice in Canada and the USA, which have some similarities, the work experiences of Mexican physicians might be different and the proposed solutions might not be readily applicable to the context of practice in Canada and the USA. However, it is important to note that differences in organization of medical practice in Canada and the USA do exist, as do differences across and within provinces in Canada and the USA. A comparative analysis can shed light on how the structure and organization of medical practice shapes the emergence of mental health concerns.
The scoping review we conducted contributes to the existing research on mental wellbeing of American and Canadian physicians by summarizing key knowledge areas and identifying key gaps and directions for future research. While the papers reviewed in our analysis focused on North America, we believe that they might be applicable to the global medical workforce. Identifying key gaps in our knowledge, we are calling for further research on these topics, including examination of medical training curricula and its impact on mental wellbeing of medical students and residents, research on common mental health concerns such as depression or anxiety, studies utilizing intersectional and longitudinal approaches, and program evaluations assessing the effectiveness of interventions aiming to improve mental wellbeing of physicians. Focus on the effect physicians’ mental health may have on the quality of care provided to patients might facilitate support from government and policy makers. We believe that large-scale interventions that are proven to work effectively can utilize an upstream approach for improving the mental health of physicians and physicians-in-training.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
United States of America
World Health Organization
Ahmed N, Devitt KS, Keshet I, Spicer J, Imrie K, Feldman L, et al. A systematic review of the effects of resident duty hour restrictions in surgery: impact on resident wellness, training, and patient outcomes. Ann Surg. 2014;259(6):1041–53.
Article Google Scholar
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Atallah F, McCalla S, Karakash S, Minkoff H. Please put on your own oxygen mask before assisting others: a call to arms to battle burnout. Am J Obstet Gynecol. 2016;215(6):731.e1.
Baer TE, Feraco AM, Tuysuzoglu Sagalowsky S, Williams D, Litman HJ, Vinci RJ. Pediatric resident burnout and attitudes toward patients. Pediatrics. 2017;139(3):e20162163. https://doi.org/10.1542/peds.2016-2163 .
Article PubMed Google Scholar
Blais R, Safianyk C, Magnan A, Lapierre A. Physician, heal thyself: survey of users of the Quebec physicians health program. Can Fam Physician. 2010;56(10):e383–9.
PubMed PubMed Central Google Scholar
Brennan J, McGrady A. Designing and implementing a resiliency program for family medicine residents. Int J Psychiatry Med. 2015;50(1):104–14.
Cass I, Duska LR, Blank SV, Cheng G, NC dP, Frederick PJ, et al. Stress and burnout among gynecologic oncologists: a Society of Gynecologic Oncology Evidence-based Review and Recommendations. Gynecol Oncol. 2016;143(2):421–7.
Chan AM, Cuevas ST, Jenkins J 2nd. Burnout among osteopathic residents: a cross-sectional analysis. J Am Osteopath Assoc. 2016;116(2):100–5.
Chaukos D, Chad-Friedman E, Mehta DH, Byerly L, Celik A, McCoy TH Jr, et al. Risk and resilience factors associated with resident burnout. Acad Psychiatry. 2017;41(2):189–94.
Compton MT, Frank E. Mental health concerns among Canadian physicians: results from the 2007-2008 Canadian physician health study. Compr Psychiatry. 2011;52(5):542–7.
Cunningham C, Preventing MD. Burnout. Trustee. 2016;69(2):6–7 1.
PubMed Google Scholar
Daskivich TJ, Jardine DA, Tseng J, Correa R, Stagg BC, Jacob KM, et al. Promotion of wellness and mental health awareness among physicians in training: perspective of a national, multispecialty panel of residents and fellows. J Grad Med Educ. 2015;7(1):143–7.
Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA. 2011;305(19):2009–10.
Article CAS Google Scholar
Epstein RM, Krasner MS. Physician resilience: what it means, why it matters, and how to promote it. Acad Med. 2013;88(3):301–3.
Evans RW, Ghosh K. A survey of headache medicine specialists on career satisfaction and burnout. Headache. 2015;55(10):1448–57.
Fahrenkopf AM, Sectish TC, Barger LK, Sharek PJ, Lewin D, Chiang VW, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336(7642):488–91.
Fargen KM, Spiotta AM, Turner RD, Patel S. The importance of exercise in the well-rounded physician: dialogue for the inclusion of a physical fitness program in neurosurgery resident training. World Neurosurg. 2016;90:380–4.
Gabel S. Demoralization in Health Professional Practice: Development, Amelioration, and Implications for Continuing Education. J Contin Educ Health Prof 2013 Spring. 2013;33(2):118–26.
Google Scholar
Govardhan LM, Pinelli V, Schnatz PF. Burnout, depression and job satisfaction in obstetrics and gynecology residents. Conn Med. 2012;76(7):389–95.
Jennings ML, Slavin SJ. Resident wellness matters: optimizing resident education and wellness through the learning environment. Acad Med. 2015;90(9):1246–50.
Keller EJ. Philosophy in medical education: a means of protecting mental health. Acad Psychiatry. 2014;38(4):409–13.
Krall EJ, Niazi SK, Miller MM. The status of physician health programs in Wisconsin and north central states: a look at statewide and health systems programs. WMJ. 2012;111(5):220–7.
Lemaire JB, Wallace JE. Burnout among doctors. BMJ. 2017;358:j3360.
Linzer M, Bitton A, Tu SP, Plews-Ogan M, Horowitz KR, Schwartz MD, et al. The end of the 15-20 minute primary care visit. J Gen Intern Med. 2015;30(11):1584–6.
Lu DW, Dresden S, McCloskey C, Branzetti J, Gisondi MA. Impact of burnout on self-reported patient care among emergency physicians. West J Emerg Med. 2015;16(7):996–1001.
Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422.
McClafferty H, Brown OW. Section on integrative medicine, committee on practice and ambulatory medicine, section on integrative medicine. Physician health and wellness. Pediatrics. 2014;134(4):830–5.
Miyasaki JM, Rheaume C, Gulya L, Ellenstein A, Schwarz HB, Vidic TR, et al. Qualitative study of burnout, career satisfaction, and well-being among US neurologists in 2016. Neurology. 2017;89(16):1730–8.
Peterson J, Pearce P, Ferguson LA, Langford C. Understanding scoping reviews: definition, purpose, and process. JAANP. 2016;29:12–6.
Przedworski JM, Dovidio JF, Hardeman RR, Phelan SM, Burke SE, Ruben MA, et al. A comparison of the mental health and well-being of sexual minority and heterosexual first-year medical students: a report from the medical student CHANGE study. Acad Med. 2015;90(5):652–9.
Ripp JA, Privitera MR, West CP, Leiter R, Logio L, Shapiro J, et al. Well-being in graduate medical education: a call for action. Acad Med. 2017;92(7):914–7.
Salles A, Mueller CM, Cohen GL. Exploring the relationship between stereotype perception and Residents’ well-being. J Am Coll Surg. 2016;222(1):52–8.
Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH. A systematic review of stress-management programs for medical students. Acad Psychiatry. 2013;37(3):158–64.
Sikka R, Morath J, Leape L. The quadruple aim: care, health, cost and meaning in work. BMJ Qual Saf. 2015;24(10):608–10. https://doi.org/10.1136/bmjqs-2015-004160 .
Tawfik DS, Phibbs CS, Sexton JB, Kan P, Sharek PJ, Nisbet CC, et al. Factors Associated With Provider Burnout in the NICU. Pediatrics. 2017;139(5):608. https://doi.org/10.1542/peds.2016-4134 Epub 2017 Apr 18.
Turner TB, Dilley SE, Smith HJ, Huh WK, Modesitt SC, Rose SL, et al. The impact of physician burnout on clinical and academic productivity of gynecologic oncologists: a decision analysis. Gynecol Oncol. 2017;146(3):642–6.
West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272.
Williams D, Tricomi G, Gupta J, Janise A. Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry. 2015;39(1):47–54.
Woodside JR, Miller MN, Floyd MR, McGowen KR, Pfortmiller DT. Observations on burnout in family medicine and psychiatry residents. Acad Psychiatry. 2008;32(1):13–9.
World Health Organization. (2001). Mental disorders affect one in four people.
World Health Organization. Promoting mental health: concepts, emerging evidence, practice (Summary Report). Geneva: World Health Organization; 2004.
Download references
Acknowledgements
Not Applicable.
Not Applicable
Author information
Authors and affiliations.
Telfer School of Management, University of Ottawa, 55 Laurier Ave E, Ottawa, ON, K1N 6N5, Canada
Mara Mihailescu
School of Public Health and Health Systems, University of Waterloo, 200 University Avenue West, Waterloo, ON, N2L 3G1, Canada
Elena Neiterman
You can also search for this author in PubMed Google Scholar
Contributions
M.M. and E.N. were involved in identifying the relevant research question and developing the combinations of keywords used in consultation with a professional librarian. M.M. performed the literature selection and screening of references for eligibility. Both authors were involved in the creation of the literature extraction tool in Excel. Both authors coded the data inductively, first independently reading five articles and generating themes from the data, then discussing their coding and developing a coding scheme that was subsequently applied to ten more papers. Both authors then refined and finalized the coding scheme and M.M. used it to code the rest of the data. M.M. conceptualized and wrote the first copy of the manuscript, followed by extensive drafting by both authors. E.N. was a contributor to writing the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Mara Mihailescu .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Mihailescu, M., Neiterman, E. A scoping review of the literature on the current mental health status of physicians and physicians-in-training in North America. BMC Public Health 19 , 1363 (2019). https://doi.org/10.1186/s12889-019-7661-9
Download citation
Received : 29 April 2019
Accepted : 20 September 2019
Published : 24 October 2019
DOI : https://doi.org/10.1186/s12889-019-7661-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Mental illness
- Medical students
- Scoping review
- Interventions
- North America
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Systematic Review
- Open access
- Published: 20 August 2024
Examining the mental health services among people with mental disorders: a literature review
- Yunqi Gao 1 ,
- Richard Burns 1 ,
- Liana Leach 1 ,
- Miranda R. Chilver 1 &
- Peter Butterworth 2 , 3
BMC Psychiatry volume 24 , Article number: 568 ( 2024 ) Cite this article
1188 Accesses
1 Altmetric
Metrics details
Mental disorders are a significant contributor to disease burden. However, there is a large treatment gap for common mental disorders worldwide. This systematic review summarizes the factors associated with mental health service use.
PubMed, Scopus, and the Web of Science were searched for articles describing the predictors of and barriers to mental health service use among people with mental disorders from January 2012 to August 2023. The initial search yielded 3230 articles, 2366 remained after removing duplicates, and 237 studies remained after the title and abstract screening. In total, 40 studies met the inclusion and exclusion criteria.
Middle-aged participants, females, Caucasian ethnicity, and higher household income were more likely to access mental health services. The use of services was also associated with the severity of mental symptoms. The association between employment, marital status, and mental health services was inconclusive due to limited studies. High financial costs, lack of transportation, and scarcity of mental health services were structural factors found to be associated with lower rates of mental health service use. Attitudinal barriers, mental health stigma, and cultural beliefs also contributed to the lower rates of mental health service use.
This systematic review found that several socio-demographic characteristics were strongly associated with using mental health services. Policymakers and those providing mental health services can use this information to better understand and respond to inequalities in mental health service use and improve access to mental health treatment.
Peer Review reports
Introduction
Mental disorders such as depression and anxiety are prevalent, with nationally representative studies showing that one-fifth of Australians experience a mental disorder each year [ 5 ]. More recent estimates derived from a similar survey during the period of the COVID-19 pandemic were 21.5% [ 11 ]. Mental illness can reduce the quality of life, and increase the likelihood of communicable and non-communicable diseases [ 116 , 137 ], and is among the costliest burdens in developed countries [ 22 , 34 , 80 ]. The National Mental Health Commission [ 96 ] stated that the annual cost of mental ill-health in Australia was around $4000 per person or $60 billion. The Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019 reported that mental disorders rank the seventh leading cause of disability-adjusted life years and the second leading cause of years lived with disability [ 48 ]. Helliwell et al. [ 56 ] indicated that chronic mental illness was a key determinant of unhappiness, and it triggered more pain than physical illness. Mental health issues can have a spillover effect on all areas of life, poor mental health conditions might lead to lower educational achievements and work performance, substance abuse, and violence [ 102 ]. In Australia, despite considerable additional investment in the provision of mental health services research suggests that the rate of psychological distress at the population level has been increasing [ 38 ], this has been argued to reflect that people who most need mental health treatment are not accessing services. Insufficient numbers of mental health services and mental healthcare professionals and inadequate health literacy have been reported as the pivotal determinants of poor mental health [ 18 ]. Previous studies have reported large treatment gaps in mental health services; finding only 42–44% of individuals with mental illness seek help from any medical or professional service provider [ 85 , 112 ] and this active proportion was much lower in low and middle-income countries [ 32 , 114 , 130 ].
Several studies have investigated factors associated with high and low rates of mental health service use and identified potential barriers to accessing mental health service use. Demographic, social, and structural factors have been associated with low rates of mental health service use. Structural barriers include the availability of mental health services and high treatment costs, social barriers to treatment access include stigma around mental health [ 125 ], fear of being perceived as weak or stigmatized [ 79 ], lack of awareness of mental disorders, and cultural stigma [ 17 ].
Existing studies that have systematically reviewed and evaluated the literature examining mental health service use have largely been constrained to specific population groups such as military service members [ 63 ] and immigrants [ 33 ], children and adolescents [ 35 ], young adults [ 76 ], and help-seeking among Filipinos in the Philippines [ 93 ]. These systematic reviews emphasize mental health service use by specific age groups or sub-groups, and the findings might not represent the patterns and barriers to mental health service use in the general population. One paper has reviewed mental health service use in the general adult population. Roberts et al. [ 112 ] found that need factors (e.g. health status, disability, duration of symptoms) were the strongest determinants of health service use for those with mental disorders.
The study results from Roberts et al. [ 112 ] were retrieved in 2016, and the current study seeks to build on this prior review with more recent research data by identifying publications since 2012 on mental health service use with a focus on high-income countries. This is in the context of ongoing community discussion and reform of the design and delivery of mental health services in Australia [ 140 ], and the need for current evidence to inform this discussion in Australia and other high-income countries. This systematic review aims to investigate factors associated with mental health service use among people with mental disorders and summarize the major barriers to mental health treatment. The specific objectives are (1) to identify factors associated with mental health service use among people with mental disorders in high-income countries, and (2) to identify commonly reported barriers to mental health service use.
Methodology
Selection procedures.
Our review adhered to PRISMA guidelines to present the results. We utilized PubMed, Scopus, and the Web of Science to search for articles describing the facilitators and barriers to mental health service use among people with mental illness from January 2012 up to August 2023. There were no specific factors that were of interest as part of conducting this systematic review, instead, the review had a broad focus intending to identify factors shown to be associated with mental health service use in the recent literature. The keywords used in our search of electronic databases were related to mental disorders and mental health service use. The full search terms and strategies were shown in Supplementary Table 1. We uploaded the search results to Covidence for deduplication and screening. After eliminating duplicates, the first author retrieved the title abstract and full-text articles for all eligible papers. Then each title and abstract were screened by two independent reviewers, to select those that would progress to full-text review. Subsequently, the two reviewers screened the full text of all the selected papers and conducted the data extraction for those that met the eligibility criteria. There were discrepancies in 12% of the papers reviewed, and all conflicts were resolved through discussion and agreed on by at least three authors.
Selection criteria
Inclusion and exclusion criteria.
In this systematic review, the scope was restricted to studies that draw samples from the general population, and the participants were either diagnosed with mental disorders or screened positive using a standardized scale. Case-control studies and cohort studies were considered for inclusion. The applied inclusion and exclusion criteria are listed in Table 1 .
Data extraction
After the full-text screening, details from all eligible studies were extracted by field into a data extraction table with thematic headings. The descriptive data includes the study title, author, publication year, geographic location, sample size, population details (gender, age), type of study design, mental disorder type (medical diagnosis or using scales) and quality grade (e.g. good, fair, and poor).
Quality assessment
The Newcastle Ottawa Scale [ 136 ] was used to evaluate the study quality for all eligible papers. We assessed the cross-sectional and cohort studies using separate assessment forms and graded each study as good, fair, or poor. The quality grade for each study was included in the data extraction table. The first author conducted the quality assessment using the Newcastle Ottawa Scale for cohort studies and the adapted scale for cross-sectional studies.
The search process is summarized in Fig. 1 . The initial search from PubMed, Scopus, and the Web of Science yielded 3230 articles: 2366 remained after removing duplicates; 2129 studies were considered not relevant; and 237 studies remained following title and abstract screening. In total, 40 studies met the inclusion criteria. Of these, four were cohort studies while thirty-six were cross-sectional studies. Ten studies (25.0%) were conducted in Canada, and nine (22.5%) were from the United States. Three studies used data from Germany (7.5%). Two studies each reported data from Australia, Denmark, Sweden, Singapore, or South Korea (5.0% of studies for each country). A single study was included with data from either the United Kingdom, Italy, Israel, Portugal, Switzerland, Chile, New Zealand, or reported pooled multinational data from six European countries (each country/ study representing 2.5% of the total sample of studies) (Table 2 ).
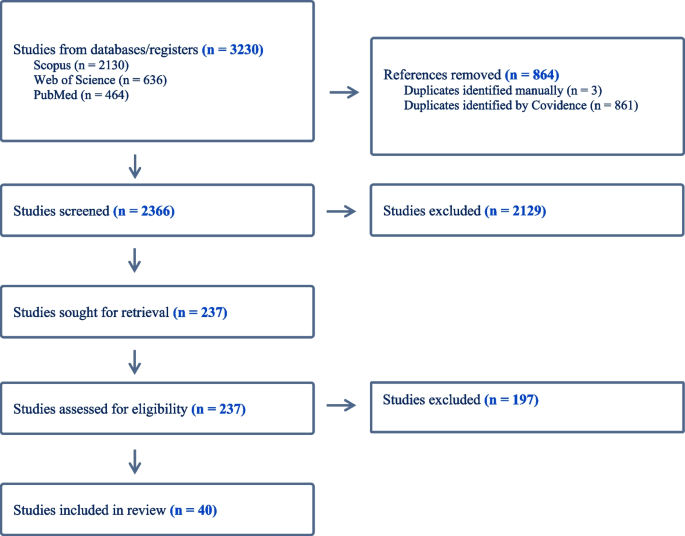
Flowchart for selections of studies
Study characteristics
As shown in Tables 2 , 3 and 4 , the sample size of studies varies; a cross-sectional study from Canada had the largest sample which contained over seven million participants [ 39 ], while the smallest sample size was 362 [ 100 ]. Sixteen studies (40.0%) used DSM-IV diagnoses [ 4 ] to measure mental disorders, twelve studies (30.0%) applied the International Classification of Disease [ 138 ], and six studies used (15.0%) the Kessler Psychological Distress Scale [ 69 ]. Only three studies (7.5%) had a hospital diagnosis of mental disorders, while three studies (7.5%) used the Patient Health Questionnaire [ 72 ] to define mental disorders.
Twenty-seven studies (67.5%) analyzed the rate of mental health service use over the last 12 months, six studies (15.0%) focused on lifetime service use, and three studies (7.5%) assessed both 12-month and lifetime mental health service use. A few studies examined other time frames, with single studies investigating mental health service use over the past 3 months, 5 years, and 7 years, and one included study considered mental health service use during the 24 months before and after a sibling’s death.
Twenty of the forty studies were classified as good quality (50.0%), seventeen as fair (42.5%), and three as poor quality (7.5%).
Overview of samples and factors investigated
The included studies examined a range of different factors associated with mental health service use. These included gender, age, marital status, ethnic groups, alcohol and drug abuse, education and income level, employment status, symptom severity, and residential location. The review identified service utilization factors related to socio-demographics, differences in utilization across countries, emerging socio-demographic factors and contexts, as well as structural and attitudinal barriers. These are described in further detail below.
Socio-demographic characteristics
Fifteen studies analyzed the association between gender and mental health service use, with fourteen studies reporting that mental health service use was more frequent among females with mental disorders than males [ 2 , 37 , 42 , 43 , 47 , 54 , 66 , 67 , 90 , 103 , 119 , 123 , 128 , 130 ]. A South Korean study concluded that gender was not associated with mental health service use [ 100 ], which might be due to the small sample size of 362 participants in the study.
Fourteen studies investigated age in association with mental health service use. Nine studies concluded that mental health service use was lower among young and old adult groups, with middle-aged persons with a mental disorder being most likely to access treatment from a mental health professional [ 26 , 42 , 43 , 47 , 54 , 66 , 67 , 123 , 130 ]. Forslund et al. [ 43 ] reported that mental health service use for women in Sweden peaked in the 45-to-64-year age group, while amongst males, mental health service use was stable across the lifespan. In contrast, two articles from New Zealand and Singapore each reported that young adults were the age group most likely to access services [ 28 , 119 ]. Reich et al. [ 103 ] concluded that age was unrelated to mental health service use when considered for the whole population, but sex-specific analyses reported that mental health service use was higher in older than younger females, while the opposite pattern was observed for males. A Canadian study using community health survey data also observed no significant age-related differences in mental health service use [ 104 ].
Marital status
There was mixed evidence concerning marital status. Studies from the United States and Germany concluded that participants who were married or cohabiting had lower rates of mental health service use [ 26 , 90 ], while Silvia et al. [ 120 ] found that mental health service use was higher among married participants in Portugal. Shafie et al. [ 119 ] reported being widowed was associated with lower rates of mental health service use in Singapore.
Ethnic groups
Eight studies examined the relationship between ethnic background and mental healthcare service use. Non-Hispanic White respondents were more likely to use mental health services in Canada and the United States [ 24 , 26 , 30 , 130 , 139 ], while Asians showed lower rates of mental health service use [ 28 , 139 ]. Chow & Mulder [ 28 ] investigated mental health service use among Asians, Europeans, Maori, and Pacific peoples in New Zealand. They concluded that Maori had the highest rate of mental health service use compared with other ethnic groups. De Luca et al. [ 30 ] reported that mental health service use was lower among ethnic minority non-veterans compared to veterans in the United States, especially for those with Black or Hispanic backgrounds. In contrast, a study conducted in the UK found that mental health service use did not vary by ethnicity, with no difference between white and non-white persons [ 54 ].
Alcohol and drug abuse
Two studies reported risky alcohol use was negatively associated with mental health service use [ 26 , 132 ]. However, within the time frame of the current review, there was insufficient published evidence on the impact of drug abuse on mental health service use among people with mental disorders. Choi, Diana & Nathan [ 26 ] found that drug abuse can lead to lower rates of mental health service use in the United States. In contrast, Werlen et al. [ 132 ] reported that risky use of (non-prescribed) prescription medications was associated with higher rates of mental health service use in Switzerland.
Education, income, and employment status
Four studies analyzed the relationship between education level, income, and mental health service use. Higher levels of educational attainment [ 26 , 120 ] and higher income [ 26 ] were generally reported to be associated with an increased likelihood of mental health service use. However, Reich et al. [ 103 ] observed that in Germany, high education and perceived middle or high social class were associated with reduced mental health service use. One paper reported no significant difference in mental health service use in South Korea, possibly due to the small number of people accessing mental healthcare services [ 100 ].
Three studies reported that compared to those who are unemployed, those in work were less likely to use mental health services [ 26 , 90 , 119 ]. This outcome aligned with a Canadian study consisting of immigrants and general populations, Islam et al. [ 66 ] concluded that immigrants who were currently unemployed had higher odds of seeking treatment than those who were employed. However, an Italian [ 123 ] and a South Korean study [ 100 ] found that employment status was not related to mental health service use.
Symptom severity
Ten studies investigated the association between symptom severity and mental health service use and ten papers concluded that participants with moderate or serious psychological symptoms were more likely to use mental health services compared to those with mild symptoms [ 23 , 27 , 66 , 103 , 120 , 123 , 130 , 139 ]. Other studies showed that study participants who viewed their mental health as poor [ 42 ], who were diagnosed with more than one mental disorder [ 103 ], and those who recognized their own need for mental health treatment [ 54 , 139 ] were more likely to receive mental health services.
Residential location
Three studies investigated the association between residential location and mental health service use. Volkert et al. [ 128 ] concluded that the rates of mental health service use in Germany were significantly lower among those living in Canterbury than those living in Hamburg. A Canadian study found individuals living in neighborhoods where renters outnumber homeowners were less likely to access mental health services [ 42 ]. In the United States, for participants with low or moderate mental illness, mental health service use was lower for those residing closer to clinics [ 46 ].
Immigrants & refugees
The reviewed research found that non-refugee immigrants had slightly higher rates of mental health service use than refugees [ 10 ]. Other research found that long-term residents were more likely to access services than immigrants regardless of their origin [ 31 , 134 ]. For example, Italian citizens were found to have higher rates of mental health service use compared to immigrants, especially for affective disorders [ 123 ]. In Canada, immigrants from West and Central Africa were more likely to access mental health services compared to immigrants from East Asia and the Pacific [ 31 ]. Research from Chile found that the rates of mental health service use were similar for immigrants and non-immigrants [ 40 ]. Although, a positive association between the severity of symptoms and rates of mental health service use was only observed among immigrants [ 40 ]. Whitley et al. [ 134 ] found that immigrants born in Asia or Africa had lower rates of mental health service use, but higher rates of service satisfaction scores compared to immigrants from other countries.
Emerging areas
Our literature review identified several areas in which only a small number of studies were found. We briefly describe them here as these may reflect emerging areas of research interest. Few published articles examined mental health treatment among participants with mental disorders together with chronic physical health conditions, and we only included the papers in this systematic review if they contained a healthy comparison group. We identified two papers that focused on survivors of adolescent and young adult cancer [ 68 ] and participants with physical health problems [ 110 ]. Both studies reported that participants with other chronic conditions reported higher rates of mental health service use than the general population [ 68 , 110 ].
Two studies compared treatment seeking among people experiencing stressful life events. Erlangsen et al. [ 39 ] investigated the impact of spousal suicide, and Gazibara et al. [ 45 ] examined the effect of a sibling’s death on mental health service use. People bereaved by relatives’ deaths were more likely to use mental health services than the general population [ 39 , 45 ]. The peak effect was observed in the first 3 months after the death for both genders, while evidence of an increase in mental health service use was evident up to 24 months before a sibling’s death and remained evident for at least 24 months after the death [ 45 ].
One paper studied the impact of the COVID-19 pandemic lockdown on mental health service use. An Israeli study concluded that compared to 2018 and 2019, adults reported they were reluctant to receive treatment during the pandemic lockdown and observed a decrease in mental health service use [ 13 ].
Structural and attitudinal barriers
In addition to the research considering a range of population characteristics (e.g. male, younger, or older age), several papers examined how attitudinal and structural factors were associated with mental health service use. The most frequently reported of these factors were cost [ 23 , 46 , 68 , 120 ], lack of transportation [ 46 , 83 ], inadequate services/ lack of availability [ 23 , 46 , 83 , 128 ], poor understanding of mental disorders and what services were available [ 10 , 11 , 22 , 83 , 100 , 105 , 120 ], language difficulties [ 10 ], and stigma-related barriers [ 83 , 100 , 103 , 105 , 128 ]. Cultural issues and personal beliefs may influence the understanding of mental disorders and prevent people from using mental health services due to mistrust or fear of treatment [ 100 , 128 ]. The review also observed some unique barriers to different population groups. Choi, Diana & Nathan [ 26 ] mentioned that lack of readiness and treatment cost were the biggest difficulties for older adults, while young participants were more concerned about stigma. Females also reported childcare as a factor limiting their ability to use mental health services, while the evidence reviewed argued that males prefer to solve mental health issues on their own, with internal control beliefs and lack of social support likely reducing their use of mental health services [ 37 , 103 ].
Summary of evidence
This systematic review investigated mental health service use among people with mental disorders and identified the factors associated with service use in high-income countries.
Most studies found that females with mental health conditions were more likely to use mental health services than males. The relationship between age and mental health service use was bell-shaped, with middle-aged participants having higher rates of mental health service use than other age groups. Possible explanations included that the elderly might be reluctant to disclose mental health symptoms, they might attribute their mental health symptoms to increasing age [ 20 ], and they may prefer to self-manage instead of seeking help from health professionals [ 44 ]. Caucasian ethnicity and higher household income were also associated with higher rates of mental health service use. Greater use of mental health services was observed in participants with severe mental symptoms, including among veterans [ 19 , 37 , 92 ]. Two studies also concluded that compared to other cultural groups, Asian respondents were more likely to receive treatment when problems were severe or had disabling effects [ 86 , 97 ]. There was mixed evidence regarding employment status, although some studies found employment to be negatively related to receiving treatment [ 26 , 90 ], and unemployed people are more likely to seek help [ 119 ]. There was inconsistent evidence for the association between marital status and service utilization. This contradictory evidence on marital status might be attributed to a lack of specification, some papers categorize it as married and non-married [ 26 , 71 , 131 ], while others further differentiate between those who were widowed, separated, and divorced [ 90 , 119 ].
A number of studies showed that immigrants can face unique stressors owing to their experience of migration, which may exacerbate or be the source of their mental health issues, and impact the use of mental health services [ 1 , 8 ]. These include separation from families, support networks, linguistic and cultural barriers [ 9 , 113 ].
Due to the increased number of international migrants, immigrants’ mental health status and healthcare use has drawn growing attention [ 7 , 77 , 99 ]. Kirmayer et al. [ 70 ] and Helman [ 57 ] found that culture might be associated with people’s attitudes and understanding of mental health, influencing help-seeking behaviors. In general, the current results showed that immigrants and refugees were less likely to use mental health services than their native-born counterparts, and this finding was consistent with previous studies [ 75 , 82 , 127 ]. For immigrants, the length of stay in the host country was closely related to rates of mental health service use, which was argued to reflect increasing familiarity with the host culture and language proficiency [ 1 , 59 ].
Both mental disorders and chronic diseases contribute significantly to the global burden of disease. Prior studies have shown that people with chronic disease have a higher chance of experiencing psychological distress [ 6 , 14 , 68 , 73 ], and vice versa [ 49 , 74 ]. Hendrie et al. [ 58 ] concluded that respondents with chronic diseases were more likely to attend mental healthcare and reported higher costs. Negative experiences and stressful consequences related to chronic disease might contribute to the increased potential for mental illness but more opportunities to seek help from health professionals [ 60 , 108 , 135 ]. People with chronic diseases and mental health problems might experience more long-term pain and limitations in their daily lives, and these stressors can exacerbate their health conditions, and impact their attitude toward seeking help.
The COVID-19 pandemic had a major impact on mental health service use worldwide, the hospital admission and consultation rate decreased dramatically during the first pandemic year [ 118 ]. This reduction in service access might be a side effect of social distancing measures taken as mitigation measures, reducing both inciting incidents and physical access to services.
Financial difficulty, service availability, and stigma were frequently identified in the literature as structural and attitudinal factors associated with lower rates of mental health service use. These factors were associated with the different rates of mental health service use for different ethnicities. For example, Asian people were less likely than other groups to identify cost as a factor limiting their use of mental health services, with a major barrier for Asian people being stigma and cultural factors [ 139 ].
Limitations
This systematic review employed a broad search strategy with broad search terms to capture relevant articles. Rather than emphasizing a particular mental disorder, this review focused on the rates of mental health service use among adults aged 18 years or older who were experiencing a common mental disorder. However, this review still contained limitations. First was the potential for selection bias. Although we used various search terms for mental health service use and mental disorder, it is possible that the service use was not the primary research question for some papers, or that the relevant service use outcome was not statistically significant- in these cases, if the information was not reported in the abstract, relevant papers might have been missed. It is also important to note that this systematic review includes studies conducted in different countries and that the mental health systems and opportunities for access vary among countries. We only searched for full-text peer-reviewed articles published in English. Grey literature and papers published in other languages were excluded from the search. Most of the included literature used self-reported data to measure service access, and these data can be liable to recall bias. Studies using administrative data were also included in the systematic review, and we note that although they have large datasets, compared to survey data, there is often a lack of adequate control variables included to minimize possible confounding influences.
Future research
There is a need for more published articles on several aspects that may influence the service utilization among people with mental disorders, including the impact of residential or neighborhood areas, and household income across various income groups. These aspects are important population characteristics that require further research to inform the targeting and type of support (e.g. low-cost, accessible). Additionally, there was a lack of longitudinal research on mental health service use, future studies could use the data to identify changes over time and relate events to specific exposures (e.g. Covid-19 pandemic). Future studies can investigate the cost of mental health treatment in detailed aspects, (e.g. publicly funded mental health services, community-based support for free or low-cost mental health services). Overall, there was a lack of studies for ethnic minorities, given ethnic minority groups were more vulnerable to mental disorders but with less mental health service use. Future research can expand gender identity representation in data collection and move beyond the binary genders. People with non-binary gender identities can face greater challenges and disadvantages in mental health and mental health service use.
This review identified that middle-aged, female gender, Caucasian ethnicity, and severity of mental disorder symptoms were factors consistently associated with higher rates of mental health service use among people with a mental disorder. In comparison, the influence of employment and marital status on mental health service use was unclear due to the limited number of published studies and/ or mixed results. Financial difficulty, stigma, lack of transportation, and inadequate mental health services were the structural barriers most consistently identified as being associated with lower rates of mental health service use. Finally, ethnicity and immigrant status were also associated with differences in understanding of mental health (i.e. mental health literacy), effectiveness of mental health treatments, as well as language difficulties. The insights gained through this review on the factors associated with mental health service use can help clinicians and policymakers to identify and provide more targeted support for those least likely to access services, and this in turn may contribute to reducing inequalities in not only mental health service use but also the burden of mental disorders.
Availability of data and materials
All data and materials related to the study are available on request from the first author, [email protected].
Abe-Kim J, Takeuchi DT, Hong S, Zane N, Sue S, Spencer MS, et al. Use of mental health–related services among immigrant and US-born Asian americans: results from the national latino and Asian American study. Am J Public Health. 2007;97(1):91–8.
Article PubMed PubMed Central Google Scholar
Abramovich A, De Oliveira C, Kiran T, Iwajomo T, Ross LE, Kurdyak P. Assessment of health conditions and health service use among transgender patients in Canada. JAMA Netw Open. 2020;3(8):e2015036. https://doi.org/10.1001/jamanetworkopen.2020.15036 .
Ambikile JS, Iseselo MK. Mental health care and delivery system at Temeke hospital in Dar Es Salaam, Tanzania. BMC Psychiatry. 2017;17:1–13. https://doi.org/10.1186/s12888-017-1271-9 .
Article Google Scholar
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013.
Book Google Scholar
Australian Bureau of Statistics. 2017-18, Mental health, ABS, viewed 23 July 2023. https://www.abs.gov.au/statistics/health/mental-health/mental-health/2017-18 .
Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes. Diabetes Care. 2001;24(6):1069–78.
Article CAS PubMed Google Scholar
Bacon L, Bourne R, Oakley C, Humphreys M. Immigration policy: implications for mental health services. Adv Psychiatr Treat. 2010;16:124–32.
Bhatia S, Ram A. Theorizing identity in transnational and diaspora cultures: a critical approach to acculturation. Int J Intercultural Relations. 2009;33:140–9.
Bhugra D. Migration, distress and cultural identity. Br Med Bull. 2004;69:129–41.
Article PubMed Google Scholar
Björkenstam E, Helgesson M, Norredam M, Sijbrandij M, de Montgomery CJ, Mittendorfer-Rutz E. Differences in psychiatric care utilization between refugees, non-refugee migrants and Swedish-born youth. Psychol Med. 2022;52(7):1365–75. https://doi.org/10.1017/s0033291720003190 .
Australian Bureau of Statistics. (2020–2022). National study of mental health and wellbeing. ABS. https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/latest-release .
Blais RK, Tsai J, Southwick SM, Pietrzak RH. Barriers and facilitators related to mental health care use among older veterans in the United States. Psychiatr Serv. 2015;66(5):500–6. https://doi.org/10.1176/appi.ps.201300469 .
Blasbalg U, Sinai D, Arnon S, Hermon Y, Toren P. Mental health consequences of the COVID-19 pandemic: results from a large-scale population-based study in Israel. Compr Psychiatr. 2023;123:123. https://doi.org/10.1016/j.comppsych.2023.152383 .
Bodurka-Bevers D, Basen-Engquist K, Carmack CL, Fitzgerald MA, Wolf JK, Moor Cd, Gershenson DM. Depression, anxiety, and quality of life in patients with epthelial ovarian cancer. Gynecol Oncol. 2000;78:302–8.
Bondesson E, Alpar T, Petersson IF, Schelin MEC, Jöud A. Health care utilization among individuals who die by suicide as compared to the general population: a population-based register study in Sweden. BMC Public Health. 2022;22(1):1616. https://doi.org/10.1186/s12889-022-14006-x
Borges G, Aguilar-Gaxiola S, Andrade L, Benjet C, Cia A, Kessler RC, Orozco R, Sampson N, Stagnaro JC, Torres Y, Viana MC, Medina-Mora ME. Twelve-month mental health service use in six countries of the Americas: a regional report from the World Mental Health Surveys. Epidemiol Psychiatr Sci. 2019;29:e53. https://doi.org/10.1017/s2045796019000477 .
Article CAS PubMed PubMed Central Google Scholar
Brenman NF, Luitel NP, Mall S, Jordans MJD. Demand and access to mental health services: a qualitative formative study in Nepal. BMC Int Health Hum Rights. 2014;14(1):1–12. https://doi.org/10.1186/1472-698X-14-22 . PMID: 25084826.
Budhathoki SS, Pokharel PK, Good S, Limbu S, Bhattachan M, Osborne RH. The potential of health literacy to address the health related UN sustainable development goal 3 (SDG3) in Nepal: a rapid review. BMC Health Serv Res. 2017;17(1):1–13. https://doi.org/10.1186/s12913-016-1943-z . PMID: 28049468.
Brown JS, Evans-Lacko S, Aschan L, Henderson MJ, Hatch SL, Hotopf M. Seeking informal and formal help for mental health problems in the community: a secondary analysis from a psychiatric morbidity survey in South London. BMC Psychiatry. 2014;14(1):275.
Burroughs H, Lovell K, Morley M, Baldwin R, Burns A, Chew-Graham C. Justifiable depression’: how primary care professionals and patients view late-life depression? A qualitative study. Fam Pract. 2006;23(3):369–77. https://doi.org/10.1093/fampra/cmi115 .
Caron J, Fleury MJ, Perreault M, Crocker A, Tremblay J, Tousignant M, Kestens Y, Cargo M, Daniel M. Prevalence of psychological distress and mental disorders, and use of mental health services in the epidemiological catchment area of Montreal South-West. BMC Psychiatry. 2012;12:12. https://doi.org/10.1186/1471-244X-12-183 .
Chan CMH, Ng SL, In S, Wee LH, Siau CS. Predictors of psychological distress and mental health resource utilization among employees in Malaysia. Int J Environ Res Public Health. 2021;18(1):1–15. https://doi.org/10.3390/ijerph18010314 .
Chaudhry MM, Banta JE, McCleary K, Mataya R, Banta JM. Psychological distress, structural barriers, and health services utilization among U.S. adults: National Health interview survey, 2011–2017. Int J Mental Health. 2022. https://doi.org/10.1080/00207411.2022.2123694
Chiu M, Amartey A, Wang X, Kurdyak P, Luppa M, Giersdorf J, Riedel-Heller S, Prütz F, Rommel A. Ethnic differences in mental health status and service utilization: a population-based study in Ontario, Canada frequent attenders in the German healthcare system: determinants of high utilization of primary care services. Results from the cross-sectional. Can J PsychiatryBMC Fam Pract. 2018;6321(71):481–91. https://doi.org/10.1186/s12875-020-1082-9 .
Cho SJ, Lee JY, Hong JP, Lee HB, Cho MJ, Hahm BJ. Mental health service use in a nationwide sample of Korean adults. Soc Psychiatry Psychiatr Epidemiol. 2009;44:943–51.
Choi NG, DiNitto DM, Marti CN. Treatment use, perceived need, and barriers to seeking treatment for substance abuse and mental health problems among older adults compared to younger adults. Drug Alcohol Depend. 2014;145:113–20. https://doi.org/10.1016/j.drugalcdep.2014.10.004 .
Chong SA, Abdin E, Vaingankar JA, Kwok KW, Subramaniam M. Where do people with mental disorders in Singapore go to for help? Ann Acad Med Singap. 2012;41(4):154–60.
Chow CS, Mulder RT. Mental health service use by asians: a New Zealand census. N Z Med J. 2017;130(1461):35–41.
PubMed Google Scholar
Dang HM, Lam TT, Dao A, Weiss B. Mental health literacy at the public health level in low and middle income countries: an exploratory mixed methods study in Vietnam. PLoS ONE. 2020;15(12):e0244573. https://doi.org/10.1371/journal.pone.0244573
De Luca SM, Blosnich JR, Hentschel EA, King E, Amen S. Mental health care utilization: how race, ethnicity and veteran status are associated with seeking help. Community Ment Health J. 2016;52(2):174–9. https://doi.org/10.1007/s10597-015-9964-3 .
Durbin A, Moineddin R, Lin E, Steele LS, Glazier RH. Mental health service use by recent immigrants from different world regions and by non-immigrants in Ontario, Canada: a cross-sectional study. BMC Health Serv Res. 2015;15(1):336. https://doi.org/10.1186/s12913-015-0995-9
Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. JAMA. 2004;291(21):2581–90.
Derr AS. Mental health service use among immigrants in the United States: a systematic review. Psychiatr Serv. 2016;67:265–74. https://doi.org/10.1176/appi.ps.201500004 .
Dimoff JK, Kelloway EK. With a little help from my Boss: the impact of workplace mental health training on leader behaviors and employee resource utilization. J Occup Health Psychol. 2019;24:4–19.
Duong MT, Bruns EJ, Lee K, et al. Rates of mental health service utilization by children and adolescents in schools and other common service settings: a systematic review and meta-analysis. Adm Policy Ment Health. 2021;48:420–39. https://doi.org/10.1007/s10488-020-01080-9 .
Edman JL, Kameoka VA. Cultural differences in illness schemas: an analysis of Filipino and American illness attributions. J Cross Cult Psychol. 1997;28(3):252–65.
Elbogen EB, Wagner HR, Johnson SC, Kinneer P, Kang H, Vasterling JJ, Timko C, Beckham JC. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey. Psychiatr Serv. 2013;64(2):134–41. https://doi.org/10.1176/appi.ps.004792011 .
Enticott J, Dawadi S, Shawyer F, Inder B, Fossey E, Teede H, Rosenberg S, Ozols Am I, Meadows G. Mental Health in Australia: psychological distress reported in six consecutive cross-sectional national surveys from 2001 to 2018. Front Psychiatry. 2022;13:815904. https://doi.org/10.3389/fpsyt.2022.815904
Erlangsen A, Runeson B, Bolton JM, Wilcox HC, Forman JL, Krogh J, Katherine Shear M, Nordentoft M, Conwell Y. Association between spousal suicide and mental, physical, and social health outcomes a longitudinal and nationwide register-based study. JAMA Psychiatry. 2017;74(5):456–64. https://doi.org/10.1001/jamapsychiatry.2017.0226 .
Errazuriz A, Schmidt K, Valenzuela P, Pino R, Jones PB. Common mental disorders in Peruvian immigrant in Chile: a comparison with the host population. BMC Public Health. 2023;23(1):1274. https://doi.org/10.1186/s12889-023-15793-7
Evans-Lacko S, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Benjet C, Bruffaerts R, Chiu WT, Florescu S, de Girolamo G, Gureje O, Haro JM, He Y, Hu C, Karam EG, Kawakami N, Lee S, Lund C, Kovess-Masfety V, Levinson D, Thornicroft G. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: results from the WHO World Mental Health (WMH) surveys. Psychol Med. 2018;48(9):1560–71. https://doi.org/10.1017/s0033291717003336 .
Fleury MJ, Grenier G, Bamvita JM, Perreault M, Kestens Y, Caron J. Comprehensive determinants of health service utilisation for mental health reasons in a Canadian catchment area. Int J Equity Health. 2012;11(1):20. https://doi.org/10.1186/1475-9276-11-20
Forslund T, Kosidou K, Wicks S, Dalman C. Trends in psychiatric diagnoses, medications and psychological therapies in a large Swedish region: a population-based study. BMC Psychiatry. 2020;20(1):328. https://doi.org/10.1186/s12888-020-02749-z
Garrido MM, Kane RL, Kaas M, Kane RA. Use of mental health care by community-dwelling older adults. J Am Geriatr Soc. 2011;59(1):50–6. https://doi.org/10.1111/j.1532-5415.2010.03220.x .
Gazibara T, Ornstein KA, Gillezeau C, Aldridge M, Groenvold M, Nordentoft M, Thygesen LC. Bereavement among adult siblings: an examination of health services utilization and mental health outcomes. Am J Epidemiol. 2021;190(12):2571–81. https://doi.org/10.1093/aje/kwab212 .
Glasheen C, Forman-Hoffman VL, Hedden S, Ridenour TA, Wang J, Porter JD. Residential transience among adults: prevalence, characteristics, and association with mental illness and mental health service use. Community Ment Health J. 2019;55(5):784–97. https://doi.org/10.1007/s10597-019-00385-w .
Gonçalves DC, Coelho CM, Byrne GJ. The use of healthcare services for mental health problems by middle-aged and older adults. Arch Gerontol Geriatr. 2014;59(2):393–7. https://doi.org/10.1016/j.archger.2014.04.013 .
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry. 2022;9:137–50. https://doi.org/10.1016/S2215-0366(21)00395-3 .
Article PubMed Central Google Scholar
Goff DC, Sullivan LM, McEvoy JP, et al. A comparison of ten-year cardiac risk estimates in schizophrenia patients from the CATIE Study and matched controls. Schizophr Res. 2005;80(1):45–53. https://doi.org/10.1016/j.schres.2005.08.010 .
Goncalves Daniela C. From loving grandma to working with older adults: promoting positive attitudes towards aging. Educ Gerontol. 2009;35(3):202–25.
Gong F, Gage S-JL, Tacata LA Jr. Helpseeking behavior among Filipino americans: a cultural analysis of face and language. J Community Psychol. 2003;31:469–88. https://doi.org/10.1002/jcop.10063 .
Grossbard JR, Lehavot K, Hoerster KD, Jakupcak M, Seal KH, Simpson TL. Relationships among veteran status, gender, and key health indicators in a national young adult sample. Psychiatric Serv. 2013;64(6):547–53. https://doi.org/10.1176/appi.ps.003002012 .
Hajebi A, Motevalian SA, Rahimi-Movaghar A, Sharifi V, Amin-Esmaeili M, Radgoodarzi R, Hefazi M. Major anxiety disorders in Iran: prevalence, sociodemographic correlates and service utilization. BMC Psychiatry. 2018;18(1):261. https://doi.org/10.1186/s12888-018-1828-2
Harber-Aschan L, Hotopf M, Brown JSL, Henderson M, Hatch SL. Longitudinal patterns of mental health service utilisation by those with mental-physical comorbidity in the community. J Psychosom Res. 2019;117:10–9. https://doi.org/10.1016/j.jpsychores.2018.11.005 .
Huýnh C, Caron J, Fleury MJ. Mental health services use among adults with or without mental disorders: do development stages matter? Int J Soc Psychiatry. 2016;62(5):434–51. https://doi.org/10.1177/0020764016641906 .
Helliwell JF, Layard R, Sachs JD, De Neve JE, Aknin LB, Wang S, editors. World Happiness Report 2022. New York: Sustainable Development Solutions Network; 2022.
Google Scholar
Helman C. Culture, health and illness. 5th ed. CRC Press; 2007. https://doi.org/10.1201/b13281 .
Hendrie HC, Lindgren D, Hay DP, et al. Comorbidity profile and healthcare utilization in elderly patients with serious mental illnesses. Am J Geriatr Psychiatry. 2013;21(12):1267–76. https://doi.org/10.1016/j.jagp.2013.01.056 .
Hermannsdóttir BS, Aegisdottir S. Spirituality, connectedness, and beliefs about psychological services among Filipino immigrants in Iceland. Counsel Psychol. 2016;44(4):546–72.
Hoffman KE, McCarthy EP, Recklitis CJ, Ng AK. Psychological distress in long-term survivors of adult-onset cancer: results from a national survey. Arch Intern Med. 2009;169:1274–81.
Hoge C, Castro C, Messer S, McGurk D, Cotting D, Koffman R. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351:13–22.
Hoge C, Grossman S, Auchterlonie J, Riviere L, Milliken C, Wilk J. PTSD treatment for soldiers after combat deployment: low utilization of mental health care and reasons for dropout. Psychiatric Serv. 2014;65(8):997–1004. https://doi.org/10.1176/appi.ps.201300307 .
Hom MA, Stanley IH, Schneider ME, Joiner TE. A systematic review of help-seeking and mental health service utilization among military service members. Clin Psychol Rev. 2017;53:59–78. https://doi.org/10.1016/j.cpr.2017.01.008 .
Hwang W, Miranda J, Chung C. Psychosis and shamanism in a Filipino–American immigrant. Cult Med Psychiatry. 2007;31(2):251–69.
Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, Smedley BD, Stith AY, Nelson AR. (Eds.). Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington National Academies Press (US). 2023. https://doi.org/10.17226/12875 .
Islam F, Khanlou N, Macpherson A, Tamim H. Mental health consultation among Ontario’s immigrant populations. Community Ment Health J. 2018;54(5):579–89. https://doi.org/10.1007/s10597-017-0210-z .
Jacobi F, Groß J. Prevalence of mental disorders, health-related quality of life, and service utilization across the adult life span. Psychiatrie. 2014;11(4):227–33. https://doi.org/10.1055/s-0038-1670774 .
Kaul S, Avila JC, Mutambudzi M, Russell H, Kirchhoff AC, Schwartz CL. Mental distress and health care use among survivors of adolescent and young adult cancer: a cross-sectional analysis of the National Health Interview Survey. Cancer. 2017;123(5):869–78. https://doi.org/10.1002/cncr.30417 .
Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–9.
Kirmayer LJ, Weinfeld M, Burgos G, et al. Use of health care services for psychological distress by immigrants in an urban multicultural milieu. Can J Psychiatry. 2007;52:295–304.
Kose T. Gender, income and mental health: the Turkish case. PLoS ONE. 2020;15(4):e0232344. https://doi.org/10.1371/journal.pone.0232344
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. https://doi.org/10.1046/j.1525-1497.2001.016009606.x .
Kugaya A, Akechi T, Okuyama T, Nakano T, Mikami I, Okamura H, Uchitomi Y. Prevalence, predictive factors, and screening for psychological distress in patients with newly diagnosed head and neck cancer. Cancer. 2000;88:2817–23.
Kurdyak PA, Gnam WH, Goering P, Chong A, Alter DA. The relationship between depressive symptoms, health service consumption, and prognosis after acute myocardial infarction: a prospective cohort study. BMC Health Serv Res. 2008;8: 200. https://doi.org/10.1186/1472-6963-8-200 .
Le Meyer O, Zane N, Cho YI, Takeuchi DT. Use of specialty mental health services by Asian americans with psychiatric disorders. J Consult Clin Psychol. 2009;77(5):1000–5. https://doi.org/10.1037/a0017065 .
Li W, Dorstyn DS, Denson LA. Predictors of mental health service use by young adults: a systematic review. Psychiatric Serv. 2016;67(9):946–56. https://doi.org/10.1176/appi.ps.201500280 .
Lindert J, Schouler-Ocak M, Heinz A, Priebe S. Mental health, health care utilisation of migrants in Europe. Eur Psychiatry. 2008;23 Suppl 1:14–20.
CAS PubMed Google Scholar
Lovering S. Cultural attitudes and beliefs about pain. J Transcult Nurs. 2006;17(4):389–95.
Luitel NP, Jordans MJD, Kohrt BA, Rathod SD, Komproe IH. Treatment gap and barriers for mental health care: A cross-sectional community survey in Nepal. PLoS One. 2017;12(8):1–15. https://doi.org/10.1371/journal.pone.0183223 . PMID: 28817734.
Article CAS Google Scholar
Jansson I, Gunnarsson AB. Employers’ views of the impact of Mental Health problems on the ability to work. Work. 2018;59:585–98.
Kayiteshonga Y, Sezibera V, Mugabo L, Iyamuremye JD. Prevalence of mental disorders, associated co-morbidities, health care knowledge and service utilization in Rwanda - towards a blueprint for promoting mental health care services in low- and middle-income countries? BMC Public Health. 2022;22(1):1858. https://doi.org/10.1186/s12889-022-14165-x .
Kirmayer LJ, Narasiah L, Munoz M, Rashid M, Ryder AG, Guzder J, Hassan G, Rousseau C, Pottie K, Canadian Collaboration for Immigrant and Refugee Health (CCIRH). Common mental health problems in immigrants and refugees: general approach in primary care. Can Med Assoc J. 2011;183(12):E959-67. https://doi.org/10.1503/cmaj.090292 .
Kline AC, Panza KE, Nichter B, Tsai J, Harpaz-Rotem I, Norman SB, Pietrzak RH. Mental health care use among U.S. Military veterans: results from the 2019–2020 national health and resilience in veterans study. Psychiatr Serv. 2022;73(6):628–35. https://doi.org/10.1176/appi.ps.202100112 .
Knipscheer JW, Kleber RJ. Help-seeking behavior of west African migrants. J Community Psychol. 2008;36:915–28. https://doi.org/10.1002/jcop.20264 .
Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82(11):858–66.
PubMed PubMed Central Google Scholar
Kung WW. Cultural and practical barriers to seeking mental health treatment for Chinese americans. J Community Psychol. 2004;32(1):27–43.
Lipson SK, Lattie EG, Eisenberg D. Increased rates of mental health service utilization by U.S. College students: 10-year population-level trends (2007–2017). Psychiatr Serv. 2019;70(1):60–3. https://doi.org/10.1176/appi.ps.201800332 .
Liu L, Chen XL, Ni CP, Yang P, Huang YQ, Liu ZR, Wang B, Yan YP. Survey on the use of mental health services and help-seeking behaviors in a community population in Northwestern China. Psychiatry Res. 2018;262:135–40. https://doi.org/10.1016/j.psychres.2018.02.010 .
Lu J, Xu X, Huang Y, Li T, Ma C, Xu G, Yin H, Ma Y, Wang L, Huang Z, Yan Y, Wang B, Xiao S, Zhou L, Li L, Zhang Y, Chen H, Zhang T, Yan J, Zhang N. Prevalence of depressive disorders and treatment in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2021;8(11):981–90. https://doi.org/10.1016/S2215-0366(21)00251-0 .
Mack S, Jacobi F, Gerschler A, Strehle J, Höfler M, Busch MA, Maske UE, Hapke U, Seiffert I, Gaebel W, Zielasek J, Maier W, Wittchen HU. Self-reported utilization of mental health services in the adult German population–evidence for unmet needs? Results of the DEGS1-Mental Health Module (DEGS1-MH). Int J Methods Psychiatr Res. 2014;23(3):289–303. https://doi.org/10.1002/mpr.1438 .
Mahar AL, Aiken AB, Cramm H, Whitehead M, Groome P, Kurdyak P. Mental health services use trends in Canadian veterans: a Population-based Retrospective Cohort Study in Ontario. Can J Psychiatry. 2018;63(6):378–86. https://doi.org/10.1177/0706743717730826 .
Maneze D, DiGiacomo M, Salamonson Y, Descallar J, Davidson PM. Facilitators and barriers to health-seeking behaviours among Filipino migrants: inductive analysis to inform health promotion. BioMed Res Int. 2015;2015:506269.
Martinez AB, Co M, Lau J, et al. Filipino help-seeking for mental health problems and associated barriers and facilitators: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2020;55:1397–413. https://doi.org/10.1007/s00127-020-01937-2 .
McKibben JBA, Fullerton CS, Gray CL, Kessler RC, Stein MB, Ursano RJ. Mental health service utilization in the U.S. Army Psychiatr Serv. 2013;64(4):347–53. https://doi.org/10.1176/appi.ps.000602012 .
Mosier KE, Vasiliadis H-M, Lepnurm M, Puchala C, Pekrul C, Tempier R. Prevalence of mental disorders and service utilization in seniors: results from the Canadian community health survey cycle 1.2. Int J Geriatr Psychiatry. 2010;25(10):960–7. https://doi.org/10.1002/gps.2434 .
National Mental Health Commission. Economics of Mental Health in Australia. 2016. Available at: https://www.mentalhealthcommission.gov.au/news-and-media/media-releases/2016/december/economics-of-mental-health-in-australia . Accessed: 20 July 2023.
Nicdao EG, Duldulao AA, Takeuchi DT. Psychological Distress, Nativity, and Help-Seeking among Filipino Americans. Education, Social Factors, and Health Beliefs in Health and Health Care Services. Emerald Group Publishing Ltd. 2015:107–20. https://doi.org/10.1108/S0275-495920150000033005 .
Nock MK, Stein MB, Heeringa SG, Ursano RJ, Colpe LJ, Fullerton CS, et al. Prevalence and correlates of suicidal behavior among soldiers: results from the Army study to assess risk and resilience in service members (Army STARRS). JAMA Psychiatry. 2014;71(5):514–22. https://doi.org/10.1001/jamapsychiatry.2014 .
Ortega AN, Fang H, Perez VH, Rizzo JA, Carter-Pokras O, Wallace SP, et al. Health care access, use of services, and experiences among undocumented mexicans and other latinos. Arch Intern Med. 2007;167(21):2354–60.
Park S, Cho MJ, Bae JN, Chang SM, Jeon HJ, Hahm BJ, Son JW, Kim SG, Bae A, Hong JP. Comparison of treated and untreated major depressive disorder in a nationwide sample of Korean adults. Community Ment Health J. 2012;48(3):363–71. https://doi.org/10.1007/s10597-011-9434-5 .
Patel V, Saxena S, Lund C, et al. The lancet commission on global mental health and sustainable development. Lancet. 2018;392:1553–98.
Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369(9569):1302–13. https://doi.org/10.1016/S0140-6736(07)60368-7 .
Reich H, Niermann HCM, Voss C, Venz J, Pieper L, Beesdo-Baum K. Sociodemographic, psychological, and clinical characteristics associated with health service (non-)use for mental disorders in adolescents and young adults from the general population. Eur Child Adolesc Psychiatry. 2023. https://doi.org/10.1007/s00787-023-02146-3 .
Pelletier L, O’Donnell S, McRae L, Grenier J. The burden of generalized anxiety disorder in Canada. Health Promot Chronic Dis Prev Can. 2017;37(2):54–62. https://doi.org/10.24095/hpcdp.37.2.04 .
Rim SJ, Hahm BJ, Seong SJ, Park JE, Chang SM, Kim BS, An H, Jeon HJ, Hong JP, Park S. Prevalence of Mental disorders and Associated factors in Korean adults: national mental health survey of Korea 2021. Psychiatry Invest. 2023;20(3):262–72. https://doi.org/10.30773/pi.2022.0307 .
Pols H, Oak S. War & military mental health: the US psychiatric response in the 20th century. Am J Public Health. 2007;97:2132–42.
Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A. No health without mental health. Lancet. 2007;370(9590):859–77. https://doi.org/10.1016/S0140-6736(07)61238-0 .
Ramsey S, Blough D, Kirchhoff A, et al. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff. 2013;32:1143–52.
Raphael MJ, Gupta S, Wei X, Peng Y, Soares CN, Bedard PL, Siemens DR, Robinson AG, Booth CM. Long-term mental health service utilization among survivors of testicular cancer: a population-based cohort study. J Clin Oncol. 2021;39(7):779–86. https://doi.org/10.1200/jco.20.02298 .
Reaume SV, Luther AWM, Ferro MA. Physical morbidity and mental health care among young people. J Adolesc Health. 2021;68(3):540–7. https://doi.org/10.1016/j.jadohealth.2020.06.040 .
Reavley NJ, Morgan AJ, Petrie D, Jorm AF. Does mental health-related discrimination predict health service use 2 years later? Findings from an Australian national survey. Soc Psychiatry Psychiatr Epidemiol. 2020;55(2):197–204. https://doi.org/10.1007/s00127-019-01762-2 .
Roberts T, Miguel Esponda G, Krupchanka D, Shidhaye R, Patel V, Rathod S. Factors associated with health service utilisation for common mental disorders: a systematic review. BMC Psychiatry. 2018;18(1):262. https://doi.org/10.1186/s12888-018-1837-1 .
Rogler LH. International migrations. A framework for directing research. Am Psychol. 1994;49(8):701–8.
Sagar R, Pattanayak RD, Chandrasekaran R, Chaudhury PK, Deswal BS, Singh RL, et al. Twelve-month prevalence and treatment gap for common mental disorders: findings from a large-scale epidemiological survey in India. Indian J Psychiatry. 2017;59(1):46.
Saxena S, Sharan P, Saraceno B. Budget and financing of mental health services: baseline information on 89 countries from WHO’s project atlas. J Ment Health Policy Econ. 2003;6(3):135–43.
Sawyer MG, Whaites L, Rey JM, Hazell PL, Graetz BW, Baghurst P. Health-related quality of life of children and adolescents with mental disorders. J Am Acad Child Adolesc Psychiatry. 2002;41(5):530–7. https://doi.org/10.1097/00004583-200205000-00010 .
Seal KH, Metzler TJ, Gima KS, Bertenthal D, Gaguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using department of veterans affairs health care, 2002–2008. Am J Public Health. 2009;99(9):1651–8.
Sepúlveda-Loyola W, Rodríguez-S´anchez I, P´erez-Rodríguez P, Ganz F, Torralba R, Oliveira DV, et al. Impact of social isolation due to COVID-19 on health in older people: mental and physical effects and recommendations. J Nutr Health Aging. 2020;24(9):938–47.
Shafie S, Subramaniam M, Abdin E, Vaingankar JA, Sambasivam R, Zhang Y, Shahwan S, Chang S, Jeyagurunathan A, Chong SA. Help-seeking patterns among the general population in singapore: results from the Singapore mental health study 2016. Adm Policy Ment Health Ment Health Serv Res. 2021;48(4):586–96. https://doi.org/10.1007/s10488-020-01092-5 .
Silva M, Antunes A, Azeredo-Lopes S, Cardoso G, Xavier M, Saraceno B, Caldas-de-Almeida JM. Barriers to mental health services utilisation in Portugal–results from the National mental health survey. J Mental Health. 2022;31(4):453–61. https://doi.org/10.1080/09638237.2020.1739249 .
Stecker T, Fortney J, Hamilton F, Ajzen I. An assessment of beliefs about mental health care among veterans who served in Iraq. Psychiatric Serv. 2007;58:1358–61.
Sodhi-Berry N, Preen DB, Alan J, Knuiman M, Morgan VA, Corrao G, Monzio Compagnoni M, Valsassina V, Lora A. Pre-sentence mental health service use by adult offenders in Western Australia: baseline results from a longitudinal whole-population cohort studyAssessing the physical healthcare gap among patients with severe mental illness: large real-world investigati. Crim Behav Ment HealthBJPsych Open. 2014;247(35):204–21. https://doi.org/10.1192/bjo.2021.998 .
Spinogatti F, Civenti G, Conti V, Lora A, Bahji A. Ethnic differences in the utilization of mental health services in Lombardy (Italy): an epidemiological analysisIncidence and correlates of opioid-related psychiatric emergency care: a retrospective, multiyear cohort study. Soc Psychiatry Psychiatr Epidemiol J Opioid Manage. 2015;5016(13):59223–65226. https://doi.org/10.5055/jom.2020.0572 .
The World Bank. Population, total, population, total - low income, middle income, high income. Washington, D.C.: The World Bank (producer and distributor); 2022. https://data.worldbank.org/indicator/SP.POP.TOTL?end=2022&locations=XM-XP-XD&start=1960&view=chart
Thornicroft G. Stigma and discrimination limit access to mental health care. Epidemiol Psychiatric Sci. 2008;17(1):14–9. https://doi.org/10.1017/S1121189X00002621 .
Thornicroft G, Tansella M. Components of a modern mental health service: a pragmatic balance of community and hospital care: overview of systematic evidence. Br J Psychiatry. 2004;185:283–90.
Tiwari SK, Wang J. Ethnic differences in mental health service use among White, Chinese, south Asian and South East Asian populations living in Canada. Soc Psychiatry Psychiatr Epidemiol. 2008;43(11):866–71. https://doi.org/10.1007/s00127-008-0373-6 .
Volkert J, Andreas S, Härter M, Dehoust MC, Sehner S, Suling A, Ausín B, Canuto A, Crawford MJ, Ronch D, Grassi C, Hershkovitz L, Muñoz Y, Quirk M, Rotenstein A, Santos-Olmo O, Shalev AB, Strehle AY, Weber J, Schulz K. Predisposing, enabling, and need factors of service utilization in the elderly with mental health problems. Int Psychogeriatr. 2018;30(7):1027–37. https://doi.org/10.1017/S1041610217002526 .
Wang N, Xie X. Associations of health insurance coverage, mental health problems, and drug use with mental health service use in US adults: an analysis of 2013 National Survey on Drug Use and Health. Aging Ment Health. 2019;23(4):439–46. https://doi.org/10.1080/13607863.2018.1441262 .
Wang PS, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Borges G, Bromet EJ, et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet. 2007;370(9590):841–50.
Wei Z, Hu C, Wei X, Yang H, Shu M, Liu T. Service utilization for mental problems in a metropolitan migrant population in China. Psychiatr Serv. 2013;64(7):645–52. https://doi.org/10.1176/appi.ps.201200304 .
Werlen L, Puhan MA, Landolt MA, Mohler-Kuo M. Mind the treatment gap: the prevalence of common mental disorder symptoms, risky substance use and service utilization among young Swiss adults. BMC Public Health. 2020;20(1):1470. https://doi.org/10.1186/s12889-020-09577-6 .
Wettstein A, Tlali M, Joska JA, Cornell M, Skrivankova VW, Seedat S, Mouton JP, van den Heuvel LL, Maxwell N, Davies MA, Maartens G, Egger M, Haas AD. The effect of the COVID-19 lockdown on mental health care use in South Africa: an interrupted time-series analysis. Epidemiol Psychiatr Sci. 2022;31:e43. https://doi.org/10.1017/s2045796022000270 .
Whitley R, Wang J, Fleury MJ, Liu A, Caron J. Mental health status, health care utilisation, and service satisfaction among immigrants in montreal: an epidemiological comparison. Can J Psychiatry. 2017;62(8):570–9. https://doi.org/10.1177/0706743716677724 .
Warner EL, Kent EE, Trevino KM, Parsons HM, Zebrack BJ, Kirchhoff AC. Social well-being among adolescents and young adults with cancer: a systematic review. Cancer. 2016;122:1029–37.
Wells G, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Department of Epidemiology and Community Medicine, University of Ottawa, Canada. Canada: University of Ottawa; 2000. Available at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.Asp
Westerhof GJ, Keyes CL. Mental illness and mental health: the two continua model across the lifespan. J Adult Dev. 2010;17(2):110–9. https://doi.org/10.1007/s10804-009-9082-y .
World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992.
Yang KG, Rodgers CRR, Lee E, B LC. Disparities in mental health care utilization and perceived need among Asian americans: 2012–2016. Psychiatr Serv. 2020;71(1):21–7. https://doi.org/10.1176/appi.ps.201900126 .
Rosenberg S, Hickie AMI. Making better choices about mental health investment: the case for urgent reform of Australia’s better access program. Australian New Z J Psychiatry. 2019;53(11):1052–8. https://doi.org/10.1177/0004867419865335 .
World Bank. World Bank income groups [dataset]. World Bank, Income Classifications [original data]. 2023. Retrieved May 2, 2024 from https://ourworldindata.org/grapher/world-bank-income-groups .
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
The National Centre for Epidemiology and Population Health, Australian National University, Canberra, Australia
Yunqi Gao, Richard Burns, Liana Leach & Miranda R. Chilver
School of Psychology, Deakin University, Melbourne, Australia
Peter Butterworth
Department of Health, Economics, Wellbeing and Society, Australian National University, Canberra, Australia
You can also search for this author in PubMed Google Scholar
Contributions
YG was responsible for the study design, title and abstract screening, full-text screening, and writing the manuscript. PB, RB, and LL contributed to the study design, title and abstract screening, full-text screening, and offered comments and detailed feedback on the draft paper. MC also helped with the title and abstract screening, full-text screening, and provided comments and detailed feedback on the draft paper.
Corresponding author
Correspondence to Yunqi Gao .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Gao, Y., Burns, R., Leach, L. et al. Examining the mental health services among people with mental disorders: a literature review. BMC Psychiatry 24 , 568 (2024). https://doi.org/10.1186/s12888-024-05965-z
Download citation
Received : 18 February 2024
Accepted : 15 July 2024
Published : 20 August 2024
DOI : https://doi.org/10.1186/s12888-024-05965-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health services
- Service use
- Mental disorder
- Systematic review
BMC Psychiatry
ISSN: 1471-244X
- General enquiries: [email protected]
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


Mindfulness-based interventions: an overall review
Dexing zhang, eric k p lee, eva c w mak, samuel y s wong.
- Author information
- Article notes
- Copyright and License information
Corresponding address. 4/F, JC School of Public Health and Primary Care, Prince of Wales Hospital, Shatin, N.T., Hong Kong.E-mail: [email protected]
Received 2020 Aug 16; Revised 2020 Dec 27; Accepted 2021 Feb 2.
This article is made available via the PMC Open Access Subset for unrestricted re-use and analyses in any form or by any means with acknowledgement of the original source. These permissions are granted for the duration of the COVID-19 pandemic or until permissions are revoked in writing. Upon expiration of these permissions, PMC is granted a perpetual license to make this article available via PMC and Europe PMC, consistent with existing copyright protections.
This article is published and distributed under the terms of the Oxford University Press, Standard Journals Publication Model ( https://academic.oup.com/journals/pages/open_access/funder_policies/chorus/standard_publication_model )
Introduction
This is an overall review on mindfulness-based interventions (MBIs).
Sources of data
We identified studies in PubMed, EMBASE, CINAHL, PsycINFO, AMED, Web of Science and Google Scholar using keywords including ‘mindfulness’, ‘meditation’, and ‘review’, ‘meta-analysis’ or their variations.
Areas of agreement
MBIs are effective for improving many biopsychosocial conditions, including depression, anxiety, stress, insomnia, addiction, psychosis, pain, hypertension, weight control, cancer-related symptoms and prosocial behaviours. It is found to be beneficial in the healthcare settings, in schools and workplace but further research is warranted to look into its efficacy on different problems. MBIs are relatively safe, but ethical aspects should be considered. Mechanisms are suggested in both empirical and neurophysiological findings. Cost-effectiveness is found in treating some health conditions.
Areas of controversy
Inconclusive or only preliminary evidence on the effects of MBIs on PTSD, ADHD, ASD, eating disorders, loneliness and physical symptoms of cardiovascular diseases, diabetes, and respiratory conditions. Furthermore, some beneficial effects are not confirmed in subgroup populations. Cost-effectiveness is yet to confirm for many health conditions and populations.
Growing points
Many mindfulness systematic reviews and meta-analyses indicate low quality of included studies, hence high-quality studies with adequate sample size and longer follow-up period are needed.
Areas timely for developing research
More research is needed on online mindfulness trainings and interventions to improve biopsychosocial health during the COVID-19 pandemic; Deeper understanding of the mechanisms of MBIs integrating both empirical and neurophysiological findings; Long-term compliance and effects of MBIs; and development of mindfulness plus (mindfulness+) or personalized mindfulness programs to elevate the effectiveness for different purposes.
Keywords: mindfulness-based interventions, biopsychosocial health, safety, ethics, compliance, mechanisms
Mindfulness and mindfulness-based interventions
Mindfulness is a moment-by-moment awareness of thoughts, feelings, bodily sensations and surrounding environment. Being mindful is related to be open, nonjudgmental, friendly, curious, accepting, compassionate and kind. 1 Mindfulness practices aim to cultivate mindfulness state. These practices can be formal (e.g. breathing, sitting, walking, body scan) or informal (e.g. mindfulness in everyday life). Many mindfulness-based intervention (MBI) programmes have been established. Among all the MBIs, mindfulness-based stress reduction (MBSR), which was launched by Jon Kabat-Zinn in 1979, 2 and mindfulness-based cognitive therapy (MBCT) by Segal, Teasdale and Williams based on MBSR, 3 , 4 are the two most widely adopted MBIs. These two programmes include eight weekly mindfulness sessions with one-day retreat.
Mindfulness is rooted in Buddhist traditions. However, it has become popular in recent years among various secular populations in healthcare, educational and workplace settings: from pre-school children to older adults across the world. Publications on mindfulness have increased dramatically in the recent decade. The publications on mindfulness is starting to be more comparable to publications on cognitive behavioural therapy (CBT), which is one of the most widely used psychotherapies ( Fig. 1 ).
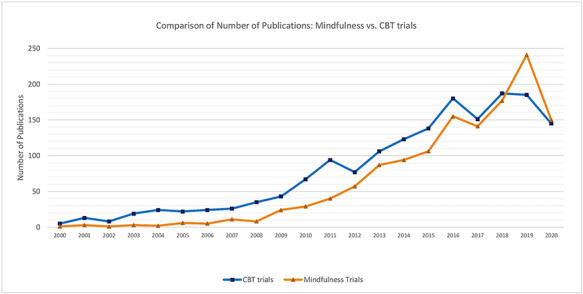
Comparison on number of publications: mindfulness vs. CBT trials (by August 2020) [Note: Search terms included (‘mindful* or meditate*’ AND ‘trial or random or random* control* trial*’); (‘cognitive behavioural therapy or cognitive behavioural therapy or CBT’ AND ‘trial or random or random* control* trial*’) in Title; Databases included MEDLINE, EMBASE and PsycINFO.]
Methods used for identifying relevant evidence
Literature in English was searched in MEDLINE, EMBASE, CINAHL, PsycInfo, AMED, Web of Science and Google Scholar using keywords including ‘mindfulness’, ‘meditation’ and ‘review’, ‘meta-analysis’ or their variations, with no restrictions on the year of publication. The search was conducted in July 2020. In choosing evidence, these general principals were applied: (i) published in more recent years if similar reviews were identified; (ii) included randomized controlled trials or meta-analysis in the review; (iii) presented with more conclusive conclusions. Literature with other types of study design (e.g. randomized controlled trials, cohorts, cross-sectional studies) were also manually searched and included when no systematic review was found or when considered as appropriate. However, while it was intent to include all important literature in a certain area, the review might not exhaust all relevant literature but had only selected key references of interest that we thought to be most pertinent and insightful for a specific topic.
Effects on mental health
MBIs have been shown to be efficacious in improving some of the common mental health problems. 5
Depression and anxiety
For depression and anxiety, the efficacy of MBIs is sufficiently confirmed with meta-analyses demonstrating moderate to strong effect sizes for the reduction of the two conditions. 6–8 The effects were also applicable during pregnancy, where a systematic review showed that MBIs helped reducing perinatal anxiety of moderate to large magnitude; however, the effects were less consistent in terms of reducing perinatal depression. 9 The trending web-based interventions on mindfulness have also shown effectiveness in reducing depression and anxiety among people diagnosed with anxiety disorders as well. 10 It was unclear, however, whether the benefits of mindfulness practices as a stand-alone intervention still exist, as it is difficult to dismantle the effects from social interaction and psychoeducation, which are the other components integrated in many MBIs (e.g. group MBCT), from standalone mindfulness practices. Therefore, a recent meta-analyses 11 of 18 eligible studies investigated the gap, and has demonstrated that even mindfulness practice itself (e.g. breathing space, body scan, sitting meditation, soundscan) had small to medium effects on both anxiety (SMD = 0.39; CI: 0.22, 0.56; PI: 0.07, 0.70; P < .001, I 2 = 18.90%) and depression (SMD = 0.41; CI: 0.19, 0.64; PI: −0.05, 0.88; P < .001; I 2 = 33.43%).
Current evidence overall supports a moderate effect of MBIs on reducing stress; however, more robust studies are needed to make clear conclusions among different populations. A meta-analysis of five randomized control trials tested the effects of MBIs on cortisol levels, a stress-mediated hormone, and found that there may be a beneficial effect in healthy adult populations. 12 Yet, the overall effect size was moderately low ( g = 0.41; P = 0.025). 12 On the other hand, another meta-analysis indicated that there was a significant, medium effect of meditation interventions on cortisol levels, but the effect was only present for at-risk samples such as those living in stressful life situations. 13 There are also studies done among specific populations such as tertiary education students 14 and older adults, 15 showing inconclusive results. Among tertiary education students, the effect sizes of interventions for stress were moderate ( g = 0.42, 95% CI: 0.27–0.57), but most studies were of poor quality. 14 Among older adults, no clear evidence was found that MBIs can reduce the perception of stress. 15
The current evidence on the effects of MBIs on insomnia and sleep disturbance is promising. A meta-analysis concluded that MBIs are effective in improving symptoms of insomnia and sleep quality when compared to attention/education and waitlist control with medium to large effects ( g = 0.67, 95% confidence interval [CI] = 0.30–1.05) and that the effects seem to endured at 3 months postintervention ( g = 1.06, 95% CI = 0.48–1.64). 16 Several other meta-analyses also found similar results, which all showed significant improvement in insomnia or sleep quality as measured by the Pittsburgh Sleep Quality Index. 17–19
Eating disorders
Current studies provided preliminary evidence on the potential effects of MBIs on eating disorders (EDs). One systematic review and meta-analysis showed a within-condition effect of MBIs on ED symptoms, emotional eating, negative affect and body dissatisfaction, and on the body mass index (BMI) in anorectic and bulimic participants relative to pre-assessment. 20 Another systematic review and meta-analysis also found that MBIs may help reducing body image concern and negative affect, while promoting body appreciation. 21 Both authors concluded that more rigorous studies are needed before the efficacy of MBIs on EDs can be confirmed. 20 , 21
Literature supports the efficacy of MBIs in both substance and behavioural addictions. A systematic review of 54 randomised controlled trials found that MBIs were successful in the reduction of dependence, craving and other symptoms related to addiction, and the improvement of mood state and emotion dysregulation. 22 Two other meta-analytic results also revealed significant small-to-large effects of MBIs in reducing levels of perceived craving, 23 , 24 severity of stress, 23 , 24 frequency and severity of substance misuse, 23 anxiety and depressive symptoms, 24 negative affectivity, 24 and post-traumatic symptoms 24 for the treatment of substance misuse. Although the effectiveness is promising, more research is needed especially on longer follow-up assessments and among diverse populations.
It seems that MBIs have potential benefits for people with psychosis, but further research is warranted. 25 A systematic review and meta-analysis on 434 patients found short-term moderate evidence of MBIs on total psychotic symptoms, positive symptoms, hospitalization rates, duration of hospitalization, and mindfulness as short-term effects and total psychotic symptoms and duration of hospitalization as long-term effects in patients with psychosis. 26 Another systematic review also confirmed that MBIs are feasible for individuals with psychosis and it could provide a number of significant benefits over routine care such as improving negative symptoms and measures of functioning. 27 Future large trials adopting randomization procedure are suggested to gain greater insight into the mechanisms and long-term effectiveness of MBIs among people with psychosis.
Post-traumatic stress disorder
MBIs among post-traumatic stress disorder (PTSD)-diagnosed participants were less conclusive. A systematic review and meta-analysis of 10 trials on meditation interventions have shown that the effects for PTSD were positive but not statistically significant. 28 The variety of meditation intervention types, the short follow-up times and the quality of studies limited the analyses. 28 Other systematic reviews reported similar findings, where they reported MBIs such as mindfulness, yoga and relaxation studies maybe useful for the mind–body treatments for PTSD but many of the trials suffered from methodologic weaknesses or were of low to moderate methodological rigor. 29 , 30 Further high-quality studies are needed on MBIs among PTSD-diagnosed participants in order to increase confidence in its effectiveness.
Attention-deficit hyperactivity disorder
There is a need for further research before determining the effectiveness of MBIs on attention-deficit hyperactivity disorder (ADHD) despite current studies showed that it can be a promising intervention. A systematic review and meta-analysis has found statistically significant effect of MBIs in decreasing the severity of ADHD core symptoms such as inattention, hyperactivity or impulsivity (children/adolescents: Hedge’s g = −0.44, 95% CI −0.69 to −0.19, I 2 0%; adults: Hedge’s g = −0.66, 95% CI –1.21 to −0.11, I 2 81.81%). 31 However, the authors concluded that there is insufficient methodologically sound evidence to support the effectiveness due to limited number of studies, heterogeneity across studies and high risk of bias. 31 Similar results and conclusions were also noted in several other systematic reviews. 32–34
Autism spectrum disorders
Current literature on MBIs for people with autism spectrum disorders (ASD) or their carers is very limited. A systematic review done in 2017 analysed 16 eligible studies but definitive recommendations could not be made on the effects of MBIs for people with ASD or their carers. 35 This was because those studies included very diverse age groups and outcome measures, including behavioural, social and psychological symptoms, as well as the subjective well-being of children and adults with ASD and their parents. 35 Overall, there may be some potential benefits of MBIs among people with ASD, these include: reducing anxiety, 35 , 36 thought problems, 35 , 36 rumination, 35 aggression, 36 parental stress 37 , and increasing subjective well-being 38 as well as parental psychological wellbeing. 37
The current available evidence to support MBIs on cognition is weak. A systematic review conducted in older adults with mild cognitive impairment found that MBIs improved participant’s cognitive function and everyday activities functioning. 39 However, the available studies had small sample sizes, lack of control comparison and lack of follow-up to understand the effects on preventing progression of dementia. 39 Further high-quality trials and on different populations are required to confirm the effectiveness of the benefits of MBIs on cognitive function.
Effects on physical health
MBIs can provide positive effects on physical health and evidence is strong regarding benefits of MBIs on the psychological symptoms among people with chronic diseases.
The evidence of benefits of MBIs on pain is abundant among different populations. 40 , 41 A systematic review and meta-analysis of 30 RCTs on chronic pain conducted in 2017 showed improvement on chronic pain management after mindfulness meditation intervention. 40 The percent change of the mean in pain for intervention subjects was −0.19% (SD, 0.91; min, −0.48; max, 0.10), which was significantly higher than the control groups (−0.08% (SD, 0.74; min, −0.35; max, 0.11)). 40 A network meta-analysis found MBSR is effective for chronic pain, and the effects are not significantly different between MBSR and CBT; though more studies are needed to confirm this. 41 Furthermore, for the effects of brief MBIs with a total contact time of less than 1.5 hours, current evidence is inadequate to confirm the effectiveness on acute and chronic pain. 42
Hypertension and cardiovascular diseases
A few systematic reviews and meta-analyses suggested that MBIs can reduce blood pressure (BP). 43–45 A systematic review and meta-analysis of five studies on MBSR showed reduction on systolic and diastolic blood pressure in people with hypertension or elevated blood pressure. However, most of the studies were related to clinical blood pressure only and evidence on ambulatory blood pressure is needed. 43 A systematic review among people with non-communicable diseases found systolic BP was reduced after the eight-week MBSR (−6.90 mmHg [95% CI: −10.82, −2.97]), followed by the 12-week breathing awareness meditation (−4.10 mmHg [95% CI: −7.54, −0.66]), and eight-week mindfulness-based intervention (−2.69 mmHg [95% CI: −3.90, −1.49]) and diastolic BP was reduced after eight-week MBSR (−2.45 mmHg [95% CI: −3.74, −1.17]) and the eight-week MBI (−2.24 mmHg [95% CI: −3.22, −1.26]). 44 Another systematic review among patients with CVD in 2020 showed benefits on systolic BP ( d + = 0.89, 95% CI = 0.26, 1.51) and psychological symptoms ( d + s = 0.49–0.64), but not diastolic BP. 45 Another systematic review by Zou evaluated the effect of mindful exercises for patients after stroke showed significantly improvement on the sensorimotor function on lower limb (SDM = 0.79; 95% CI, 0.43–1.15; I 2 = 62.67%) and upper limb (SDM = 0.7; 95% CI, 0.39–1.01; I 2 = 32.36%). 46 Further studies can assess gait speed, leg strength, aerobic endurance, motor function, cognitive function and gait parameters.
Weight control and obesity
Overweight and obesity are a significant health risk factor leading to tremendous disease burden due to the associated comorbidities. 47 Mindful eating is an effective intervention for weight control, especially among people with binge eating or emotional eating tendency. Mindful eating might have longer-term effects when comparing to conventional diet programmes, which involves limiting energy intake and restricting food choices, because mindful eating tends to be more sustainable and also deal with emotional problems that may influence unhealthy diet. 48–52 A systematic review and meta-analysis in 2019 evaluated ten mindful eating and weight control studies, and found significant weight reduction after mindful eating program when compared with control groups (−0.348 kg, 95% CI: −0.591 to −0.105). 53 Furthermore, effects of MBIs were equal to conventional diet programmes. 53 However, limitations were found in the studies, such as short duration and biased samples (unbalanced sex ratio, source and place of living). Hence, further studies with longer duration and modifications of subject selection could be beneficial to evaluate long-term improvement among different populations.
The current evidence to support the effect of MBIs on the physiological outcomes of diabetes is inconclusive. One systematic review found mixed results on the effectiveness of MBIs for physiological outcomes (glycaemic control and blood pressure) on both types 1 and 2 diabetes patients. 54 Another systematic review and meta-analysis found that meditative movements significantly improved the glycaemic control including fasting blood glucose, glycated haemoglobin (HbA1c) and postprandial blood glucose in type 2 diabetes mellitus (T2DM) patients. 55 Nonetheless, the authors noted it is difficult to conclude the extent to which MBIs are effective because of the small sample size, short duration and diverse delivery methods within the published studies. 55 Apart from glycaemic control, systematic reviews also found improvement in psychological symptoms such as anxiety, 54 distress symptoms, 54 , 56 depression 54 , 57 and quality of life. 57 Further research addressing the limitations is necessary to gauge the efficacy of MBIs for diabetes.
There may be some benefits of MBIs on the physical health outcomes in cancer patients especially on cancer-related fatigue and pain, besides psychological benefits. 58 , 59 A systematic review and meta-analysis found that MBIs led to a statistically significant reduction in cancer-related fatigue (CRF) score among cancer patients (SMD = -0.51, 95%CI [−0.81–0.20]), 59 especially among lung cancer patients. 60 Apart from CRF, a range of other outcomes such as improvements in sleep disturbances, pain and other psychological symptoms including anxiety, depression, fear of cancer recurrence were also found in another systematic review and meta-analysis. 61 Overall, although MBIs appeared effective in reducing CRF and other symptoms, further high-quality studies are still required to provide additional insights and to confirm the existing evidence.
Respiratory health (COPD, asthma, etc.)
The effectiveness of MBIs on respiratory health remained unclear. A systematic review and meta-analysis of 16 studies found that meditative movement may have the potential to enhance lung function and physical activity in Chronic obstructive pulmonary disease (COPD) patients. 62 When compared to nonexercised group, the intervention enhanced the 6-minute walking distance (3 months: mean difference [MD] = 25.40 m, 95% CI: 16.25–34.54; 6 months: MD = 35.75 m, 95% CI: 22.23–49.27), as well as functions on forced expiratory volume in 1 s (FEV 1 ) (3 months: MD = 0.1 L, 95% CI: 0.02–0.18; 6 months: MD = 0.18 L, 95% CI: 0.1–0.26). 62 However, taking into considerations of the limitations of the studies such as small sample sizes, inconsistency in study quality and the diverse style of meditative movement in studies, the authors noted that further trials are needed to substantiate the findings. 62 Other systematic reviews and meta-analyses on COPD 65 and asthma 63 also concluded that further high-quality trials are needed to confirm the effectiveness of MBIs on respiratory health. 63 , 64
Effects on social health and prosocial behaviours
There is evidence supporting effects of MBIs on social health and prosocial behaviours (i.e. voluntary behaviour intended to benefit another). 65 , 66 A systematic review found medium effects on prosocial behaviours for both correlational and intervention studies, and the effects are similar to known and unknown others. 65 The results suggest that mindfulness fosters ethical and cooperative behaviour across a range of interpersonal contexts and may reduce intergroup biases. 65 Another recent review with 29 studies also find similar results with small to medium effect sizes, suggesting MBIs reliably improve compassionate helping and reduces prejudice and retaliation. 66 Furthermore, MBIs can effectively reduce anger, 67 violence 68 and aggression. 69 It also may help improve social and ecological sustainability, by improving individuals’ subjective well-being and benign connection with others, the society and the nature. 70
Loneliness and social isolation are an increasing public health concern, especially during COVID-19 and for older adults. Some preliminary studies indicated that mindfulness training might have positive effect in mitigating loneliness. 71–74 A preliminary study showed MBSR effectively reduced loneliness in older adults. 71 Another study found positive effect on mitigating the loneliness of women with HIV. 72 A study among Chinese college students found a positive relationship between mindfulness and loneliness reduction. 73 Lindsay et al. raised that mindfulness both reduced loneliness and increased social interactions in daily life compared with an active control program, in the experiment of smartphone-based mindfulness training. 74
Mindfulness in different settings
Mindfulness among professionals in healthcare settings.
Mindfulness has been adopted as a stress management tool for healthcare professionals, with a medium effect size was found ( r = 0.342, CI = 0.202–0.468). 75 Systematic reviews and meta-analyses have shown the promising effects on the other psychological indicators among healthcare professionals and students, e.g. reducing depression and burnout and improving emotional resilience. 76 , 77 However, both benefits and challenges (time limitations and feasibility) were perceived at the same time, 78 and there are insufficient studies on indirect outcomes of MBIs among healthcare professionals, e.g. how it may influence professional-patient communication, relationship and patient outcomes.
Mindfulness in schools
Mindfulness programmes in schools are increasingly popular. Many different school mindfulness programmes (e.g. ‘.b’, mindful schools, well and resilience program) have been implemented across the world. 79 , 80 These programmes can target at students, teachers, and even parents or caregivers. 81 Recent systematic reviews found MBIs hold promises in particular in improving resilience to stress, cognitive performance such as attention, and emotional problems in children and youths. 82 , 83 The reviews showed a significant effect for resilience in regards to well-being, positive and constructive emotions or affect, social skills and positive relationships, self-concept and self-esteem. The effects (effect size = 0.36–0.80) are comparable or better than the effects (overall effect size = 0.30) of school-based social and emotional learning programs as revealed in the meta-analysis. 84 It is promising in applying MBIs as a life skill within pre-, elementary, middle or high schools. Students might be benefited from 90-min mindfulness practice per week (i.e. 18 minutes on average per day). 85 In building up mindful schools, a whole school approach is valuable to integrate mindfulness through the curriculum, professional development of teachers, leadership practice and across the learning environment. 86
Mindfulness in workplace
A systematic review on 58 592 adults from nonclinical samples showed that trait mindfulness was positively associated with confidence, job satisfaction, performance and interpersonal relations, and negatively associated with burnout and work withdrawal. 87 A recent systematic review on 56 randomized controlled trials shows that MBIs are beneficial to employees in reducing stress, burnout, mental distress and somatic complaints, while improving mindfulness, well-being, compassion and job satisfaction—all with small to large effect sizes ranging from Hedge’s g = 0.32–0.77, but effects on work engagement and productivity were limited by low number of studies. 88
Cost-effectiveness of MBIs
MBIs are likely to be cost-effective and value for money as it can be provided in group format or as self-help interventions, 89 and it can also be integrated into educational programmes for clinicians, educationalists and other professionals to directly and indirectly benefit themselves, students, their clients and people around them. 90 While the benefits are almost equal to cognitive behavioural interventions, mindfulness may require less professional training and take less time for both workers and clients to master, and they are probably less expensive to provide. 91 For example, studies showed that the training cost for teachers in a mindfulness training program ranged from US$515 to US$1850 per teacher depending on the number of teachers being trained and the ancillary and opportunity costs. 92 However, more studies are needed to confirm their cost-effectiveness. Preliminary evidence support its cost-effectiveness, 93 including but not limited to pain in breast cancer, 94 fibromyalgia, 95 low back pain 96 and caregiver training. 97 It is also a cost-saving treatment for improving quality of life for distressed cancer patients using both online or face-to-face MBCT. 98 However, uncertainties existed in workplace, 99 and yet it needs cost-effectiveness studies on many other health problems aswell.
Compliance of MBIs
Non-compliance is a barrier to learning mindfulness 100 and research shows that the drop-out rate can reach 25% or higher. 101 , 102 Inconsistent findings were shown in previous studies regarding who might or might not comply with MBIs. Although in general, women, those with higher openness to experience, higher resistance to change and severer symptoms showed higher levels of compliance. 103 , 104 The relationship between participants’ compliance and intervention outcomes is inconsistent, ranging from no correlation to a positive correlation, 105 although one recent systematic review based on 28 studies found a small but significant association between participants’ self-reported home practice and intervention outcomes ( r = 0.26, 95% CI: 0.19–0.34). 106 In terms of factors associated with better compliance, a good natural setting is found to be important, especially for beginners. 100 And some researchers suggested to identify meditation exercises that can balance optimizing effectiveness and enhancing adherence to strengthen the compliance to MBIs. 107 It still needs more research to understand who might comply with and benefit from which type of MBIs the most, and to look into factors and strategies enhancing compliance.
Mechanisms of MBIs
Studies suggested that the mechanisms of MBIs include changes in mindfulness, rumination, worry, self-regulation, compassion or meta-awareness, which predicted or mediated the treatment effects, which are theoretically predicted mechanisms of MBIs. 108–111 Preliminary results also suggested alterations in attention, memory specificity, self-discrepancy, emotional reactivity and momentary positive and negative affect, can be part of the mechanisms. 108 Recently, the mindfulness-to-meaning (MMT) approach has also been recognized as providing a theoretical framework to investigate specific mindfulness components and their contributions to the positive health outcomes. 112 , 113 In this approach, the iterative cycle of appraisal, decentering and metacognition would lead to positive reappraisals of broader contexts that extinguish negative affect and promote positive effects and eudaimonic meaning in life. 112 , 113 Yet, there are still many unknowns regarding the mechanisms ofMBIs.
Neurophysiological findings
The changes on brain and biomarkers of immune function and stress might have provided neurophysiological basis for explaining the positive effects of MBIs. Systematic reviews have consistently found effects of MBIs on brain activity that involves in processing self-relevant information, self-regulation, focused problem-solving, adaptive behaviour and interoception, among both healthy populations and patient groups. 114–119 Eight brain regions key to meta-awareness (frontopolar cortex), body awareness (sensory cortices and insular), memory consolidation and reconsolidation (hippocampus), self and emotion regulation (anterior and mid cingulate; orbitofrontal cortex), and intra- and interhemispheric communication (superior longitudinal fasciculus; corpus callosum) consistently altered with a medium effect size after mindfulness practices. 118 In expert meditators, both functional and structural brain modifications have been induced, especially in areas involved in self-referential processes such as self-awareness and self-regulation, though not enough evidence suggests structural brain modifications in short-term meditators. 114 Among people with major depressive disorders, MBIs have also modulatory effects on several brain regions (e.g. the prefrontal cortex, the basal ganglia, the anterior and posterior cingulate cortices and the parietal cortex). 115 Another systematic review on 78 functional neuroimaging (fMRI and PET) studies of meditation found patterns of brain activation and deactivation for common styles of meditation (focused attention, mantra recitation, open monitoring and compassion/loving-kindness), with medium effects for both activations ( d = 0.59) and deactivations ( d = −0.74), suggesting potential practical significance. 116 The systematic review on EEG results suggested that mindfulness is associated with increased alpha and theta power in both healthy populations and patient groups, which may signify a relaxed alertness state contributing to mental health. 117
Systematic reviews on RCTs revealed that mindfulness meditation have effects on stress and immune-related physiological markers of inflammation, cell-mediated immunity and biological aging: reductions in the activity of the cellular transcription factor NF-kB, reductions in circulating levels of C-reactive protein, increases in CD4+ T cell count (in HIV-diagnosed individuals), and increases in telomerase activity. 120 Another systematic review on RCTs found that, compared to an active control (relaxation, exercise or education), mindfulness meditation reduced physiological markers of stress, such as cortisol, C-reactive protein, systolic blood pressure, heart rate, triglycerides and tumour necrosis factor-alpha, in various populations. 121 And a greater number of hours of meditation are associated with a greater impact on telomere biology. 122 However, these tentative findings need further replication and the review authors call for studies to include physiological markers as primary outcome of RCTs. 120–123
Ethics of MBIs
Ethical questions are fundamental and essential in guiding the future directions of MBIs to use the right mindfulness rightly, and also the application of MBIs should not overstate the organizational and social determinants of ill health. In the books of ‘Practitioner’s Guide to Ethics and Mindfulness-Based Interventions’ (edited by Lynette Monteiro, Jane Compson and Frank Musten) and ‘Handbook of Ethical Foundations of Mindfulness’ (edited by Stanley Steven, Ronald Purser and Nirbhay Singh), ethical questions of mindfulness are discussed extensively. Many questions on ethics are yet to be addressed for MBIs. For example, paradox in teaching mindfulness in business and military settings, depriving superiors to make use of subordinates through mindfulness regardless of other organizational factors causing work-related stress or depression. On the other hand, there are many virtues and strengths in MBIs in providing personally meaningful and prosocial values, 124 and MBIs can improve ethical standards, that mindfulness promotes greater ethical intentions and lesser ethical infractions, with more mindful people revealed a greater emphasis on moral principles than those who are less mindful. 125
Safety of MBIs
MBIs are regarded as relatively safe interventions. 126 Like many other psychological intervention trials, adverse events and adverse effects of MBIs are largely underreported. A previous systematic review on safety of MBSR and MBCT indicated that fewer than one in five trials had mentioned the monitoring of adverse effects. 126 Program-related factors, participant-related factors, and clinician- or teacher-related factors are potential sources of adverse effects. 1 , 126–132 A safety checklist is yet needed to be built based on previous studies and empirical experiences. Practitioners and researchers in future MBI programmes are advised to report the potential adverse events using such a checklist, and also continue to take safety precautions such as screening and caring for vulnerable individuals. These individuals could be those with PTSD, seizure disorder/epilepsy, acute psychosis, mania, suicidality or other health problems of concern. 133
Future directions
Despite the increasing trend of mindfulness studies and applications, there are still many areas need exploration. First, higher quality of research studies is needed. The most frequent limitations mentioned in the systematic reviews on effectiveness and cost-effectiveness of MBIs are low quality of study design, small sample size, short follow-up period, and inconsistent terminology and measurement tools. Future more robust studies are needed to address these caveats. Second, more studies on online MBIs intervention and training are needed to understand if online alternatives have equal or better effects and cost-effectiveness, though preliminary benefits are seen. 10 , 134 , 135 Online alternatives might be important, especially given the pandemic of COVID-19. Third, more understanding of the mechanisms by integrating both empirical findings and neurophysiological findings. Fourth, more research is needed to explore the acceptance and compliance of MBIs to understand who might benefit more from MBIs, and barriers and respective strategies (e.g. better meditation environment) for improving the acceptance and compliance, taken into considerations of safety issues and ethical concerns. And a closer look at the long-term compliance is needed. This may call for large-scale cohort studies on MBIs. Fifth, develop more mindfulness related research and services guidelines and regulations, e.g. on adverse events monitoring and safety guarantee, and qualifications of mindfulness teachers. These might be important when MBIs are provided as a collective action in schools, companies or organizations. Sixth, exploration of Mindfulness Plus (Mindfulness+), i.e. combination of MBIs with other effective interventions (for example, mindfulness plus medications, mindfulness plus behavioural activation, 136 mindfulness plus reflection training 137 and mindfulness plus Qigong movement therapy 138 ), or exploration of personalized/individualized mindfulness-based interventions for individuals with different characteristics and needs, selecting from many different mindfulness programs. This would provide more potential to improve the effects of MBIs for different goals.
MBIs are effective for many common mental, physical and social health conditions among different populations. Beneficial effects of MBIs have been found on depression, anxiety, stress, insomnia, addiction, psychosis, pain, hypertension, weight control, cancer-related symptoms and prosocial behaviours. Current evidence suggested MBIs can be beneficial for healthcare professionals and within schools and workplaces although more studies are still needed to look into its efficacy on many different biopsychosocial health conditions. MBIs are relatively safe. Ethical aspects should always be taken into account during mindfulness-based trainings and interventions. Mechanisms of MBIs have been suggested in both empirical and neurophysiological findings. Cost-effectiveness is found for some health problems (e.g. breast cancer, fibromyalgia, low back pain or caregiver training). More high-quality studies with adequate sample size and longer follow-up duration are needed to confirm its effectiveness and cost-effectiveness in many other problems and among sub-groups. Some other areas needing additional research are suggested in this review.
Contributor Information
Dexing Zhang, JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong SAR, China; Thomas Jing Mindfulness Centre for Research and Training, The Chinese University of Hong Kong, Hong Kong SAR, China.
Eric K P Lee, JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong SAR, China; Thomas Jing Mindfulness Centre for Research and Training, The Chinese University of Hong Kong, Hong Kong SAR, China.
Eva C W Mak, JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong SAR, China; Thomas Jing Mindfulness Centre for Research and Training, The Chinese University of Hong Kong, Hong Kong SAR, China.
C Y Ho, JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong SAR, China; Thomas Jing Mindfulness Centre for Research and Training, The Chinese University of Hong Kong, Hong Kong SAR, China.
Samuel Y S Wong, JC School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong SAR, China; Thomas Jing Mindfulness Centre for Research and Training, The Chinese University of Hong Kong, Hong Kong SAR, China.
Conflict of interest statement
Data availability statement.
There are no new data associated with this article.
- 1. Baer R, Crane C, Miller E et al. Doing no harm in mindfulness-based programs: conceptual issues and empirical findings. Clin Psychol Rev 2019;71:101–14. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Kabat-Zinn J. Mindfulness-based stress reduction (MBSR). Constructivism in the Human Sciences 2003;8:73. [ Google Scholar ]
- 3. Segal ZV, Teasdale JD, Williams JMG. Mindfulness-Based Cognitive Therapy: Theoretical Rationale and Empirical Status. New York: Guilford Press, 2004.
- 4. Teasdale JD, Segal ZV, Williams JMG et al. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol 2000;68:615. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Aghaie E, Roshan R, Mohamadkhani P et al. Well-being, mental health, general health and quality of life improvement through mindfulness-based interventions: a systematic review and meta-analysis. Iran Red Crescent Med J 2018;20:7. doi: 10.5812/ircmj.16231 [ DOI ] [ Google Scholar ]
- 6. Khoury B, Sharma M, Rush SE et al. Mindfulness-based stress reduction for healthy individuals: a meta-analysis. J Psychosom Res 2015;78:519–28. doi: 10.1016/j.jpsychores.2015.03.009 [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Hofmann SG, Sawyer AT, Witt AA et al. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol 2010;78:169–83. doi: 10.1037/a0018555 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 8. Khoury B, Lecomte T, Fortin G et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev 2013;33:763–71. doi: 10.1016/j.cpr.2013.05.005 [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Shi ZR, MacBeth A. The effectiveness of mindfulness-based interventions on maternal perinatal mental health outcomes: a systematic review. Mind 2017;8:823–47. doi: 10.1007/s12671-016-0673-y. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Sevilla-Llewellyn-Jones J, Santesteban-Echarri O, Pryor I et al. Web-based mindfulness interventions for mental health treatment: systematic review and meta-analysis. JMIR Ment Health 2018;5:16. doi: 10.2196/10278. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Blanck P, Perleth S, Heidenreich T et al. Effects of mindfulness exercises as stand-alone intervention on symptoms of anxiety and depression: systematic review and meta-analysis. Behav Res Ther 2018;102:25–35. doi: 10.1016/j.brat.2017.12.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Sanada K, Montero-Marin J, Diez MA et al. Effects of mindfulness-based interventions on salivary cortisol in healthy adults: a meta-analytical review. Front Physiol 2016;7:12. doi: 10.3359/fphys.2016.00/171. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 13. Koncz A, Demetrovics Z, Takacs ZK. Meditation interventions efficiently reduce cortisol levels of at-risk samples: a meta-analysis. Health Psychol Rev 2020:1–29. doi: 10.1080/17437199.2020.1760727. [ DOI ] [ PubMed ]
- 14. Breedvelt JJF, Amanvermez Y, Harrer M et al. The effects of meditation, yoga, and mindfulness on depression, anxiety, and stress in tertiary education students: a meta-analysis. Front Psych 2019;10:15. doi: 10.3389/fpsyt.2019.00193. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Li SYH, Bressington D. The effects of mindfulness-based stress reduction on depression, anxiety, and stress in older adults: a systematic review and meta-analysis. Int J Ment Health Nurs 2019;28:635–56. doi: 10.1111/inm.12568. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Rash JA, Kavanagh VAJ, Garland SN. A meta-analysis of mindfulness-based therapies for insomnia and sleep disturbance moving towards processes of change. Sleep Med Clin 2019;14:209-+. doi: 10.1016/j.jsmc.2019.01.004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Wang YY, Wang F, Zheng W et al. Mindfulness-based interventions for insomnia: a meta-analysis of randomized controlled trials. Behav Sleep Med 2020;18:1–9. doi: 10.1080/15402002.2018.1518228. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Gong H, Ni CX, Liu YZ et al. Mindfulness meditation for insomnia: a meta-analysis of randomized controlled trials. J Psychosom Res 2016;89:1–6. doi: 10.1016/j.jpsychores.2016.07.016 [published online first: September 25, 2016]. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Chen T-L, Chang S-C, Hsieh H-F et al. Effects of mindfulness-based stress reduction on sleep quality and mental health for insomnia patients: a meta-analysis. J Psychosom Res 2020;135:110144. doi: 10.1016/j.jpsychores.2020.110144. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Turgon R, Ruffault A, Juneau C et al. Eating disorder treatment: a systematic review and meta-analysis of the efficacy of mindfulness-based programs. Mind 2019;10:2225–44. doi: 10.1007/s12671-019-01216-5. [ DOI ] [ Google Scholar ]
- 21. Beccia AL, Dunlap C, Hanes DA, et al. Mindfulness-based eating disorder prevention programs: a systematic review and meta-analysis. Mental Health & Prevention 2018;9:1–12 doi: 10.1016/j.mhp.2017.11.001. [ DOI ] [ Google Scholar ]
- 22. Sancho M, De Gracia M, Rodriguez RC et al. Mindfulness-based interventions for the treatment of substance and Behavioral addictions: a systematic review. Front Psych 2018;9:9. doi: 10.3389/fpsyt.2018.00095. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Li W, Howard MO, Garland EL et al. Mindfulness treatment for substance misuse: a systematic review and meta-analysis. J Subst Abus Treat 2017;75:62–96. doi: 10.1016/j.jsat.2017.01.008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Cavicchioli M, Movalli M, Maffei C. The clinical efficacy of mindfulness-based treatments for alcohol and drugs use disorders: a meta-analytic review of randomized and nonrandomized controlled trials. Eur Addict Res 2018;24:137–62. doi: 10.1159/000490762. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Louise S, Fitzpatrick M, Strauss C et al. Mindfulness-and acceptance-based interventions for psychosis: our current understanding and a meta-analysis. Schizophr Res 2018;192:57–63. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Cramer H, Lauche R, Haller H et al. Mindfulness- and acceptance-based interventions for psychosis: a systematic review and meta-analysis. Glob Adv Health Med 2016;5:30–43. doi: 10.7453/gahmj.2015.083 [published online first: March 5, 2016]. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Aust J, Bradshaw T. Mindfulness interventions for psychosis: a systematic review of the literature. J Psychiatr Ment Health Nurs 2017;24:69–83. doi: 10.1111/jpm.12357. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Hilton L, Maher AR, Colaiaco B et al. Meditation for posttraumatic stress: systematic review and meta-analysis. Psychol Trauma 2017;9:453–60. doi: 10.1037/tra0000180. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Niles BL, Mori DL, Polizzi C et al. A systematic review of randomized trials of mind-body interventions for PTSD. J Clin Psychol 2018;74:1485–508. doi: 10.1002/jclp.22634. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Banks K, Newman E, Saleem J. An overview of the research on mindfulness-based interventions for treating symptoms of posttraumatic stress disorder: a systematic review. J Clin Psychol 2015;71:935–63. doi: 10.1002/jclp.22200. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Zhang JH, Diaz-Roman A, Cortese S. Meditation-based therapies for attention-deficit/hyperactivity disorder in children, adolescents and adults: a systematic review and meta-analysis. Evid-Based Ment Health 2018;21:87–94. doi: 10.1136/ebmental-2018-300015. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 32. Mak C, Whittingham K, Cunnington R et al. Efficacy of mindfulness-based interventions for attention and executive function in children and adolescents-a systematic review. Mind 2018;9:59–78. doi: 10.1007/s12671-017-0770-6. [ DOI ] [ Google Scholar ]
- 33. Lee CSC, Ma M-T, Ho H-Y et al. The effectiveness of mindfulness-based intervention in attention on individuals with ADHD: a systematic review. Hong Kong J Occup Ther 2017;30:33–41. doi: 10.1016/j.hkjot.2017.05.001. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 34. Poissant H, Mendrek A, Talbot N et al. Behavioral and cognitive impacts of mindfulness-based interventions on adults with attention-deficit hyperactivity disorder: a systematic review. Behav Neurol 2019;2019:16. doi: 10.1155/2019/5682050. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 35. Hourston S, Atchley R. Autism and mind-body therapies: a systematic review. J Altern Complement Med 2017;23:331–9. doi: 10.1089/acm.2016.0336. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. Cachia RL, Anderson A, Moore DW. Mindfulness in individuals with autism Spectrum disorder: a systematic review and narrative analysis. Rev J Autism Dev Disord 2016;3:165–78. doi: 10.1007/s40489-016-0074-0. [ DOI ] [ Google Scholar ]
- 37. Cachia RL, Anderson A, Moore DW. Mindfulness, stress and well-being in parents of children with autism Spectrum disorder: a systematic review. Journal of Child and Family Studies 2016;25(1):1–14 doi: 10.1007/s10826-015-0193-8. [ DOI ] [ Google Scholar ]
- 38. Hartley M, Dorstyn D, Due C. Mindfulness for children and adults with autism Spectrum disorder and their caregivers: a meta-analysis. J Autism Dev Disord 2019;49:4306–19. doi: 10.1007/s10803-019-04145-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Farhang MA-O, Miranda-Castillo C, Rubio M et al. Impact of mind-body interventions in older adults with mild cognitive impairment: a systematic review. Int Psychogeriatr 2019;31:643–66. doi: 10.1017/S1041610218002302. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Hilton LA-O, Hempel S, Ewing BA et al. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med 2017;51:199–213. doi: 10.1007/s12160-016-9844-2. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Khoo E-L, Small R, Wei C et al. Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: a systematic review and network metaanalysis. Evid Based Ment Health 2019;22:26–35. doi: 10.1136/ebmental-2018-300062. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. McClintock AS, McCarrick SM, Garland EL et al. Brief mindfulness-based interventions for acute and chronic pain: a systematic review. J Altern Complement Med 2019;25:265–78. doi: 10.1089/acm.2018.0351. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Solano Lopez AL. Effectiveness of the mindfulness-based stress reduction program on blood pressure: a systematic review of literature. Worldviews Evid-Based Nurs 2018;15:344–52. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Intarakamhang U, Macaskill A, Prasittichok P. Mindfulness interventions reduce blood pressure in patients with non-communicable diseases: a systematic review and meta-analysis. Heliyon 2020;6:9. doi: 10.1016/j.heliyon.2020.e03834. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 45. Scott-Sheldon LA, Gathright EC, Donahue ML et al. Mindfulness-based interventions for adults with cardiovascular disease: a systematic review and meta-analysis. Ann Behav Med 2020;54:67–73. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 46. Zou LY, Sasaki JE, Zeng N et al. A systematic review with meta-analysis of mindful exercises on rehabilitative outcomes among poststroke patients. Arch Phys Med Rehabil 2018;99:2355–64. doi: 10.1016/j.apmr.2018.04.010. [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Guh DP, Zhang W, Bansback N et al. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 2009;9:88. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48. Lyzwinski LN, Caffery L, Bambling M et al. Relationship between mindfulness, weight, and weight-related behaviors in college students: a systematic review. Alternative & Complementary Therapies 2018;24:202–14. doi: 10.1089/act.2018.29182.lnl. [ DOI ] [ Google Scholar ]
- 49. Carriere K, Khoury B, Gunak MM et al. Mindfulness-based interventions for weight loss: a systematic review and meta-analysis. Obes Rev 2018;19:164–77. doi: 10.1111/obr.12623. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Ruffault A, Czernichow S, Hagger MS et al. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: a systematic review and meta-analysis. Obes Res Clin Pract 2017;11:90–111. doi: 10.1016/j.orcp.2016.09.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Fulwiler C, Brewer JA, Sinnott S, et al. Mindfulness-based interventions for weight loss and CVD risk management. Curr Cardiovasc Risk Rep 2015;9(10):46. doi: 10.1007/s12170-015-0474-1. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 52. Katterman SN, Kleinman BM, Hood MM et al. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eat Behav 2014;15:197–204. doi: 10.1016/j.eatbeh.2014.01.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Artiles RF, Staub K, Aldakak L et al. Mindful eating and common diet programs lower body weight similarly: systematic review and meta-analysis. Obes Rev 2019;20(11):1619–27. doi: 10.1111/obr.12918. [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. Noordali F, Cumming J, Thompson JL. Effectiveness of mindfulness-based interventions on physiological and psychological complications in adults with diabetes: a systematic review. J Health Psychol 2017;22:965–83. doi: 10.1177/1359105315620293. [ DOI ] [ PubMed ] [ Google Scholar ]
- 55. Xia TW, Yang Y, Li WH et al. Meditative movements for patients with type 2 diabetes: a systematic review and meta-analysis. Evid-based Complement Altern Med 2020;2020:12. doi: 10.1155/2020/5745013. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 56. Bogusch LM, O'Brien WH. The effects of mindfulness-based interventions on diabetes-related distress, quality of life, and metabolic control among persons with diabetes: a meta-analytic review. Behav Med 2019;45:19–29. doi: 10.1080/08964289.2018.1432549. [ DOI ] [ PubMed ] [ Google Scholar ]
- 57. Xunlin NG, Lau Y, Klainin-Yobas P et al. The effectiveness of mindfulness-based interventions among cancer patients and survivors: a systematic review and meta-analysis. Support Care Cancer 2020;28:1563–78. doi: 10.1007/s00520-019-05219-9. [ DOI ] [ PubMed ] [ Google Scholar ]
- 58. Ngamkham S, Holden JE, Smith EL. A systematic review: mindfulness intervention for Cancer-related pain. Asia Pac J Oncol Nurs 2019;6:161–9. doi: 10.4103/apjon.apjon_67_18. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 59. He J, Hou JH, Qi J, et al. Mindfulness based stress reduction interventions for cancer related fatigue: a meta-analysis and systematic review. J Natl Med Assoc 2020;112(4):387–94. doi: 10.1016/j.jnma.2020.04.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Xie CY, Dong B, Wang LH et al. Mindfulness-based stress reduction can alleviate cancer-related fatigue: a meta-analysis. J Psychosom Res 2020;130:8. doi: 10.1016/j.jpsychores.2019.109916. [ DOI ] [ PubMed ] [ Google Scholar ]
- 61. Cillessen L, Johannsen M, Speckens AEM et al. Mindfulness-based interventions for psychological and physical health outcomes in cancer patients and survivors: a systematic review and meta-analysis of randomized controlled trials. Psychooncology 2019;28(12):2257–69. doi: 10.1002/pon.5214. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 62. Wu LL, Lin ZK, Weng HD et al. Effectiveness of meditative movement on COPD: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 2018;13:1239–50. doi: 10.2147/COPD.S159042. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 63. Paudyal P, Jones C, Grindey C et al. Meditation for asthma: systematic review and meta-analysis. J Asthma 2018;55:771–8. doi: 10.1080/02770903.2017.1365887. [ DOI ] [ PubMed ] [ Google Scholar ]
- 64. Clari M, Conti A, Fontanella R et al. Mindfulness-based programs for people with chronic obstructive pulmonary disease: a mixed methods systematic review. Mind 2020;20. doi: 10.1007/s12671-020-01348-z. [ DOI ] [ Google Scholar ]
- 65. Donald JN, Sahdra BK, Van Zanden B et al. Does your mindfulness benefit others? A systematic review and meta-analysis of the link between mindfulness and prosocial behaviour. Br J Psychol 2019;110:101–25. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Berry DR, Hoerr JP, Cesko S et al. Does mindfulness training without explicit ethics-based instruction promote prosocial Behaviors? A meta-analysis. Personal Soc Psychol Bull 2020;46:1247–69. [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Wright S, Day A, Howells K. Mindfulness and the treatment of anger problems. Aggression and Violent Behavior 2009;14(5):396–401. doi: 10.1016/j.avb.2009.06.008. [ DOI ] [ Google Scholar ]
- 68. Gillions A, Cheang R, Duarte R. The effect of mindfulness practice on aggression and violence levels in adults: a systematic review. Aggress Violent Behav 2019;48:104–15. doi: 10.1016/j.avb.2019.08.012. [ DOI ] [ Google Scholar ]
- 69. Fix RL, Fix ST. The effects of mindfulness-based treatments for aggression: a critical review. Aggression and Violent Behavior 2013;18(2):219–27. doi: 10.1016/j.avb.2012.11.009. [ DOI ] [ Google Scholar ]
- 70. Friese M, Messner C, Schaffner Y. Mindfulness meditation counteracts self-control depletion. Conscious Cogn 2012;21:1016–22. doi: 10.1016/j.concog.2012.01.008 [published online first: February 09, 2012]. [ DOI ] [ PubMed ] [ Google Scholar ]
- 71. Creswell JD, Irwin MR, Burklund LJ et al. Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain Behav Immun 2012;26(7):1095–101. doi: 10.1016/j.bbi.2012.07.006. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 72. Samhkaniyan E, Mahdavi A, Mohamadpour S, et al. The effectiveness of mindfulness-based cognitive therapy on quality of life and loneliness of women with HIV. J Med Life 2015;8(Spec Iss 4):107–113. [published online first: January 1, 2015] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 73. Zhang N, FM F, Sy H et al. Mindfulness training for loneliness among Chinese college students: a pilot randomized controlled trial. Int J Psychol 2018;53:373–8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 74. Lindsay EK, Young S, Brown KW et al. Mindfulness training reduces loneliness and increases social contact in a randomized controlled trial. Proc Natl Acad Sci U S A 2019;116:3488–93. doi: 10.1073/pnas.1813588116 [published online first: February 28, 2019]. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 75. Burton A, Burgess C, Dean S et al. How effective are mindfulness-based interventions for reducing stress among healthcare professionals? A systematic review and meta-analysis. Stress & Health: J Int Soc for the Investigation of Stress 2017;33:3–13. doi: 10.1002/smi.2673. [ DOI ] [ PubMed ] [ Google Scholar ]
- 76. Lomas T, Medina JC, Ivtzan I et al. A systematic review and meta-analysis of the impact of mindfulness-based interventions on the well-being of healthcare professionals. Mind 2019;10:1193–216. doi: 10.1007/s12671-018-1062-5. [ DOI ] [ Google Scholar ]
- 77. Suleiman-Martos N, Gomez-Urquiza JL, Aguayo-Estremera R et al. The effect of mindfulness training on burnout syndrome in nursing: a systematic review and meta-analysis. J Adv Nursing (John Wiley & Sons, Inc) 2020;76:1124–40. doi: 10.1111/jan.14318. [ DOI ] [ PubMed ] [ Google Scholar ]
- 78. Scheepers RA, Emke H, Epstein RM et al. The impact of mindfulness-based interventions on doctors' well-being and performance: a systematic review. Med Educ 2020;54:138–49. doi: 10.1111/medu.14020. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 79. Bostic JQ, Nevarez MD, Potter MP et al. Being present at school: implementing mindfulness in schools. Child and Adolescent Psychiatric Clinics 2015;24:245–59. [ DOI ] [ PubMed ] [ Google Scholar ]
- 80. Sapthiang S, Van Gordon W, Shonin E. Health school-based mindfulness interventions for improving mental health: a systematic review and thematic synthesis of qualitative studies. Journal of Child and Family Studies 2019;28(10):2650–8. doi: 10.1007/s10826-019-01482-w. [ DOI ] [ Google Scholar ]
- 81. Burgdorf V, Szabo M, Abbott MJ. The effect of mindfulness interventions for parents on parenting stress and youth psychological outcomes: a systematic review and meta-analysis. Front Psychol 2019;10:1336. doi: 10.3389/fpsyg.2019.01336. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 82. Zenner C, Herrnleben-Kurz S, Walach H. Mindfulness-based interventions in schools—a systematic review and meta-analysis. Front Psychol 2014;5:603. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 83. Erbe R, Lohrmann D. Mindfulness meditation for adolescent stress and well-being: a systematic review of the literature with implications for school health programs. Health Educ 2015;47(2):12–9. [ Google Scholar ]
- 84. Durlak JA, Weissberg RP, Dymnicki AB et al. The impact of enhancing students’ social and emotional learning: a meta-analysis of school-based universal interventions. Child Dev 2011;82:405–32. [ DOI ] [ PubMed ] [ Google Scholar ]
- 85. Klingbeil DA, Renshaw TL, Willenbrink JB et al. Mindfulness-based interventions with youth: a comprehensive meta-analysis of group-design studies. J Sch Psychol 2017;63:77–103. [ DOI ] [ PubMed ] [ Google Scholar ]
- 86. Bailey NW, Owen J, Hassed CS, et al. Evidence based guidelines for mindfulness in schools: a guide for teachers and principals. Smiling Mind, 2018. https://static1.squarespace.com/static/5a2f40a41f318d38ccf0c819/t/5b28988170a6ad07781beeb9/1529387171804/smiling-mind-mindfulness-guidelines-for-schools-whitepaper.pdf . (10 August 2020, date last accessed).
- 87. Mesmer-Magnus J, Manapragada A, Viswesvaran C et al. Trait mindfulness at work: a meta-analysis of the personal and professional correlates of trait mindfulness. Hum Perform 2017;30:79–98. doi: 10.1080/08959285.2017.1307842. [ DOI ] [ Google Scholar ]
- 88. Vonderlin R, Biermann M, Bohus M et al. Mindfulness-based programs in the workplace: a meta-analysis of randomized controlled trials. Mind 2020. doi: 10.1007/s12671-020-01328-3. [ DOI ] [ Google Scholar ]
- 89. Cavanagh K, Strauss C, Forder L et al. Can mindfulness and acceptance be learnt by self-help?: a systematic review and meta-analysis of mindfulness and acceptance-based self-help interventions. Clin Psychol Rev 2014;34:118–29. [ DOI ] [ PubMed ] [ Google Scholar ]
- 90. Ergas O. The deeper teachings of mindfulness-based "Interventions' as a reconstruction of "education'. J Philos Educ 2015;49:203–20. doi: 10.1111/1467-9752.12137. [ DOI ] [ Google Scholar ]
- 91. Singh SK, Gorey KM. Relative effectiveness of mindfulness and cognitive behavioral interventions for anxiety disorders: meta-analytic review. Soc Work Ment Health 2018;16:238–51. [ Google Scholar ]
- 92. Doyle SL, Brown JL, Rasheed D et al. Cost analysis of ingredients for successful implementation of a mindfulness-based professional development program for teachers. Mind 2019;10:122–30. [ Google Scholar ]
- 93. Duarte R, Lloyd A, Kotas E et al. Are acceptance and mindfulness-based interventions ‘value for money’? Evidence from a systematic literature review. Br J Clin Psychol 2019;58:187–210. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 94. Johannsen M, Sørensen J, O'Connor M et al. Mindfulness-based cognitive therapy (MBCT) is cost-effective compared to a wait-list control for persistent pain in women treated for primary breast cancer—results from a randomized controlled trial. Psychooncology 2017;26:2208–14. [ DOI ] [ PubMed ] [ Google Scholar ]
- 95. Pérez-Aranda A, D’Amico F, Feliu-Soler A et al. Cost–utility of mindfulness-based stress reduction for fibromyalgia versus a multicomponent intervention and usual care: a 12-month randomized controlled trial (EUDAIMON study). J Clin Med 2019;8:1068. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 96. Herman PM, Anderson ML, Sherman KJ et al. Cost-effectiveness of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care among adults with chronic low-back pain. Spine 2017;42:1511. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 97. Singh NN, Lancioni GE, Karazsia BT et al. Effectiveness of caregiver training in mindfulness-based positive behavior support (MBPBS) vs. training-as-usual (TAU): a randomized controlled trial. Front Psychol 2016;7:1549. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 98. Compen F, Adang E, Bisseling E et al. Cost-utility of individual internet-based and face-to-face mindfulness-based cognitive therapy compared with treatment as usual in reducing psychological distress in cancer patients. Psychooncology 2020;29:294–303. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 99. van Dongen JM, van Berkel J, Boot CR et al. Long-term cost-effectiveness and return-on-investment of a mindfulness-based worksite intervention: results of a randomized controlled trial. J Occup Environ Med 2016;58:550–60. [ DOI ] [ PubMed ] [ Google Scholar ]
- 100. Lymeus F, Lindberg P, Hartig T. A natural meditation setting improves compliance with mindfulness training. J Environ Psychol 2019;64:98–106. doi: 10.1016/j.jenvp.2019.05.008. [ DOI ] [ Google Scholar ]
- 101. Abbott RA, Whear R, Rodgers LR et al. Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: a systematic review and meta-analysis of randomised controlled trials. J Psychosom Res 2014;76:341–51. doi: 10.1016/j.jpsychores.2014.02.012 [published online first: April 22, 2014]. [ DOI ] [ PubMed ] [ Google Scholar ]
- 102. Lamothe M, Rondeau E, Malboeuf-Hurtubise C et al. Outcomes of MBSR or MBSR-based interventions in health care providers: a systematic review with a focus on empathy and emotional competencies. Complement Ther Med 2016;24:19–28. doi: 10.1016/j.ctim.2015.11.001 [published online first: February 11, 2016]. [ DOI ] [ PubMed ] [ Google Scholar ]
- 103. Hill CL, Updegraff JA. Mindfulness and its relationship to emotional regulation. Emotion 2012;12:81–90. doi: 10.1037/a0026355 [published online first: December 14, 2011]. [ DOI ] [ PubMed ] [ Google Scholar ]
- 104. Mikolasek M, Witt CM, Barth J. Adherence to a mindfulness and relaxation self-care app for Cancer patients: mixed-methods feasibility study. JMIR Mhealth Uhealth 2018;6:06. doi: 10.2196/11271. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 105. Vettese LC, Toneatto T, Stea JN, et al. Do mindfulness meditation participants do their homework? And does it make a difference? A review of the empirical evidence. Journal of Cognitive Psychotherapy 2009;23(3):198–225. doi: 10.1891/0889-8391.23.3.198. [ DOI ] [ Google Scholar ]
- 106. Parsons CE, Crane C, Parsons LJ et al. Home practice in mindfulness-based cognitive therapy and mindfulness-based stress reduction: a systematic review and meta-analysis of participants' mindfulness practice and its association with outcomes. Behav Res Ther 2017;95:29–41. doi: 10.1016/j.brat.2017.05.004 [published online first: May 21, 2017]. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 107. Berghoff CR, Wheeless LE, Ritzert TR et al. Mindfulness meditation adherence in a college sample: comparison of a 10-min versus 20-min 2-week daily practice. Mind 2017;8:1513–21. doi: 10.1007/s12671-017-0717-y. [ DOI ] [ Google Scholar ]
- 108. van der Velden AM, Kuyken W, Wattar U et al. A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clin Psychol Rev 2015;37:26–39. [ DOI ] [ PubMed ] [ Google Scholar ]
- 109. Alsubaie M, Abbott R, Dunn B et al. Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: a systematic review. Clin Psychol Rev 2017;55:74–91. [ DOI ] [ PubMed ] [ Google Scholar ]
- 110. Hölzel BK, Lazar SW, Gard T et al. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci 2011;6:537–59. [ DOI ] [ PubMed ] [ Google Scholar ]
- 111. Leyland A, Rowse G, Emerson L-M. Experimental effects of mindfulness inductions on self-regulation: systematic review and meta-analysis. Emotion 2019;19:108. [ DOI ] [ PubMed ] [ Google Scholar ]
- 112. McConnell PA, Froeliger B. Mindfulness, mechanisms and meaning: perspectives from the cognitive neuroscience of addiction. Psychol Inq 2015;26:349–57. doi: 10.1080/1047840X.2015.1076701 [published online first: March 1, 2016]. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 113. Garland EL, Farb NA, Goldin P et al. Mindfulness broadens awareness and builds eudaimonic meaning: a process model of mindful positive emotion regulation. Psychol Inq 2015;26:293–314. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 114. Boccia M, Piccardi L, Guariglia P. The meditative mind: a comprehensive meta-analysis of MRI studies. BioMed Research International 2015;2015:419808 doi: 10.1155/2015/419808. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 115. Vignaud P, Donde C, Sadki T et al. Neural effects of mindfulness-based interventions on patients with major depressive disorder: a systematic review. Neurosci Biobehav Rev 2018;88:98–105. [ DOI ] [ PubMed ] [ Google Scholar ]
- 116. Fox KC, Dixon ML, Nijeboer S et al. Functional neuroanatomy of meditation: a review and meta-analysis of 78 functional neuroimaging investigations. Neurosci Biobehav Rev 2016;65:208–28. [ DOI ] [ PubMed ] [ Google Scholar ]
- 117. Lomas T, Ivtzan I, Fu CHY. A systematic review of the neurophysiology of mindfulness on EEG oscillations. Neurosci Biobehav Rev 2015;57:401–10. doi: 10.1016/j.neubiorev.2015.09.018. [ DOI ] [ PubMed ] [ Google Scholar ]
- 118. Fox KC, Nijeboer S, Dixon ML et al. Is meditation associated with altered brain structure? A systematic review and meta-analysis of morphometric neuroimaging in meditation practitioners. Neurosci Biobehav Rev 2014;43:48–73. [ DOI ] [ PubMed ] [ Google Scholar ]
- 119. Marchand WR. Neural mechanisms of mindfulness and meditation: evidence from neuroimaging studies. World J Radiol 2014;6:471–9. doi: 10.4329/wjr.v6.i7.471. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 120. Black DS, Slavich GM. Mindfulness meditation and the immune system: a systematic review of randomized controlled trials. Ann N Y Acad Sci 2016;1373:13–24. doi: 10.1111/nyas.12998 [published online first: January 23, 2016]. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 121. Pascoe MC, Thompson DR, Jenkins ZM et al. Mindfulness mediates the physiological markers of stress: systematic review and meta-analysis. J Psychiatr Res 2017;95:156–78. [ DOI ] [ PubMed ] [ Google Scholar ]
- 122. Schutte NS, Malouff JM, Keng SL. Meditation and telomere length: a meta-analysis. Psychol Health 2020;1–15. doi: 10.1080/08870446.2019.1707827. [ DOI ] [ PubMed ] [ Google Scholar ]
- 123. Heckenberg RA, Eddy P, Kent S et al. Do workplace-based mindfulness meditation programs improve physiological indices of stress? A systematic review and meta-analysis. J Psychosom Res 2018;114:62–71. [ DOI ] [ PubMed ] [ Google Scholar ]
- 124. Baer R. Ethics, values, virtues, and character strengths in mindfulness-based interventions: a psychological science perspective. Mind 2015;6:956–69. [ Google Scholar ]
- 125. Ruedy NE, Schweitzer ME. In the moment: the effect of mindfulness on ethical decision making. J Bus Ethics 2010;95:73–87. doi: 10.1007/s10551-011-0796-y. [ DOI ] [ Google Scholar ]
- 126. Wong SYS, Chan JYC, Zhang DX et al. The safety of mindfulness-based interventions: a systematic review of randomized controlled trials. Mind 2018;9:1344–57. doi: 10.1007/s12671-018-0897-0. [ DOI ] [ Google Scholar ]
- 127. Anālayo B. The insight knowledge of fear and adverse effects of mindfulness practices. Mind 2019;10:2172–85. [ Google Scholar ]
- 128. Anderson T, Suresh M, Farb NA. Meditation benefits and drawbacks: empirical codebook and implications for teaching. Journal of Cognitive Enhancement 2019;3:207–20. [ Google Scholar ]
- 129. Britton W. Can mindfulness be too much of a good thing? The value of a middle way. Current Opinion in Psychology 2019;28:159–65. doi: 10.1016/j.copsyc.2018.12.011. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 130. Britton WB. Can mindfulness be too much of a good thing? The value of a middle way. Curr Opin Psychol 2019;28:159–65. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 131. Falick M. Mindfulness and the need to minimize the risk of harm: a proposal to implement and enforce standards for secular mindfulness practice. Mindfulness Studies Theses 2020:33. https://digitalcommons.lesley.edu/mindfulness_theses/33 . [ Google Scholar ]
- 132. Schlosser M, Sparby T, Vörös S et al. Unpleasant meditation-related experiences in regular meditators: prevalence, predictors, and conceptual considerations. PLoS ONE 2019;14:e0216643. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 133. Lustyk MK, Chawla N, Nolan R et al. Mindfulness meditation research: issues of participant screening, safety procedures, and researcher training. Adv Mind Body Med 2009;24:20–30. [ PubMed ] [ Google Scholar ]
- 134. Spijkerman M, Pots WTM, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: a review and meta-analysis of randomised controlled trials. Clin Psychol Rev 2016;45:102–14. [ DOI ] [ PubMed ] [ Google Scholar ]
- 135. Toivonen KI, Zernicke K, Carlson LE. Web-based mindfulness interventions for people with physical health conditions: systematic review. J Med Internet Res 2017;19:17. doi: 10.2196/jmir.7487. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 136. Wong SY, Sun YY, Chan AT et al. Treating subthreshold depression in primary care: a randomized controlled trial of behavioral activation with mindfulness. The Annals of Family Medicine 2018;16:111–9. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 137. Zelazo PD, Forston JL, Masten AS et al. Mindfulness plus reflection training: effects on executive function in early childhood. Front Psychol 2018;9:208. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 138. Astin JA, Berman BM, Bausell B et al. The efficacy of mindfulness meditation plus qigong movement therapy in the treatment of fibromyalgia: a randomized controlled trial. J Rheumatol 2003;30:2257–62. [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
- View on publisher site
- PDF (433.4 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 19 April 2021
A systematic review and meta-analysis of psychological interventions to improve mental wellbeing
- Joep van Agteren ORCID: orcid.org/0000-0002-7347-7649 1 , 2 ,
- Matthew Iasiello ORCID: orcid.org/0000-0003-1449-602X 1 , 2 , 3 ,
- Laura Lo 1 ,
- Jonathan Bartholomaeus 1 , 4 , 5 ,
- Zoe Kopsaftis ORCID: orcid.org/0000-0002-9189-1405 6 , 7 , 8 ,
- Marissa Carey 1 &
- Michael Kyrios ORCID: orcid.org/0000-0001-9438-9616 1 , 2 , 9
Nature Human Behaviour volume 5 , pages 631–652 ( 2021 ) Cite this article
22k Accesses
220 Citations
426 Altmetric
Metrics details
- Disease prevention
- Medical humanities
- Outcomes research
- Quality of life
Our current understanding of the efficacy of psychological interventions in improving mental states of wellbeing is incomplete. This study aimed to overcome limitations of previous reviews by examining the efficacy of distinct types of psychological interventions, irrespective of their theoretical underpinning, and the impact of various moderators, in a unified systematic review and meta-analysis. Four-hundred-and-nineteen randomized controlled trials from clinical and non-clinical populations ( n = 53,288) were identified for inclusion. Mindfulness-based and multi-component positive psychological interventions demonstrated the greatest efficacy in both clinical and non-clinical populations. Meta-analyses also found that singular positive psychological interventions, cognitive and behavioural therapy-based, acceptance and commitment therapy-based, and reminiscence interventions were impactful. Effect sizes were moderate at best, but differed according to target population and moderator, most notably intervention intensity. The evidence quality was generally low to moderate. While the evidence requires further advancement, the review provides insight into how psychological interventions can be designed to improve mental wellbeing.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
111,21 € per year
only 9,27 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Systematic review and individual participant data meta-analysis of randomized controlled trials assessing mindfulness-based programs for mental health promotion

A common factors perspective on mindfulness-based interventions
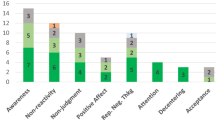
The impact of mindfulness apps on psychological processes of change: a systematic review
Data availability.
The datasets that were used in this review are available from the corresponding author on reasonable request.
Rusk, R. D. & Waters, L. E. Tracing the size, reach, impact, and breadth of positive psychology. J. Posit. Psychol. 8 , 207–221 (2013).
Google Scholar
Diener, E. Subjective wellbeing. Psychological Bull. 95 , 542–575 (1984).
CAS Google Scholar
Ryff, C. D. Happiness is everything, or is it? Explorations on the meaning of psychological wellbeing. J. Pers. Soc. Psychol. 57 , 1069–1081 (1989).
Diener, E., Pressman, S. D., Hunter, J. & Delgadillo‐Chase, D. If, why, and when subjective well‐being influences health, and future needed research. Appl. Psychol. Health Well Being 9 , 133–167 (2017).
PubMed Google Scholar
Keyes, C. L. M., Dhingra, S. S. & Simoes, E. J. Change in level of positive mental health as a predictor of future risk of mental illness. Am. J. Public Health 100 , 2366–2371 (2010).
PubMed PubMed Central Google Scholar
Wood, A. M. & Joseph, S. The absence of positive psychological (eudemonic) wellbeing as a risk factor for depression: a ten year cohort study. J. Affect. Disord. 122 , 213–217 (2010).
Iasello, M., van Agteren, J., Keyes, C. L. M. & Cochrane, E. M. Positive mental health as a predictor of recovery from mental illness. J. Affect. Disord. 251 , 227–230 (2019).
Schotanus-Dijkstra, M., Keyes, C. L. M., de Graaf, R. & ten Have, M. Recovery from mood and anxiety disorders: The influence of positive mental health. J. Affect. Disord. 252 , 107–113 (2019).
Sin, N. L. The protective role of positive wellbeing in cardiovascular disease: review of current evidence, mechanisms, and clinical implications. Curr. Cardiol. Rep. 18 , 106 (2016).
Iasiello, M., van Agteren, J. & Muir-Cochrane, E. Mental health and/or mental illness: a scoping review of the evidence and implications of the dual-continua model of mental health. Evid. Base 2020 , 1–45 (2020).
Keyes, C. L. M. Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am. Psychol. 62 , 95–108 (2007).
Keyes, C. L. M. Mental illness and/or mental health? Investigating axioms of the complete state model of health. J. Consult. Clin. Psychol. 73 , 539–548 (2005).
Slade, M. Mental illness and wellbeing: the central importance of positive psychology and recovery approaches. BMC Health Serv. Res. 10 , 26 (2010).
Hodges, L. J. et al. What is a psychological intervention? A metareview and practical proposal. Psycho‐Oncol. 20 , 470–478 (2011).
Seligman, M. E. P. & Csikszentmihalyi, M. in Flow and the Foundations of Positive Psychology 279–298 (Springer, 2014).
Wood, A. M. & Tarrier, N. Positive clinical psychology: a new vision and strategy for integrated research and practice. Clin. Psychol. Rev. 30 , 819–829 (2010).
Sin, N. L. & Lyubomirsky, S. Enhancing well‐being and alleviating depressive symptoms with positive psychology interventions: a practice‐friendly meta‐analysis. J. Clin. Psychol. 65 , 467–487 (2009).
Weiss, L. A., Westerhof, G. J. & Bohlmeijer, E. T. Can we increase psychological wellbeing? The effects of interventions on psychological wellbeing: A meta-analysis of randomized controlled trials. PLoS ONE 11 , e0158092 (2016).
Chakhssi, F., Kraiss, J. T., Sommers-Spijkerman, M. & Bohlmeijer, E. T. The effect of positive psychology interventions on wellbeing and distress in clinical samples with psychiatric or somatic disorders: a systematic review and meta-analysis. BMC Psychiatry 18 , 211 (2018).
Bolier, L. et al. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health 13 , 119 (2013).
White, C. A., Uttl, B. & Holder, M. D. Meta-analyses of positive psychology interventions: the effects are much smaller than previously reported. PLoS ONE 14 , e0216588 (2019).
CAS PubMed PubMed Central Google Scholar
Gu, J., Strauss, C., Bond, R. & Cavanagh, K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin. Psychol. Rev. 37 , 1–12 (2015).
CAS PubMed Google Scholar
Diener, E. D., Emmons, R. A., Larsen, R. J. & Griffin, S. The satisfaction with life scale. J. Pers. Assess. 49 , 71–75 (1985).
Watson, D., Clark, L. A. & Tellegen, A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J. Pers. Soc. Psychol. 54 , 1063–1070 (1988).
Schueller, S., Kashdan, T. & Parks, A. Synthesizing positive psychological interventions: Suggestions for conducting and interpreting meta-analyses. Int. J. Wellbeing 4 , 91–98 (2014).
Schirrmacher, V. From chemotherapy to biological therapy: a review of novel concepts to reduce the side effects of systemic cancer treatment. Int. J. Oncol. 54 , 407–419 (2019).
Lamers, S. M. A., Bolier, L., Westerhof, G. J., Smit, F. & Bohlmeijer, E. T. The impact of emotional wellbeing on long-term recovery and survival in physical illness: a meta-analysis. J. Behav. Med. 35 , 538–547 (2012).
Hofmann, S. G., Asnaani, A., Vonk, I. J. J., Sawyer, A. T. & Fang, A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cogn. Ther. Res. 36 , 427–440 (2012).
Brown, M., Glendenning, A. C., Hoon, A. E. & John, A. Effectiveness of web-delivered acceptance and commitment therapy in relation to mental health and wellbeing: a systematic review and meta-analysis. J. Med. Internet Res. 18 , e221 (2016).
Dodge, R., Daly, A. P., Huyton, J. & Sanders, L. D. The challenge of defining wellbeing. Int. J. Wellbeing 2 , 222–235 (2012).
Hone, L. C., Jarden, A., Schofield, G. M. & Duncan, S. Measuring flourishing: the impact of operational definitions on the prevalence of high levels of wellbeing. Int. J. Wellbeing 4 , 62–90 (2014).
Higgins, J. P. T. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343 , d5928 (2011).
Guyatt, G. H. et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336 , 924–926 (2008).
Patel, V. et al. The Lancet Commission on global mental health and sustainable development. Lancet 392 , 1553–1598 (2018).
Slade, M. Personal Recovery and Mental Illness: A Guide for Mental Health Professionals (Cambridge Univ. Press, 2009).
Crowe, J. Reform, revolution and disruption in mental health care: a consumer’s perspective. Public Health Res. Pract. 27 , 2721711 (2017).
Mokdad, A. H. et al. The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA 319 , 1444–1472 (2018).
McGorry, P. Prevention, innovation and implementation science in mental health: the next wave of reform. Br. J. Psychiatry 202 , s3–s4 (2013).
Dixon, L. B., Holoshitz, Y. & Nossel, I. Treatment engagement of individuals experiencing mental illness: review and update. World Psychiatry 15 , 13–20 (2016).
Hendriks, T. et al. The efficacy of positive psychological interventions from non-western countries: a systematic review and meta-analysis. Int. J. Wellbeing 8 , 711 (2018).
Hendriks, T., Schotanus-Dijkstra, M., Hassankhan, A., De Jong, J. & Bohlmeijer, E. The efficacy of multi-component positive psychology interventions: a systematic review and meta-analysis of randomized controlled trials. J. Happiness Stud. 21 , 357–390 (2020).
Seligman, M. E. P., Steen, T. A., Park, N. & Peterson, C. Positive psychology progress: empirical validation of interventions. Am. Psychol. 60 , 410–421 (2005).
Lyubomirsky, S. & Layous, K. How do simple positive activities increase wellbeing? Curr. Dir. Psychol. Sci. 22 , 57–62 (2013).
Creswell, J. D. Mindfulness interventions. Annu. Rev. Psychol. 68 , 491–516 (2017).
Padesky, C. A. & Mooney, K. A. Strengths‐based cognitive–behavioural therapy: a four‐step model to build resilience. Clin. Psychol. Psychother. 19 , 283–290 (2012).
David, D., Cristea, I. & Hofmann, S. G. Why cognitive behavioral therapy is the current gold standard of psychotherapy. Front. Psychiatry 9 , 4 (2018).
Stulz, N., Lutz, W., Kopta, S. M., Minami, T. & Saunders, S. M. Dose–effect relationship in routine outpatient psychotherapy: does treatment duration matter?. J. Couns. Psychol. 60 , 593–600 (2013).
Craig, P. et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 337 , a1655 (2008).
Driessen, E., Cuijpers, P., Hollon, S. D. & Dekker, J. J. M. Does pretreatment severity moderate the efficacy of psychological treatment of adult outpatient depression? A meta-analysis. J. Consult. Clin. Psychol. 78 , 668–680 (2010).
Trompetter, H., Lamers, S., Westerhof, G., Fledderus, M. & Bohlmeijer, E. Both positive mental health and psychopathology should be monitored in psychotherapy: confirmation for the dual-factor model in acceptance and commitment therapy. Behav. Res. Ther. 91 , 58–63 (2017).
Van Agteren, J. & Iasiello, M. Advancing our understanding of mental wellbeing and mental health: the call to embrace complexity over simplification. Aust. Psychologist 55 , 307–316 (2020).
Leamy, M., Bird, V., Le Boutillier, C., Williams, J. & Slade, M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br. J. Psychiatry 199 , 445–452 (2011).
Hendriks, T. et al. How WEIRD are positive psychology interventions? A bibliometric analysis of randomized controlled trials on the science of wellbeing. J. Posit. Psychol. 14 , 489–501 (2019).
Chowdhary, N. et al. The methods and outcomes of cultural adaptations of psychological treatments for depressive disorders: a systematic review. Psychol. Med. 44 , 1131–1146 (2014).
Ng, M. Y. & Weisz, J. R. Annual research review: building a science of personalized intervention for youth mental health. J. Child Psychol. Psychiatry 57 , 216–236 (2016).
Wellenzohn, S., Proyer, R. T. & Ruch, W. How do positive psychology interventions work? A short-term placebo-controlled humor-based study on the role of the time focus. Pers. Individ. Differ. 96 , 1–6 (2016).
Rash, J. A., Matsuba, M. K. & Prkachin, K. M. Gratitude and well‐being: who benefits the most from a gratitude intervention? Appl. Psychol. Health Well‐Being 3 , 350–369 (2011).
Parks, A. C. A case for the advancement of the design and study of online positive psychological interventions. J. Posit. Psychol. 9 , 502–508 (2014).
Grant, S. P., Mayo-Wilson, E., Melendez-Torres, G. J. & Montgomery, P. Reporting quality of social and psychological intervention trials: a systematic review of reporting guidelines and trial publications. PLoS ONE 8 , e65442 (2013).
La Placa, V., McNaught, A. & Knight, A. Discourse on wellbeing in research and practice. Int. J. Wellbeing 3 , 116–125 (2013).
Cunningham, J. A., Kypri, K. & McCambridge, J. Exploratory randomized controlled trial evaluating the impact of a waiting list control design. BMC Med. Res. Methodol. 13 , 150 (2013).
Vigo, D., Thornicroft, G. & Atun, R. Estimating the true global burden of mental illness. Lancet Psychiatry 3 , 171–178 (2016).
Slade, M., Oades, L. & Jarden, A. Wellbeing, Recovery and Mental Health (Cambridge Univ. Press, 2017).
Grant, F., Guille, C. & Sen, S. Wellbeing and the risk of depression under stress. PLoS ONE 8 , e67395 (2013).
Maxwell, S. E., Lau, M. Y. & Howard, G. S. Is psychology suffering from a replication crisis? What does ‘failure to replicate’ really mean? Am. Psychologist 70 , 487 (2015).
Proyer, R. T., Wellenzohn, S., Gander, F. & Ruch, W. Toward a better understanding of what makes positive psychology interventions work: predicting happiness and depression from the person × intervention fit in a follow‐up after 3.5 years. Appl. Psychol. Health Well‐Being 7 , 108–128 (2015).
Welton, N. J., Caldwell, D. M., Adamopoulos, E. & Vedhara, K. Mixed treatment comparison meta-analysis of complex interventions: psychological interventions in coronary heart disease. Am. J. Epidemiol. 169 , 1158–1165 (2009).
Kok, G. et al. A taxonomy of behaviour change methods: an intervention mapping approach. Health Psychol. Rev. 10 , 297–312 (2016).
Michie, S. et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 46 , 81–95 (2013).
Michie, S., West, R., Sheals, K. & Godinho, C. A. Evaluating the effectiveness of behavior change techniques in health-related behavior: a scoping review of methods used. Transl. Behav. Med. 8 , 212–224 (2018).
Peters, G.-J. Y., De Bruin, M. & Crutzen, R. Everything should be as simple as possible, but no simpler: towards a protocol for accumulating evidence regarding the active content of health behaviour change interventions. Health Psychol. Rev. 9 , 1–14 (2015).
McHugh, M. L. Interrater reliability: the kappa statistic. Biochemia Med. Biochemia Med. 22 , 276–282 (2012).
Hedges, L. V. Distribution theory for Glass’s estimator of effect size and related estimators. J. Educ. Stat. 6 , 107–128 (1981).
Borenstein, M., Hedges, L., Higgins, J., & Rothstein, H. Comprehensive Meta-Analysis Version 3. https://www.meta-analysis.com/ (Biostat, 2013).
Borenstein, M., Hedges, L. V., Higgins, J. P. T. & Rothstein, H. R. Introduction to Meta-Analysis (Wiley, 2011).
Polanin, J. R. & Pigott, T. D. The use of meta‐analytic statistical significance testing. Res. Synth. Methods 6 , 63–73 (2015).
Valentine, J. C., Pigott, T. D. & Rothstein, H. R. How many studies do you need? A primer on statistical power for meta-analysis. J. Educ. Behav. Stat. 35 , 215–247 (2010).
Disabato, D. J., Goodman, F. R., Kashdan, T. B., Short, J. L. & Jarden, A. Different types of wellbeing? A cross-cultural examination of hedonic and eudaimonic wellbeing. Psychol. Assess. 28 , 471 (2016).
Borenstein, M., Hedges, L. V., Higgins, J. P. T. & Rothstein, H. R. A basic introduction to fixed‐effect and random‐effects models for meta‐analysis. Res. Synth. Methods 1 , 97–111 (2010).
Higgins, J. P. T. & Green, S., eds. Cochrane Handbook for Systematic Reviews of Interventions (Wiley, 2008).
Scammacca, N., Roberts, G. & Stuebing, K. K. Meta-analysis with complex research designs: dealing with dependence from multiple measures and multiple group comparisons. Rev. Educ. Res. 84 , 328–364 (2014).
Tanniou, J., Van Der Tweel, I., Teerenstra, S. & Roes, K. C. B. Subgroup analyses in confirmatory clinical trials: time to be specific about their purposes. BMC Med. Res. Methodol. 16 , 20 (2016).
Ataie Moghanloo, V., Ataie Moghanloo, R. & Moazezi, M. Effectiveness of acceptance and commitment therapy for depression, psychological wellbeing and feeling of Guilt in 7–15 years old diabetic children. Iran. J. Pediatr. 25 , e2436 (2015).
Azkhosh, M., Farhoudianm, A., Saadati, H., Shoaee, F. & Lashani, L. Comparing acceptance and commitment group therapy and 12-steps narcotics anonymous in addict’s rehabilitation process: a randomized controlled trial. Iran. J. Psychiatry 11 , 244–249 (2016).
Fledderus, M., Bohlmeijer, E. T., Smit, F. & Westerhof, G. J. Mental health promotion as a new goal in public mental health care: a randomized controlled trial of an intervention enhancing psychological flexibility. Am. J. Public Health 100 , 2372–2378 (2010).
Fledderus, M., Bohlmeijer, E. T., Pieterse, M. E. & Schreurs, K. M. G. Acceptance and commitment therapy as guided self-help for psychological distress and positive mental health: a randomized controlled trial. Psychol. Med. 42 , 485–495 (2012).
Gregoire, S., Lachance, L., Bouffard, T. & Dionne, F. The use of acceptance and commitment therapy to promote mental health and school engagement in university students: a multisite randomized controlled trial. Behav. Ther. 49 , 360–372 (2018).
Rasanen, P., Lappalainen, P., Muotka, J., Tolvanen, A. & Lappalainen, R. An online guided ACT intervention for enhancing the psychological wellbeing of university students: a randomized controlled clinical trial. Behav. Res. Ther. 78 , 30–42 (2016).
Krafft, J., Potts, S., Schoendorff, B. & Levin, M. E. A Randomized controlled trial of multiple versions of an acceptance and commitment therapy matrix app for wellbeing. Behav. Modif. 43 , 246–272 (2019).
Mani, A. et al. The effectiveness of group acceptance and commitment psychotherapy on psychological wellbeing of breast cancer patients in Shiraz, Iran. Middle East J. Cancer 10 , 231–238 (2019).
Juul, L., Pallesen, K. J., Bjerggaard, M., Nielsen, C. & Fjorback, L. O. A pilot randomised trial comparing a mindfulness-based stress reduction course, a locally-developed stress reduction intervention and a waiting list control group in a real-life municipal health care setting. BMC Public Health 20 , 409 (2020).
McConachie, D. A. J., McKenzie, K., Morris, P. G. & Walley, R. M. Acceptance and mindfulness-based stress management for support staff caring for individuals with intellectual disabilities. Res. Dev. Disabil. 35 , 1216–1227 (2014).
Puolakanaho, A., Tolvanen, A., Kinnunen, S. M. & Lappalainen, R. A psychological flexibility-based intervention for burnout: a randomized controlled trial. J. Contextual Behav. Sci. 15 , 52–67 (2020).
Tol, W. A. et al. Guided self-help to reduce psychological distress in South Sudanese female refugees in Uganda: a cluster randomised trial. Lancet Glob. Health 8 , e254–e263 (2020).
Trompetter, H. R., Bohlmeijer, E. T., Lamers, S. & Schreurs, K. M. Positive psychological wellbeing is required for online self-help acceptance and commitment therapy for chronic pain to be effective. Front. Psychol. 7 , 353 (2014).
Viskovich, S. & Pakenham, K. I. Randomized controlled trial of a web‐based acceptance and commitment therapy (ACT) program to promote mental health in university students. J. Clin. Psychol. 76 , 929–951 (2020).
Wicksell, R. K., Ahlqvist, J., Bring, A., Melin, L. & Olsson, G. L. Can exposure and acceptance strategies improve functioning and life satisfaction in people with chronic pain and whiplash-associated disorders (WAD)? A randomized controlled trial. Cogn. Behav. Ther. 37 , 169–182 (2008).
Hofer, P. D. et al. Self-help for stress and burnout without therapist contact: an online randomised controlled trial. Work Stress 32 , 189–208 (2018).
Johnston, M., Foster, M., Shennan, J., Starkey, N. J. & Johnson, A. The effectiveness of an acceptance and commitment therapy self-help intervention for chronic pain. Clin. J. Pain. 26 , 393–402 (2010).
Majumdar, S. & Morris, R. Brief group‐based acceptance and commitment therapy for stroke survivors. Br. J. Clin. Psychol. 58 , 70–90 (2019).
Sewart, A. R. et al. Examining positive and negative affect as outcomes and moderators of cognitive-behavioral therapy and acceptance and commitment therapy for social anxiety disorder. Behav. Ther. 50 , 1112–1124 (2019).
Jazaieri, H. et al. A randomized controlled trial of compassion cultivation training: Effects on mindfulness, affect, and emotion regulation. Motiv. Emot. 38 , 23–35 (2014).
Mongrain, M., Chin, J. M. & Shapira, L. B. Practicing compassion increases happiness and self-esteem. J. Happiness Stud. 12 , 963–981 (2011).
Shapira, L. B. & Mongrain, M. The benefits of self-compassion and optimism exercises for individuals vulnerable to depression. J. Posit. Psychol. 5 , 377–389 (2010).
Smeets, E., Neff, K., Alberts, H. & Peters, M. Meeting suffering with kindness: effects of a brief self-compassion intervention for female college students. J. Clin. Psychol. 70 , 794–807 (2014).
Neff, K. D. & Germer, C. K. A pilot study and randomized controlled trial of the mindful self-compassion program. J. Clin. Psychol. 69 , 28–44 (2013).
Krieger, T. et al. An internet-based compassion-focused intervention for increased self-criticism: a randomized controlled trial. Behav. Ther. 50 , 430–445 (2019).
Ziemer, K. S., Lamphere, B. R., Raque-Bogdan, T. L. & Schmidt, C. K. A randomized controlled study of writing interventions on college women’s positive body image. Mindfulness 10 , 66–77 (2019).
Alireza Afshani, S., Abooei, A. & Mohamad Abdoli, A. Self-compassion training and psychological wellbeing of infertile female. Int. J. Reprod. Biomedicine 17 , 757–762 (2019).
Gammer, I., Hartley-Jones, C. & Jones, F. W. A randomized controlled trial of an online, compassion-based intervention for maternal psychological wellbeing in the first year postpartum. Mindfulness 11 , 928–939 (2020).
Sommers-Spijkerman, M., Trompetter, H., Schreurs, K. & Bohlmeijer, E. Compassion-focused therapy as guided self-help for enhancing public mental health: a randomized controlled trial. J. Consult. Clin. Psychol. 86 , 101–115 (2018).
Wong, C. C. & Mak, W. W. Writing can heal: effects of self-compassion writing among Hong Kong Chinese college students. Asian Am. J. Psychol. 7 , 74–82 (2016).
Barnes, C. & Mongrain, M. A three-factor model of personality predicts changes in depression and subjective wellbeing following positive psychology interventions. J. Posit. Psychol. 15 , 556–568 (2020).
Abbott, J.-A., Klein, B., Hamilton, C. & Rosenthal, A. The impact of online resilience training for sales managers on wellbeing and performance. E-J. Appl. Psychol. 5 , 89–95 (2009).
Beukes, E. W., Baguley, D. M., Allen, P. M., Manchaiah, V. & Andersson, G. Audiologist-guided internet-based cognitive behavior therapy for adults with tinnitus in the United Kingdom: a randomized controlled trial. Ear Hearing 39 , 423–433 (2018).
Green, L., Oades, L. & Grant, A. Cognitive-behavioral, solution-focused life coaching: enhancing goal striving, wellbeing, and hope. J. Posit. Psychol. 1 , 142–149 (2006).
Arango-Lasprilla, J. C. et al. Evaluation of a group cognitive-behavioral dementia caregiver intervention in Latin America. Am. J. Alzheimers Dis. Other Dement. 29 , 548–555 (2014).
Rose, K., Hawes, D. J. & Hunt, C. J. Randomized controlled trial of a friendship skills intervention on adolescent depressive symptoms. J. Consult. Clin. Psychol. 82 , 510–520 (2014).
Chambers, S. K., Ferguson, M., Gardiner, R. A., Aitken, J. & Occhipinti, S. Intervening to improve psychological outcomes for men with prostate cancer. Psychooncology 22 , 1025–1034 (2013).
Cho, H., Ryu, S., Noh, J. & Lee, J. The effectiveness of daily mindful breathing practices on test anxiety of students. PLoS ONE 11 , e0164822 (2016).
Diab, M., Peltonen, K., Qouta, S. R., Palosaari, E. & Punamaki, R.-L. Effectiveness of psychosocial intervention enhancing resilience among war-affected children and the moderating role of family factors. Child Abus. Negl. 40 , 24–35 (2015).
Eimontas, J. et al. The role of therapist support on effectiveness of an internet-based modular self-help intervention for adjustment disorder: a randomized controlled trial. Anxiety Stress Coping 31 , 146–158 (2018).
Garland, E. L., Roberts-Lewis, A., Tronnier, C. D., Graves, R. & Kelley, K. Mindfulness-oriented recovery enhancement versus CBT for co-occurring substance dependence, traumatic stress, and psychiatric disorders: proximal outcomes from a pragmatic randomized trial. Behav. Res. Ther. 77 , 7–16 (2016).
Hoifodt, R. S. et al. The clinical effectiveness of web-based cognitive behavioral therapy with face-to-face therapist support for depressed primary care patients: randomized controlled trial. J. Med. Internet Res. 15 , e153 (2013).
Hyer, L., Yeager, C. A., Hilton, N. & Sacks, A. Group, individual, and staff therapy: an efficient and effective cognitive behavioral therapy in long-term care. Am. J. Alzheimers Dis. Other Dement. 23 , 528–539 (2008).
Lumley, M. A. et al. Emotional awareness and expression therapy, cognitive behavioral therapy, and education for fibromyalgia: a cluster-randomized controlled trial. Pain 158 , 2354–2363 (2017).
Oei, T. P. S., Raylu, N. & Lai, W. W. Effectiveness of a self help cognitive behavioural treatment program for problem gamblers: a randomised controlled trial. J. Gambl. Stud. 34 , 581–595 (2018).
Rezvan, S., Baghban, I., Bahrami, F. & Abedi, M. A comparison of cognitive-behavior therapy with interpersonal and cognitive behavior therapy in the treatment of generalized anxiety disorder. Counselling Psychol. Q. 21 , 309–321 (2008).
Ruppert, J. C. & Eiroa-Orosa, F. J. Positive visual reframing: A randomised controlled trial using drawn visual imagery to defuse the intensity of negative experiences and regulate emotions in healthy adults. An. de Psicol. 34 , 368–377 (2018).
Strachowski, D. et al. The effects of cognitive behavior therapy on depression in older patients with cardiovascular risk. Depress. Anxiety 25 , E1–E10 (2008).
Tak, Y. R., Kleinjan, M., Lichtwarck-Aschoff, A. & Engels, R. C. M. E. Secondary outcomes of a school-based universal resiliency training for adolescents: a cluster randomized controlled trial. BMC Public Health 14 , 1171 (2014).
Walker, J. V. III & Lampropoulos, G. K. A comparison of self-help (homework) activities for mood enhancement: results from a brief randomized controlled trial. J. Psychother. Integr. 24 , 46–64 (2014).
Zautra, A. J. et al. Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. J. Consult. Clin. Psychol. 76 , 408–421 (2008).
Zhang, B. et al. Effect of group cognitive-behavioral therapy on the quality of life and social functioning of patients with mild depression. Shanghai Arch. Psychiatry 28 , 18–27 (2016).
Garland, E. L., Hanley, A. W., Goldin, P. R. & Gross, J. J. Testing the mindfulness-to-meaning theory: evidence for mindful positive emotion regulation from a reanalysis of longitudinal data. PLoS ONE 12 , e0187727 (2017).
Spence, G. B. & Grant, A. M. Professional and peer life coaching and the enhancement of goal striving and wellbeing: an exploratory study. J. Posit. Psychol. 2 , 185–194 (2007).
Smith, G. C., Strieder, F., Greenberg, P., Hayslip, B. Jr. & Montoro-Rodriguez, J. Patterns of enrollment and engagement of custodial grandmothers in a randomized clinical trial of psychoeducational interventions. Fam. Relat. 65 , 369–386 (2016).
Brodbeck, J., Berger, T., Biesold, N., Rockstroh, F. & Znoj, H. J. Evaluation of a guided internet-based self-help intervention for older adults after spousal bereavement or separation/divorce: a randomised controlled trial. J. Affect. Disord. 252 , 440–449 (2019).
Wilner Tirpak, J. et al. Changes in positive affect in cognitive-behavioral treatment of anxiety disorders. Gen. Hosp. Psychiatry 61 , 111–115 (2019).
García-Escalera, J., Valiente, R. M., Sandín, B., Ehrenreich-May, J. & Chorot, P. Educational and wellbeing outcomes of an anxiety and depression prevention program for adolescents. Rev. de. Psicodidactica https://doi.org/10.1016/j.psicod.2020.05.001 (2020).
Article Google Scholar
Knapstad, M., Lervik, L. V., Saether, S. M. M., Aaro, L. E. & Smith, O. R. F. Effectiveness of prompt mental health care, the norwegian version of improving access to psychological therapies: a randomized controlled trial. Psychother. Psychosom. 89 , 90–105 (2020).
Loucas, C. E., Sclare, I., Stahl, D. & Michelson, D. Feasibility randomized controlled trial of a one-day CBT workshop (‘DISCOVER’) for 15- to 18-year-olds with anxiety and/or depression in clinic settings. Behav. Cogn. Psychother. 48 , 142–159 (2020).
Punamäki, R.-L., Peltonen, K., Diab, M. & Qouta, S. R. Psychosocial interventions and emotion regulation among war-affected children: randomized control trial effects. Traumatology 20 , 241 (2014).
Lichter, S., Haye, K. & Kammann, R. Increasing happiness through cognitive retraining. NZ J. Psychol. 9 , 57–64 (1980).
Peters, M. L. et al. Happy despite pain: a randomized controlled trial of an 8-week internet-delivered positive psychology intervention for enhancing wellbeing in patients with chronic pain. Clin. J. Pain. 33 , 962–975 (2017).
Tovote, K. A. et al. Individual mindfulness-based cognitive therapy and cognitive behavior therapy for treating depressive symptoms in patients with diabetes: results of a randomized controlled trial. Diabetes Care 37 , 2427–2434 (2014).
Casey, L. M. et al. Internet-based delivery of cognitive behaviour therapy compared to monitoring, feedback and support for problem gambling: a randomised controlled trial. J. Gambl. Stud. 33 , 993–1010 (2017).
Freeman, D. et al. An early Phase II randomised controlled trial testing the effect on persecutory delusions of using CBT to reduce negative cognitions about the self: the potential benefits of enhancing self confidence. Schizophrenia Res. 160 , 186–192 (2014).
Graziano, F., Calandri, E., Borghi, M. & Bonino, S. The effects of a group-based cognitive behavioral therapy on people with multiple sclerosis: a randomized controlled trial. Clin. Rehabil. 28 , 264–274 (2014).
Hazell, C. M., Hayward, M., Cavanagh, K., Jones, A.-M. & Strauss, C. Guided self-help cognitive-behaviour Intervention for VoicEs (GiVE): Results from a pilot randomised controlled trial in a transdiagnostic sample. Schizophrenia Res. 195 , 441–447 (2018).
Hermanns, N. et al. The effect of a diabetes-specific cognitive behavioral treatment program (diamos) for patients with diabetes and subclinical depression: results of a randomized controlled trial. Diabetes Care 38 , 551–560 (2015).
Jensen, S. E. et al. Cognitive-behavioral stress management and psychological weil-being in HIV+ racial/ethnic minority women with human papillomavirus. Health Psychol. 32 , 227–230 (2013).
Lokman, S. et al. Complaint-directed mini-interventions for depressive complaints: a randomized controlled trial of unguided web-based self-help interventions. J. Med. Internet Res. 19 , e4 (2017).
Lu, Q. & Stanton, A. L. How benefits of expressive writing vary as a function of writing instructions, ethnicity and ambivalence over emotional expression. Psychol. Health 25 , 669–684 (2010).
Nahlen Bose, C. et al. Evaluation of a coping effectiveness training intervention in patients with chronic heart failure - a randomized controlled trial. Eur. J. Cardiovascular Nurs. 15 , 537–548 (2016).
Parks, A. C. & Szanto, R. K. Assessing the efficacy and effectiveness of a positive psychology-based self-help book. Posit. Psychol. 31 , 141–149 (2013).
Powell, J. et al. Effectiveness of a web-based cognitive-behavioral tool to improve mental wellbeing in the general population: randomized controlled trial. J. Med. Internet Res. 15 , 3–19 (2013).
Seligman, M. E. P., Schulman, P. & Tryon, A. M. Group prevention of depression and anxiety symptoms. Behav. Res. Ther. 45 , 1111–1126 (2007).
Terides, M. D. et al. Increased skills usage statistically mediates symptom reduction in self-guided internet-delivered cognitive–behavioural therapy for depression and anxiety: a randomised controlled trial. Cogn. Behav. Ther. 47 , 43–61 (2018).
Nwobi, U. A. et al. A stress management intervention for adults living with HIV in Nigerian community settings: an effects study. Medicine 97 , e12801 (2018).
Eimontas, J., Rimsaite, Z., Gegieckaite, G., Zelviene, P. & Kazlauskas, E. Internet-based self-help intervention for ICD-11 adjustment disorder: preliminary findings. Psychiatr. Q. 89 , 451–460 (2018).
Peters, E. et al. A randomised controlled trial of cognitive behaviour therapy for psychosis in a routine clinical service. Acta Psychiatr. Scandinavica 122 , 302–318 (2010).
Barclay, L. J. & Skarlicki, D. P. Healing the wounds of organizational injustice: examining the benefits of expressive writing. J. Appl. Psychol. 94 , 511–523 (2009).
Tavakoli, S., Lumley, M. A., Hijazi, A. M., Slavin-Spenny, O. M. & Parris, G. P. Effects of assertiveness training and expressive writing on acculturative stress in international students: a randomized trial. J. Couns. Psychol. 56 , 590–596 (2009).
Troop, N. A., Chilcot, J., Hutchings, L. & Varnaite, G. Expressive writing, self-criticism, and self-reassurance. Psychol. Psychother. 86 , 374–386 (2013).
Wing, J. F., Schutte, N. S. & Byrne, B. The effect of positive writing on emotional intelligence and life satisfaction. J. Clin. Psychol. 62 , 1291–1302 (2006).
Francis, M. E. & Pennebaker, J. W. Putting stress into words: the impact of writing on physiological, absentee, and self-reported emotional wellbeing measures. Am. J. Health Promot. 6 , 280–287 (1992).
Koenig Kellas, J., Horstman, H. K., Willer, E. K. & Carr, K. The benefits and risks of telling and listening to stories of difficulty over time: experimentally testing the expressive writing paradigm in the context of interpersonal communication between friends. Health Commun. 30 , 843–858 (2015).
Lamers, S. M. A., Bohlmeijer, E. T., Korte, J. & Westerhof, G. J. The efficacy of life-review as online-guided self-help for adults: a randomized trial. J. Gerontol. B 70 , 24–34 (2015).
Baker, F. A. et al. A therapeutic songwriting intervention to promote reconstruction of self-concept and enhance wellbeing following brain or spinal cord injury: pilot randomized controlled trial. Clin. Rehabil. 33 , 1045–1055 (2019).
Miao, M. & Gan, Y. How does meaning in life predict proactive coping? The self-regulatory mechanism on emotion and cognition. J. Pers. 87 , 579–592 (2019).
Lyubomirsky, S., Sousa, L. & Dickerhoof, R. The costs and benefits of writing, talking, and thinking about life’s triumphs and defeats. J. Pers. Soc. Psychol. 90 , 692 (2006).
Rubin, M., Hawkins, B., Cobb, A. & Telch, M. J. Emotional reactivity to grief-related expressive writing. Death Stud. 44 , 552–560 (2020).
Fernandez, I. & Paez, D. The benefits of expressive writing after the Madrid terrorist attack: implications for emotional activation and positive affect. Br. J. Health Psychol. 13 , 31–34 (2008).
Rivkin, I. D. & Taylor, S. E. The effects of mental simulation on coping with controllable stressful events. Pers. Soc. Psychol. Bull. 25 , 1451–1462 (1999).
Bhayee, S. et al. Attentional and affective consequences of technology supported mindfulness training: a randomised, active control, efficacy trial. BMC Psychol. 4 , 60 (2016).
Bower, J. E. et al. Mindfulness meditation for younger breast cancer survivors: a randomized controlled trial. Cancer 121 , 1231–1240 (2015).
Cole, B. S. et al. A randomised clinical trial of the effects of spiritually focused meditation for people with metastatic melanoma. Ment. Health Relig. Cult. 15 , 161–174 (2012).
Dvořáková, K. et al. Promoting healthy transition to college through mindfulness training with first-year college students: pilot randomized controlled trial. J. Am. Coll. Health 65 , 259–267 (2017).
Galante, J. et al. A mindfulness-based intervention to increase resilience to stress in university students (the Mindful Student Study): a pragmatic randomised controlled trial. Lancet Public Health 3 , e72–e81 (2018).
Gambrel, L. E. & Piercy, F. P. Mindfulness-based relationship education for couples expecting their first child–part 1: a randomized mixed-methods program evaluation. J. Marital Fam. Ther. 41 , 5–24 (2015).
Glück, T. M. & Maercker, A. A randomized controlled pilot study of a brief web-based mindfulness training. BMC Psychiatry 11 , 175 (2011).
Howells, A., Ivtzan, I. & Eiroa-Orosa, F. J. Putting the ‘app’ in happiness: a randomised controlled trial of a smartphone-based mindfulness intervention to enhance wellbeing. J. Happiness Stud. 17 , 163–185 (2016).
Hwang, K., Kwon, A. & Hong, C. A preliminary study of new positive psychology interventions: neurofeedback-aided meditation therapy and modified positive psychotherapy. Curr. Psychol. 36 , 683–695 (2017).
Ivtzan, I. et al. Integrating mindfulness into positive psychology: a randomised controlled trial of an online positive mindfulness program. Mindfulness 7 , 1396–1407 (2016).
Johnson, C., Burke, C., Brinkman, S. & Wade, T. Effectiveness of a school-based mindfulness program for transdiagnostic prevention in young adolescents. Behav. Res. Ther. 81 , 1–11 (2016).
Mi Ra, Y., Misoon, S., Kyung-Hae, J., Yu, B. J. & Kyung Jae, L. The effects of mind subtraction meditation on breast cancer survivors’ psychological and spiritual wellbeing and sleep quality: a randomized controlled trial in South Korea. Cancer Nurs. 40 , 377–385 (2017).
Mongrain, M., Komeylian, Z. & Barnhart, R. Happiness vs. mindfulness exercises for individuals vulnerable to depression. J. Posit. Psychol. 11 , 366–377 (2016).
Nakamura, S. et al. Effect of management training in organizational justice: a randomized controlled trial. Ind. Health 54 , 263–271 (2016).
Oken, B. S. et al. Meditation in stressed older adults: improvements in self-rated mental health not paralleled by improvements in cognitive function or physiological measures. Mindfulness 8 , 627–638 (2017).
Perez-Blasco, J., Sales, A., Meléndez, J. C. & Mayordomo, T. The effects of mindfulness and self-compassion on improving the capacity to adapt to stress situations in elderly people living in the community. Clin. Gerontologist 39 , 90–103 (2016).
Pinniger, R., Brown, R. F., Thorsteinsson, E. B. & McKinley, P. Argentine tango dance compared to mindfulness meditation and a waiting-list control: a randomised trial for treating depression. Complement. Ther. Med. 20 , 377–384 (2012).
Spek, A. A., van Ham, N. C. & Nyklicek, I. Mindfulness-based therapy in adults with an autism spectrum disorder: a randomized controlled trial. Res. Dev. Disabil. 34 , 246–253 (2013).
Vieten, C. & Astin, J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Arch. Womens Ment. Health 11 , 67–74 (2008).
Waelde, L. C., Meyer, H., Thompson, J. M., Thompson, L. & Gallagher-Thompson, D. Randomized controlled trial of inner resources meditation for family dementia caregivers. J. Clin. Psychol. 73 , 1629–1641 (2017).
Cousin, G. & Crane, C. Changes in disengagement coping mediate changes in affect following mindfulness-based cognitive therapy in a non-clinical sample. Br. J. Psychol. 107 , 434–447 (2016).
Dowd, H. et al. Comparison of an online mindfulness-based cognitive therapy intervention with online pain management psychoeducation: a randomized controlled study. Clin. J. Pain. 31 , 517–527 (2015).
Huffman, J. C. et al. Development of a positive psychology intervention for patients with acute cardiovascular disease. Heart Int. 6 , e14 (2011).
Johannsen, M. et al. Efficacy of mindfulness-based cognitive therapy on late post-treatment pain in women treated for primary breast cancer: a randomized controlled trial. J. Clin. Oncol. 34 , 3390–3399 (2016).
Lee, W. K. & Bang, H. J. The effects of mindfulness‐based group intervention on the mental health of middle‐aged Korean women in community. Stress Health 26 , 341–348 (2010).
Lever Taylor, B., Strauss, C., Cavanagh, K. & Jones, F. The effectiveness of self-help mindfulness-based cognitive therapy in a student sample: a randomised controlled trial. Behav. Res. Ther. 63 , 63–69 (2014).
Pots, W. T., Meulenbeek, P. A., Veehof, M. M., Klungers, J. & Bohlmeijer, E. T. The efficacy of mindfulness-based cognitive therapy as a public mental health intervention for adults with mild to moderate depressive symptomatology: a randomized controlled trial. PLoS ONE 9 , e109789 (2014).
de Vibe, M. et al. Mindfulness training for stress management: a randomised controlled study of medical and psychology students. BMC Med. Educ. 13 , 107 (2013).
Gallegos, A. M., Hoerger, M., Talbot, N. L., Moynihan, J. A. & Duberstein, P. R. Emotional benefits of mindfulness-based stress reduction in older adults: the moderating roles of age and depressive symptom severity. Aging Ment. Health 17 , 823–829 (2013).
Gayner, B. et al. A randomized controlled trial of mindfulness-based stress reduction to manage affective symptoms and improve quality of life in gay men living with HIV. J. Behav. Med. 35 , 272–285 (2012).
Henriksson, J., Wasara, E. & Ronnlund, M. Effects of eight-week-web-based mindfulness training on pain intensity, pain acceptance, and life satisfaction in individuals with chronic pain. Psychol. Rep. 119 , 586–607 (2016).
Jansen, P., Dahmen-Zimmer, K., Kudielka, B. M. & Schulz, A. Effects of karate training versus mindfulness training on Emotional wellbeing and cognitive performance in later Life. Res. Aging 39 , 1118–1144 (2017).
Mackenzie, C. S., Poulin, P. A. & Seidman-Carlson, R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Appl. Nurs. Res. 19 , 105–109 (2006).
Neece, C. L. Mindfulness-based stress reduction for parents of young children with developmental delays: implications for parental mental health and child behavior problems. J. Appl. Res. Intellect. Disabil. 27 , 174–186 (2014).
Nyklicek, I. & Kuijpers, K. F. Effects of mindfulness-based stress reduction intervention on psychological wellbeing and quality of life: is increased mindfulness indeed the mechanism? Ann. Behav. Med. 35 , 331–340 (2008).
Pradhan, E. K. et al. Effect of mindfulness-based stress reduction in rheumatoid arthritis patients. Arthritis Rheum. 57 , 1134–1142 (2007).
van Dijk, I. et al. Effects of mindfulness-based stress reduction on the mental health of clinical clerkship students: a cluster-randomized controlled trial. Academic Med. 92 , 1012–1021 (2017).
Zolnierczyk-Zreda, D., Sanderson, M. & Bedynska, S. Mindfulness-based stress reduction for managers: a randomized controlled study. Occup. Med. 66 , 630–635 (2016).
Dambrun, M. When the dissolution of perceived body boundaries elicits happiness: the effect of selflessness induced by a body scan meditation. Conscious. Cogn. 46 , 89–98 (2016).
Peters, R. K., Benson, H. & Porter, D. Daily relaxation response breaks in a working population: I. Effects on self-reported measures of health, performance, and wellbeing. Am. J. Public Health 67 , 946–953 (1977).
Reig-Ferrer, A. et al. A relaxation technique enhances psychological wellbeing and immune parameters in elderly people from a nursing home: a randomized controlled study. BMC Complement. Altern. Med. 14 , 311 (2014).
Roche, L. T., Barrachina, M. T. M., Fernández, I. I. & Betancort, M. YOGA and self-regulation in management of essential arterial hypertension and associated emotional symptomatology: a randomized controlled trial. Complementary Ther. Clin. Pract. 29 , 153–161 (2017).
Fredrickson, B. L., Cohn, M. A., Coffey, K. A., Pek, J. & Finkel, S. M. Open hearts build lives: positive emotions, induced through loving-kindness meditation, build consequential personal resources. J. Pers. Soc. Psychol. 95 , 1045–1062 (2008).
Hecht, F. M. et al. A randomized, controlled trial of mindfulness-based stress reduction in HIV infection. Brain Behav. Immun. 73 , 331–339 (2018).
Innes, K. E., Selfe, T. K., Khalsa, D. S. & Kandati, S. Effects of meditation versus music listening on perceived stress, mood, sleep, and quality of life in adults with early memory loss: a pilot randomized controlled trial. J. Alzheimers Dis. 52 , 1277–1298 (2016).
Kögler, M. et al. Mindfulness in informal caregivers of palliative patients. Palliat. Support. Care 13 , 11–18 (2015).
Zilcha-Mano, S. & Langer, E. Mindful attention to variability intervention and successful pregnancy outcomes. J. Clin. Psychol. 72 , 897–907 (2016).
Shapiro, S. L., Astin, J. A., Bishop, S. R. & Cordova, M. Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int. J. Stress Manag. 12 , 164 (2005).
Bostock, S., Crosswell, A. D., Prather, A. A. & Steptoe, A. Mindfulness on-the-go: effects of a mindfulness meditation app on work stress and wellbeing. J. Occup. Health Psychol. 24 , 127–138 (2019).
Flett, J. A. M., Hayne, H., Riordan, B. C., Thompson, L. M. & Conner, T. S. Mobile mindfulness meditation: a randomised controlled trial of the effect of two popular apps on mental health. Mindfulness 10 , 863–876 (2019).
Ivtzan, I. et al. Mindfulness based flourishing program: a cross-cultural study of Hong Kong Chinese and British participants. J. Happiness Stud. 19 , 2205–2223 (2018).
Jarukasemthawee, S., Halford, W. K. & McLean, J. P. When East meets West: a randomized controlled trial and pre- to postprogram evaluation replication of the effects of insight-based mindfulness on psychological wellbeing. J. Psychother. Integr. 29 , 307–323 (2019).
Lin, L., He, G., Yan, J., Gu, C. & Xie, J. The effects of a modified mindfulness-based stress reduction program for nurses: A randomized controlled trial. Workplace Health Saf. 67 , 111–122 (2019).
Zemestani, M. & Fazeli Nikoo, Z. Effectiveness of mindfulness-based cognitive therapy for comorbid depression and anxiety in pregnancy: a randomized controlled trial. Arch. Womens Ment. Health 23 , 207–214 (2020).
Zeng, X., Wang, R., Oei, T. P. S. & Leung, F. Y. K. Heart of joy: a randomized controlled trail evaluating the effect of an appreciative joy meditation training on subjective wellbeing and attitudes. Mindfulness 10 , 506–515 (2019).
Ahmad, F. et al. An eight-week, web-based mindfulness virtual community intervention for students’ mental health: randomized controlled trial. JMIR Ment. Health 7 , e15520 (2020).
Bostani, S., Rambod, M., Irani, P. S. & Torabizadeh, C. Comparing the effect of progressive muscle relaxation exercise and support group therapy on the happiness of nursing students: a randomized clinical trial study. Int. J. Afr. Nurs. Sci. 13 , 100218 (2020).
Cejudo, J. et al. Using a mindfulness-based intervention to promote subjective wellbeing, trait emotional intelligence, mental health, and resilience in women with fibromyalgia. Front. Psychol. 10 , 2541 (2019).
Cerna, C., Garcia, F. E. & Tellez, A. Brief mindfulness, mental health, and cognitive processes: a randomized controlled trial. Psych. J. 9 , 359–369 (2020).
Donald, G. et al. Positively mindful: a mixed method feasibility study of mindfulness meditation for people living with HIV in the UK. Eur. J. Integr. Med. 37 , 101088 (2020).
Hirshberg, M. J., Flook, L., Enright, R. D. & Davidson, R. J. Integrating mindfulness and connection practices into preservice teacher education improves classroom practices. Learn. Instr. 66 , 101298 (2020).
Lo, H. H. M. et al. The effects of family-based mindfulness intervention on adhd symptomology in young children and their parents: a randomized control trial. J. Atten. Disord. 24 , 667–680 (2020).
Macdougall, H., O’Halloran, P., Sherry, E. & Shields, N. A pilot randomised controlled trial to enhance wellbeing and performance of athletes in para sports. Eur. J. Adapted Phys. Act. 12 , 7 (2019).
Mistretta, E. G. et al. Resilience training for work-related stress among health care workers: results of a randomized clinical trial comparing in-person and smartphone-delivered interventions. J. Occup. Environ. Med. 60 , 559–568 (2018).
Nadler, R., Carswell, J. J. & Minda, J. P. Online mindfulness training increases wellbeing, trait emotional intelligence, and workplace competency ratings: a randomized waitlist-controlled trial. Front. Psychol. 11 , 255 (2020).
Weytens, F., Luminet, O., Verhofstadt, L. L. & Mikolajczak, M. An integrative theory-driven positive emotion regulation intervention. PLoS ONE 9 , e95677 (2014).
Zarifsanaiey, N., Jamalian, K., Bazrafcan, L., Keshavarzy, F. & Shahraki, H. R. The effects of mindfulness training on the level of happiness and blood sugar in diabetes patients. J. Diabetes Metab. Disord . 19 , 311–317 2020.
Maddock, A., Hevey, D., D’Alton, P. & Kirby, B. A randomized trial of mindfulness-based cognitive therapy with psoriasis patients. Mindfulness 10 , 2606–2619 (2019).
Dandan, P., Ruch, W. & Pang, D. Fusing character strengths and mindfulness interventions: benefits for job satisfaction and performance. J. Occup. Health Psychol. 24 , 150–162 (2019).
Nakamura, Y., Lipschitz, D. L., Kuhn, R., Kinney, A. Y. & Donaldson, G. W. Investigating efficacy of two brief mind-body intervention programs for managing sleep disturbance in cancer survivors: a pilot randomized controlled trial. J. Cancer Surviv. 7 , 165–182 (2013).
Norouzi, E. et al. Implementation of a mindfulness-based stress reduction (MBSR) program to reduce stress, anxiety, and depression and to improve psychological wellbeing among retired Iranian football players. Psychol. Sport Exerc. 47 , 101636 (2020).
Boryri, T., Navidian, A. & Marghzari, N. Comparison of the effect of muscle relaxation and guided imagery on happiness and fear of childbirth in primiparous women admitted to health care centers. Int. J. Womens Health Reprod. Sci. 7 , 490–495 (2019).
Guo, L., Zhang, J., Mu, L. & Ye, Z. Preventing postpartum depression with mindful self-compassion intervention: a randomized control study. J. Nerv. Ment. Dis. 208 , 101–107 (2020).
O’Leary, K. & Dockray, S. The effects of two novel gratitude and mindfulness interventions on wellbeing. J. Altern. Complement. Med. 21 , 243–245 (2015).
Black, D. S. & Amaro, H. Moment-by-Moment in Women’s Recovery (MMWR): mindfulness-based intervention effects on residential substance use disorder treatment retention in a randomized controlled trial. Behav. Res. Ther. 120 , 103437 (2019).
Dambrun, M. et al. Unified consciousness and the effect of body scan meditation on happiness: alteration of inner-body experience and feeling of harmony as central processes. Mindfulness 10 , 1530–1544 (2019).
Davis, M. C. & Zautra, A. J. An online mindfulness intervention targeting socioemotional regulation in fibromyalgia: results of a randomized controlled trial. Ann. Behav. Med. 46 , 273–284 (2013).
Hoffman, C. J. et al. Effectiveness of mindfulness-based stress reduction in mood, breast- and endocrine-related quality of life, and wellbeing in stage 0 to III breast cancer: a randomized, controlled trial. J. Clin. Oncol. 30 , 1335–1342 (2012).
Mak, W. W. S., Chan, A. T. Y., Cheung, E. Y. L., Lin, C. L. Y. & Ngai, K. C. S. Enhancing web-based mindfulness training for mental health promotion with the health action process approach: randomized controlled trial. J. Med. Internet Res. 17 , e8 (2015).
Noone, C. & Hogan, M. J. A randomised active-controlled trial to examine the effects of an online mindfulness intervention on executive control, critical thinking and key thinking dispositions in a university student sample. BMC Psychol. 6 , 13 (2018).
Oman, D., Hedberg, J. & Thoresen, C. E. Passage meditation reduces perceived stress in health professionals: a randomized, controlled trial. J. Consult. Clin. Psychol. 74 , 714–719 (2006).
Pinniger, R., Brown, R. F., Thorsteinsson, E. B. & McKinley, P. Tango programme for individuals with age-related macular degeneration. Br. J. Vis. Impair. 31 , 47–59 (2013).
Shapiro, S. L., Brown, K. W., Thoresen, C. & Plante, T. G. The moderation of mindfulness-based stress reduction effects by trait mindfulness: results from a randomized controlled trial. J. Clin. Psychol. 67 , 267–277 (2011).
Thompson, N. J. et al. Expanding the efficacy of project UPLIFT: distance delivery of mindfulness-based depression prevention to people with epilepsy. J. Consult. Clin. Psychol. 83 , 304–313 (2015).
Chambers, S. K. et al. A randomised controlled trial of a mindfulness intervention for men with advanced prostate cancer. BMC Cancer 13 , 89 (2013).
Liu, C., Chen, H., Liu, C. Y., Lin, R. T. & Chiou, W. K. The effect of loving-kindness meditation on flight attendants’ spirituality, mindfulness and subjective wellbeing. Healthcare 8 , 16 (2020).
Perez-Blasco, J., Viguer, P. & Rodrigo, M. F. Effects of a mindfulness-based intervention on psychological distress, wellbeing, and maternal self-efficacy in breast-feeding mothers: results of a pilot study. Arch. Womens Ment. Health 16 , 227–236 (2013).
Champion, L., Economides, M. & Chandler, C. The efficacy of a brief app-based mindfulness intervention on psychosocial outcomes in healthy adults: a pilot randomised controlled trial. PLoS ONE 13 , e0209482 (2018).
Antoni, M. H. et al. How stress management improves quality of life after treatment for breast cancer. J. Consult. Clin. Psychol. 74 , 1143–1152 (2006).
Bolier, L. et al. Workplace mental health promotion online to enhance wellbeing of nurses and allied health professionals: a cluster-randomized controlled trial. Internet Interv. 1 , 196–204 (2014).
Burckhardt, R., Manicavasagar, V., Batterham, P. J. & Hadzi-Pavlovic, D. A randomized controlled trial of strong minds: a school-based mental health program combining acceptance and commitment therapy and positive psychology. J. Sch. Psychol. 57 , 41–52 (2016).
Castro, C. A., Adler, A. B., McGurk, D. & Bliese, P. D. Mental health training with soldiers four months after returning from Iraq: randomization by platoon. J. Trauma. Stress 25 , 376–383 (2012).
Di, S., Wen, G. & Feng-Lin, C. Brief psychological intervention in patients with cervical cancer: a randomized controlled trial. Health Psychol. 35 , 1383–1391 (2016).
Fegg, M. J. et al. Existential behavioural therapy for informal caregivers of palliative patients: a randomised controlled trial. Psychooncology 22 , 2079–2086 (2013).
Frieswijk, N., Steverink, N., Buunk, B. P. & Slaets, J. P. J. The effectiveness of a bibliotherapy in increasing the self-management ability of slightly to moderately frail older people. Patient Educ. Counsel. 61 , 219–227 (2006).
Gigantesco, A. et al. A universal mental health promotion programme for young people in Italy. BioMed. Res. Int. 2015 , 345926 (2015).
Kemeny, M. E. et al. Contemplative/emotion training reduces negative emotional behavior and promotes prosocial responses. Emotion 12 , 338–350 (2012).
Kotsou, I., Nelis, D., Gregoire, J. & Mikolajczak, M. Emotional plasticity: conditions and effects of improving emotional competence in adulthood. J. Appl. Psychol. 96 , 827–839 (2011).
LeBlanc, S., Uzun, B., Pourseied, K. & Mohiyeddini, C. Effect of an emotion regulation training program on mental wellbeing. Int. J. Group Psychother. 67 , 108–123 (2017).
Maatouk, I. et al. Healthy ageing at work- Efficacy of group interventions on the mental health of nurses aged 45 and older: results of a randomised, controlled trial. PLoS ONE 13 , e0191000 (2018).
Reich, J. W. & Zautra, A. J. A perceived control intervention for at-risk older adults. Psychol. Aging 4 , 415–424 (1989).
Rini, C. et al. Automated internet-based pain coping skills training to manage osteoarthritis pain: a randomized controlled trial. Pain 156 , 837–848 (2015).
Roepke, A. M. et al. Randomized controlled trial of superbetter, a smartphone-based/internet-based self-help tool to reduce depressive symptoms. Games Health J. 4 , 235–246 (2015).
Ruini, C. et al. School intervention for promoting psychological wellbeing in adolescence. J. Behav. Ther. Exp. Psychiatry 40 , 522–532 (2009).
Steinhardt, M. & Dolbier, C. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. J. Am. Coll. Health 56 , 445–453 (2008).
Tunariu, A. D., Tribe, R., Frings, D. & Albery, I. P. The iNEAR programme: an existential positive psychology intervention for resilience and emotional wellbeing. Int. Rev. Psychiatry 29 , 362–372 (2017).
Drozd, F., Skeie, L. G., Kraft, P. & Kvale, D. A web-based intervention trial for depressive symptoms and subjective wellbeing in patients with chronic HIV infection. AIDS Care 26 , 1080–1089 (2014).
Dowling, K., Simpkin, A. J. & Barry, M. M. A cluster randomized-controlled trial of the mindout social and emotional learning program for disadvantaged post-primary school students. J. Youth Adolesc. 48 , 1245–1263 (2019).
Bateman, A. & Fonagy, P. A randomized controlled trial of a mentalization-based intervention (MBT-FACTS) for families of people with borderline personality disorder. Pers. Disord. 10 , 70–79 (2019).
Behrndt, E.-M. et al. Brief telephone counselling is effective for caregivers who do not experience any major life events—caregiver-related outcomes of the German day-care study. BMC Health Serv. Res. 19 , 20 (2019).
Coker, J. et al. Re-inventing yourself after spinal cord injury: a site-specific randomized clinical trial. Spinal Cord. 57 , 282–292 (2019).
Shirani, M., Kheirabadi, G., Sharifirad, G. & Keshvari, M. The effect of education program on health promotion behavior on successful aging. Iran. J. Nurs. Midwifery Res. 24 , 234–238 (2019).
Carrico, A. W. et al. Pilot randomized controlled trial of an integrative intervention with methamphetamine-using men who have sex with men. Arch. Sex. Behav. 44 , 1861–1867 (2015).
Heintzelman, S. J. et al. ENHANCE: evidence for the efficacy of a comprehensive intervention program to promote subjective wellbeing. J. Exp. Psychol. Appl. 26 , 360–383 (2020).
Keeman, A., Naswall, K., Malinen, S. & Kuntz, J. Employee wellbeing: evaluating a wellbeing intervention in two settings. Front. Psychol. 8 , 2135 (2017).
Kovacs, A. H. et al. Feasibility and outcomes in a pilot randomized controlled trial of a psychosocial intervention for adults with congenital heart disease. Can. J. Cardiol. 34 , 766–773 (2018).
Matvienko-Sikar, K. & Dockray, S. Effects of a novel positive psychological intervention on prenatal stress and wellbeing: a pilot randomised controlled trial. Women Birth 30 , e111–e118 (2017).
Miller, V. A., Silva, K., Friedrich, E., Robles, R. & Ford, C. A. Efficacy of a primary care-based intervention to promote parent-teen communication and wellbeing: a randomized controlled trial. J. Pediatr. 222 , 200–206 (2020).
Sanchez-Hernandez, O., Mendez, F. X., Ato, M. & Garber, J. Prevention of depressive symptoms and promotion of wellbeing in adolescents: a randomized controlled trial of the Smile Program. An. de Psicologia 35 , 300–313 (2019).
Schoeps, K., de la Barrera, U. & Montoya-Castilla, I. Impact of emotional development intervention program on subjective wellbeing of university students. High. Educ. 79 , 711–729 (2020).
Wang, C. et al. Effects of a mutual recovery intervention on mental health in depressed elderly community-dwelling adults: a pilot study. BMC Public Health 17 , 4 (2017).
Weber, S., Lorenz, C. & Hemmings, N. Improving stress and positive mental health at work via an app-based intervention: a large-scale multi-centre randomised control trial. Front. Psychol. 10 , 2745 (2019).
Cejudo, J., Losada, L. & Feltrero, R. Promoting social and emotional learning and subjective wellbeing: impact of the ‘Aislados’ intervention program in adolescents. Int. J. Environ. Res. Public Health 17 , 609 (2020).
PubMed Central Google Scholar
Miller, K. E. et al. Supporting Syrian families displaced by armed conflict: a pilot randomized controlled trial of the Caregiver Support Intervention. Child Abus. Negl. 106 , 104512 (2020).
Monteiro, F., Pereira, M., Canavarro, M. C. & Fonseca, A. Be a mom’s efficacy in enhancing positive mental health among postpartum women presenting low risk for postpartum depression: results from a pilot randomized trial. Int. J. Environ. Res. Public Health 17 , 29 (2020).
O’Dea, B. et al. A randomised controlled trial of a relationship-focussed mobile phone application for improving adolescents’ mental health. J. Child Psychol. Psychiatry 19 , 899–913 (2020).
Sodani, M., Mehregan, S. B. & Honarmand, M. M. An investigation into the effectiveness of group life skills training on life expectancy and psychological wellbeing of female students. Prensa Méd. Argent. 105 , 710–719 (2019).
Wingert, J. R., Jones, J. C., Swoap, R. A. & Wingert, H. M. Mindfulness-based strengths practice improves wellbeing and retention in undergraduates: a preliminary randomized controlled trial. J. Am. Coll. Health https://doi.org/10.1080/07448481.2020.1764005 (2020).
Calear, A. L. et al. Cluster randomised controlled trial of the e-couch Anxiety and Worry program in schools. J. Affect. Disord. 196 , 210–217 (2016).
Chiang, K., Lu, R., Chu, H., Chang, Y. & Chou, K. Evaluation of the effect of a life review group program on self-esteem and life satisfaction in the elderly. Int. J. Geriatr. Psychiatry 23 , 7–10 (2008).
Goldstein, E. D. Sacred moments: Implications on well being and stress. J. Clin. Psychol. 63 , 1001–1019 (2007).
Jennings, P. A., Frank, J. L., Snowberg, K. E., Coccia, M. A. & Greenberg, M. T. Improving classroom learning environments by Cultivating Awareness and Resilience in Education (CARE): results of a randomized controlled trial. Sch. Psychol. Q. 28 , 374–390 (2013).
Karimi, Z., Rezaee, N., Shakiba, M. & Navidian, A. The effect of group counseling based on quality of life therapy on stress and life satisfaction in family caregivers of individuals with substance use problem: a randomized controlled trial. Issues Ment. Health Nurs. 40 , 1012–1018 (2019).
Stallman, H. M. Efficacy of the My Coping Plan mobile application in reducing distress: a randomised controlled trial. Clin. Psychologist 23 , 206–212 (2019).
Schoeps, K., Tamarit, A., de la Barrera, U. & Gonzalez Barron, R. Effects of emotional skills training to prevent burnout syndrome in schoolteachers. Ansiedad y. Estres 25 , 7–13 (2019).
Nikrahan, G. R. et al. Randomized controlled trial of a wellbeing intervention in cardiac patients. Gen. Hospital Psychiatry 61 , 116–124 (2019).
Boselie, J. J. L. M., Vancleef, L. M. G. & Peters, M. L. Filling the glass: effects of a positive psychology intervention on executive task performance in chronic pain patients. Eur. J. Pain 22 , 1268–1280 (2018).
Burckhardt, R. et al. A web-based adolescent positive psychology program in schools: randomized controlled trial. J. Med. Internet Res. 17 , e187 (2015).
Cantarella, A., Borella, E., Marigo, C. & De Beni, R. Benefits of wellbeing training in healthy older adults. Appl. Psychol. Health Wellbeing 9 , 261–284 (2017).
Cheung, E. O. et al. A randomized pilot trial of a positive affect skill intervention (lessons in linking affect and coping) for women with metastatic breast cancer. Psychooncology 26 , 2101–2108 (2017).
Cohn, M. A., Pietrucha, M. E., Saslow, L. R., Hult, J. R. & Moskowitz, J. T. An online positive affect skills intervention reduces depression in adults with type 2 diabetes. J. Posit. Psychol. 9 , 523–534 (2014).
Deane, F. P., Marshall, S., Crowe, T., White, A. & Kavanagh, D. A randomized controlled trial of a correspondence-based intervention for carers of relatives with psychosis. Clin. Psychol. Psychother. 22 , 142–152 (2015).
Gander, F., Proyer, R. T. & Ruch, W. Positive psychology interventions addressing pleasure, engagement, meaning, positive relationships, and accomplishment increase wellbeing and ameliorate depressive symptoms: a randomized, placebo-controlled online study. Front. Psychol. 7 , 686 (2016).
Giannopoulos, V. L. & Vella-Brodrick, D. A. Effects of positive interventions and orientations to happiness on subjective wellbeing. J. Posit. Psychol. 6 , 95–105 (2011).
Ho, H. C. Y. et al. Happy Family Kitchen II: a cluster randomized controlled trial of a community-based family intervention for enhancing family communication and wellbeing in Hong Kong. Front. Psychol. 7 , 638 (2016).
Jaser, S. S., Patel, N., Rothman, R. L., Choi, L. & Whittemore, R. Check it! A randomized pilot of a positive psychology intervention to improve adherence in adolescents with type 1 diabetes. Diabetes Educ. 40 , 659–667 (2014).
Koydemir, S. & Sun-Selisik, Z. Wellbeing on campus: testing the effectiveness of an online strengths-based intervention for first year college students. Br. J. Guid. Counsell. 44 , 434–446 (2016).
Kwok, S. Y. C. L., Gu, M. & Kit, K. T. K. Positive psychology intervention to alleviate child depression and increase life satisfaction. Res. Soc. Work Pract. 26 , 350–361 (2016).
Manicavasagar, V. et al. Feasibility and effectiveness of a web-based positive psychology program for youth mental health: randomized controlled trial. J. Med. Internet Res. 16 , e140 (2014).
Mohammadi, N. et al. A randomized trial of an optimism training intervention in patients with heart disease. Gen. Hospital Psychiatry 51 , 46–53 (2018).
Moskowitz, J. T. et al. Randomized controlled trial of a positive affect intervention for people newly diagnosed with HIV. J. Consult. Clin. Psychol. 85 , 409–423 (2017).
Neumeier, L. M., Brook, L., Ditchburn, G. & Sckopke, P. Delivering your daily dose of wellbeing to the workplace: a randomized controlled trial of an online wellbeing programme for employees. Eur. J. Work Organ. Psychol. 26 , 555–573 (2017).
Moeenizadeh, M. & Zarif, H. The efficacy of wellbeing therapy for depression in infertile women. Int. J. Fertil. Steril. 10 , 363–370 (2017).
Nikrahan, G. R. et al. Positive psychology interventions for patients with heart disease: a preliminary randomized trial. Psychosomatics 57 , 348–358 (2016).
Page, K. M. & Vella-Brodrick, D. A. The working for wellness program: RCT of an employee wellbeing intervention. J. Happiness Stud. 14 , 1007–1031 (2013).
Pietrowsky, R. & Mikutta, J. Effects of positive psychology interventions in depressive patients—a randomized control study. Psychology 3 , 1067–1073 (2012).
Proyer, R. T., Gander, F., Wellenzohn, S. & Ruch, W. Addressing the role of personality, ability, and positive and negative affect in positive psychology interventions: findings from a randomized intervention based on the authentic happiness theory and extensions. J. Posit. Psychol. 11 , 609–621 (2016).
Roth, R. A., Suldo, S. M. & Ferron, J. M. Improving middle school students’ subjective wellbeing: efficacy of a multicomponent positive psychology intervention targeting small groups of youth. Sch. Psychol. Rev. 46 , 21–41 (2017).
Sanjuan, P. et al. A randomised trial of a positive intervention to promote wellbeing in cardiac patients. Appl. Psychol. Health Wellbeing 8 , 64–84 (2016).
Suldo, S. M., Savage, J. A. & Mercer, S. H. Increasing middle school students’ life satisfaction: efficacy of a positive psychology group intervention. J. Happiness Stud. 15 , 19–42 (2014).
Taylor, C. T., Lyubomirsky, S. & Stein, M. B. Upregulating the positive affect system in anxiety and depression: outcomes of a positive activity intervention. Depress. anxiety 34 , 267–280 (2017).
Asl, S. T. et al. Effect of group positive psychotherapy on improvement of life satisfaction and the quality of life in infertile woman. Int. J. Fertil. Steril. 10 , 105–112 (2016).
Dowlatabadi, M. M. et al. The effectiveness of group positive psychotherapy on depression and happiness in breast cancer patients: a randomized controlled trial. Electron. Physician 8 , 2175–2180 (2016).
Seligman, M. E., Rashid, T. & Parks, A. C. Positive psychotherapy. Am. Psychol. 61 , 774 (2006).
Proyer, R. T., Ruch, W. & Buschor, C. Testing strengths-based interventions: a preliminary study on the effectiveness of a program targeting curiosity, gratitude, hope, humor, and zest for enhancing life satisfaction. J. Happiness Stud. 14 , 275–292 (2013).
Shoshani, A., Steinmetz, S. & Kanat-Maymon, Y. Effects of the Maytiv positive psychology school program on early adolescents’ wellbeing, engagement, and achievement. J. Sch. Psychol. 57 , 73–92 (2016).
Kloos, N., Drossaert, C. H. C., Bohlmeijer, E. T. & Westerhof, G. J. Online positive psychology intervention for nursing home staff: a cluster-randomized controlled feasibility trial of effectiveness and acceptability. Int. J. Nurs. Stud. 98 , 48–56 (2019).
Xu, Y. Y., Wu, T., Yu, Y. J. & Li, M. A randomized controlled trial of wellbeing therapy to promote adaptation and alleviate emotional distress among medical freshmen. BMC Med. Educ. 19 , 182 (2019).
Antoine, P., Andreotti, E. & Congard, A. Positive psychology intervention for couples: a pilot study. Stress Health. 36 , 179–190 (2020).
Carrico, A. W. et al. Randomized controlled trial of a positive affect intervention to reduce HIV viral load among sexual minority men who use methamphetamine. J. Int. AIDS Soc. 22 , e25436 (2019).
Celano, C. M. et al. A positive psychology intervention for patients with bipolar depression: a randomized pilot trial. J. Ment. Health 29 , 60–68 (2020).
Coelhoso, C. C. et al. A new mental health mobile app for wellbeing and stress reduction in working women: randomized controlled trial. J. Med. Internet Res. 21 , e14269 (2019).
Greer, S. et al. Use of the chatbot ‘Vivibot’ to deliver positive psychology skills and promote wellbeing among young people after cancer treatment: randomized controlled feasibility trial. JMIR Mhealth Uhealth 7 , e15018 (2019).
Hendriks, T. et al. Resilience and wellbeing in the Caribbean: findings from a randomized controlled trial of a culturally adapted multi-component positive psychology intervention. J. Posit. Psychol. 15 , 238–253 (2020).
Mazlomi Barm Sabz, A., Asgari, P., Makvandi, B., Ehteshamzadeh, P. & Bakhtiyar Pour, S. Comparison of the effectiveness of positive psychology and emotion regulation training interventions in promoting the psychological wellbeing in nar-anon group. Int. J. Ment. Health Addiction https://doi.org/10.1007/s11469-020-00284-2 (2020).
Murdoch, K. C. et al. The efficacy of the strength, hope and resourcefulness program for people with Parkinson’s disease (SHARP-PWP): a mixed methods study. Parkinsonism Relat. Disord. 70 , 7–12 (2020).
Osborn, T. L. et al. Single-session digital intervention for adolescent depression, anxiety, and wellbeing: outcomes of a randomized controlled trial with Kenyan adolescents. J. Consult. Clin. Psychol. 88 , 657–668 (2020).
Poole, A. E. & Malouff, J. M. Preliminary experimental evaluation of a behavioral-cognitive method of increasing life excitement. J. Posit. Psychol. Wellbeing 3 , 26–44 (2019).
Radstaak, M., Huning, L. & Bohlmeijer, E. T. Wellbeing therapy as rehabilitation therapy for posttraumatic stress disorder symptoms: a randomized controlled trial. J. Trauma. Stress 33 , 813–823 (2020).
Schotanus-Dijkstra, M. et al. An early intervention to promote wellbeing and flourishing and reduce anxiety and depression: a randomized controlled trial. Internet Intervent. 9 , 15–24 (2017).
Shaghaghi, F., Abedian, Z., Forouhar, M., Esmaily, H. & Eskandarnia, E. Effect of positive psychology interventions on psychological wellbeing of midwives: a randomized clinical trial. J. Educ. Health Promot. 8 , 160 (2019).
Weiss, L. A., Oude Voshaar, M. A., Bohlmeijer, E. T. & Westerhof, G. J. The long and winding road to happiness: a randomized controlled trial and cost-effectiveness analysis of a positive psychology intervention for lonely people with health problems and a low socio-economic status. Health Qual. Life Outcomes 18 , 162 (2020).
Taghvaienia, A. & Alamdari, N. Effect of positive psychotherapy on psychological wellbeing, happiness, life expectancy and depression among retired teachers with depression: a randomized controlled trial. Commun. Ment. Health J. 56 , 229–237 (2020).
Hausmann, L. R. et al. Effect of a positive psychological intervention on pain and functional difficulty among adults with osteoarthritis: a randomized clinical trial. JAMA Netw. Open 1 , e182533 (2018).
Gander, F., Proyer, R. T., Ruch, W. & Wyss, T. Strength-based positive interventions: further evidence for their potential in enhancing wellbeing and alleviating depression. J. Happiness Stud. 14 , 1241–1259 (2013).
Bolier, L. et al. An Internet-based intervention to promote mental fitness for mildly depressed adults: randomized controlled trial. J. Med. Internet Res. 15 , e200 (2013).
Celano, C. M. et al. Psychological interventions to reduce suicidality in high-risk patients with major depression: a randomized controlled trial. Psychol. Med. 47 , 810–821 (2017).
Cerezo, M. V., Ortiz-Tallo, M., Cardenal, V. & de la Torre-Luque, A. Positive psychology group intervention for breast cancer patients: a randomised trial. Psychol. Rep. 115 , 44–64 (2014).
Dowling, G. A. et al. Life enhancing activities for family caregivers of people with frontotemporal dementia. Alzheimer Dis. Assoc. Disord. 28 , 175–181 (2014).
Drozd, F., Mork, L., Nielsen, B., Raeder, S. & Bjorkli, C. A. Better days—a randomized controlled trial of an internet-based positive psychology intervention. J. Posit. Psychol. 9 , 377–388 (2014).
Feicht, T. et al. Evaluation of a seven-week web-based happiness training to improve psychological wellbeing, reduce stress, and enhance mindfulness and flourishing: a randomized controlled occupational health study. Evid. Based Complement. Alternat. Med. 2013 , 676953 (2013).
Hausmann, L. R. et al. Testing a positive psychological intervention for osteoarthritis. Pain. Med. 18 , 1908–1920 (2017).
Lü, W., Wang, Z. & Liu, Y. A pilot study on changes of cardiac vagal tone in individuals with low trait positive affect: the effect of positive psychotherapy. Int. J. Psychophysiol. 88 , 213–217 (2013).
Schrank, B. et al. Evaluation of a positive psychotherapy group intervention for people with psychosis: pilot randomised controlled trial. Epidemiol. Psychiatr. Sci. 25 , 235–246 (2016).
Shoshani, A. & Slone, M. Positive education for young children: effects of a positive psychology intervention for preschool children on subjective well being and learning behaviors. Front. Psychol. 8 , 1866 (2017).
Seyedi Asl, S. T. et al. Effect of group positive psychotherapy on improvement of life satisfaction and the quality of life in infertile woman. Int. J. Fertil. Steril. 10 , 105–112 (2016).
Muller, R. et al. Effects of a tailored positive psychology intervention on wellbeing and pain in individuals with chronic pain and a physical disability: a feasibility trial. Clin. J. Pain. 32 , 32–44 (2016).
King, L. A. The health benefits of writing about life goals. Pers. Soc. Psychol. Bull. 27 , 798–807 (2001).
Layous, K., Nelson, S., Kurtz, J. L. & Lyubomirsky, S. What triggers prosocial effort? A positive feedback loop between positive activities, kindness, and wellbeing. J. Posit. Psychol. 12 , 385–398 (2017).
Littman-Ovadia, H. & Nir, D. Looking forward to tomorrow: The buffering effect of a daily optimism intervention. J. Posit. Psychol. 9 , 122–136 (2014).
Manthey, L., Vehreschild, V. & Renner, K.-H. Effectiveness of two cognitive interventions promoting happiness with video-based online instructions. J. Happiness Stud. 17 , 319–339 (2016).
Molinari, G. et al. The power of visualization: Back to the future for pain management in fibromyalgia syndrome. Pain. Med. 19 , 1451–1468 (2017).
Odou, N. & Vella-Brodrick, D. A. The efficacy of positive psychology interventions to increase wellbeing and the role of mental imagery ability. Soc. Indic. Res. 110 , 111–129 (2013).
Peters, M. L., Flink, I. K., Boersma, K. & Linton, S. J. Manipulating optimism: can imagining a best possible self be used to increase positive future expectancies? J. Posit. Psychol. 5 , 204–211 (2010).
Quoidbach, J. & Dunn, E. W. Give it up: a strategy for combating hedonic adaptation. Soc. Psychological Pers. Sci. 4 , 563–568 (2013).
Seear, K. H. & Vella-Brodrick, D. A. Efficacy of positive psychology interventions to increase wellbeing: examining the role of dispositional mindfulness. Soc. Indic. Res. 114 , 1125–1141 (2013).
Sheldon, K. M. & Lyubomirsky, S. How to increase and sustain positive emotion: the effects of expressing gratitude and visualizing best possible selves. J. Posit. Psychol. 1 , 73–82 (2006).
Lyubomirsky, S., Dickerhoof, R., Boehm, J. K. & Sheldon, K. M. Becoming happier takes both a will and a proper way: an experimental longitudinal intervention to boost wellbeing. Emotion 11 , 391–402 (2011).
Ng, W. Use of positive interventions: does neuroticism moderate the sustainability of their effects on happiness? J. Posit. Psychol. 11 , 51–61 (2016).
Enrique Roig, A. et al. Implementation of a positive technology application in patients with eating disorders: a pilot randomized control trial. Front. Psychol. 9 , 934 (2018).
Auyeung, L. & Mo, P. K. H. The efficacy and mechanism of online positive psychological intervention (PPI) on improving wellbeing among Chinese university students: a pilot study of the best possible self (BPS) intervention. J. Happiness Stud. 20 , 2525–2550 (2019).
Heekerens, J. B., Eid, M. & Heinitz, K. Dealing with conflict: reducing goal ambivalence using the best-possible-self intervention. J. Posit. Psychol. 15 , 325–337 (2020).
Quoidbach, J., Wood, A. M. & Hansenne, M. Back to the future: the effect of daily practice of mental time travel into the future on happiness and anxiety. J. Posit. Psychol. 4 , 349–355 (2009).
Carrillo, A., Etchemendy, E. & Baños, R. M. My best self in the past, present or future: results of two randomized controlled trials. J. Happiness Stud. 22 , 955–980 (2021).
Boehm, J. K., Lyubomirsky, S. & Sheldon, K. M. A longitudinal experimental study comparing the effectiveness of happiness-enhancing strategies in Anglo Americans and Asian Americans. Cognition Emot. 25 , 1263–1272 (2011).
Khanna, P. & Singh, K. Do all positive psychology exercises work for everyone? replication of Seligman et al.’s (2005) interventions among adolescents. Psychol. Stud. 64 , https://doi.org/10.1007/s12646-019-00477-3 (2019).
Owens, R. L. & Patterson, M. M. Positive psychological interventions for children: a comparison of gratitude and best possible selves approaches. J. Genet. Psychol. 174 , 403–428 (2013).
Peters, M. L., Meevissen, Y. M. C. & Hanssen, M. M. Specificity of the best possible self intervention for increasing optimism: comparison with a gratitude intervention. Posit. Psychol. 31 , 93–100 (2013).
Enrique, Á., Bretón-López, J., Molinari, G., Baños, R. M. & Botella, C. Efficacy of an adaptation of the best possible self intervention implemented through positive technology: a randomized control trial. Appl. Res. Qual. Life 13 , 671–689 (2018).
Duan, W., Ho, S. M. Y., Tang, X., Li, T. & Zhang, Y. Character strength-based intervention to promote satisfaction with life in the Chinese university context. J. Happiness Stud. 15 , 1347–1361 (2014).
Proyer, R. T., Gander, F., Wellenzohn, S. & Ruch, W. Positive psychology interventions in people aged 50–79 years: long-term effects of placebo-controlled online interventions on wellbeing and depression. Aging Ment. health 18 , 997–1005 (2014).
Proyer, R. T., Gander, F., Wellenzohn, S. & Ruch, W. Strengths-based positive psychology interventions: a randomized placebo-controlled online trial on long-term effects for a signature strengths- vs. a lesser strengths-intervention. Front. Psychol. 6 , 456 (2015).
Mitchell, J., Stanimirovic, R., Klein, B. & Vella-Brodrick, D. A randomised controlled trial of a self-guided internet intervention promoting wellbeing. Comput. Hum. Behav. 25 , 749–760 (2009).
Senf, K. & Liau, A. K. The effects of positive interventions on happiness and depressive symptoms, with an examination of personality as a moderator. J. Happiness Stud. 14 , 591–612 (2013).
Mongrain, M. & Anselmo-Matthews, T. Do positive psychology exercises work? A replication of Seligman et al. (2005). J. Clin. Psychol. 68 , 382–389 (2012).
Duan, W. & Bu, H. Randomized trial investigating of a single-session character-strength-based cognitive intervention on freshman’s adaptability. Res. Soc. Work Pract. 29 , 82–92 (2019).
Dolev-Amit, T., Rubin, A. & Zilcha-Mano, S. Is awareness of strengths intervention sufficient to cultivate wellbeing and other positive outcomes? J. Happiness Stud. 22 , 645–666 (2021).
Woodworth, R. J., O’Brien-Malone, A., Diamond, M. R. & Schuz, B. Web-based positive psychology interventions: a reexamination of effectiveness. J. Clin. Psychol. 73 , 218–232 (2017).
Chérif, L., Wood, V. M. & Watier, C. Testing the effectiveness of a strengths-based intervention targeting all 24 strengths: results from a randomized controlled trial. Psychol. Rep . 0033294120937441 (2020).
Al-Seheel, A. Y. & Noor, N. M. Effects of an Islamic-based gratitude strategy on Muslim students’ level of happiness. Ment. Health Relig. Cult. 19 , 686–703 (2016).
Algoe, S. B. & Zhaoyang, R. Positive psychology in context: effects of expressing gratitude in ongoing relationships depend on perceptions of enactor responsiveness. J. Posit. Psychol. 11 , 399–415 (2016).
Deng, Y. et al. Counting blessings and sharing gratitude in a Chinese prisoner sample: effects of gratitude-based interventions on subjective wellbeing and aggression. J. Posit. Psychol. 14 , 303–311 (2019).
Froh, J. J., Sefick, W. J. & Emmons, R. A. Counting blessings in early adolescents: an experimental study of gratitude and subjective wellbeing. J. Sch. Psychol. 46 , 213–233 (2008).
Froh, J. J., Kashdan, T. B., Ozimkowski, K. M. & Miller, N. Who benefits the most from a gratitude intervention in children and adolescents? Examining positive affect as a moderator. J. Posit. Psychol. 4 , 408–422 (2009).
Froh, J. J. et al. Nice thinking! An educational intervention that teaches children to think gratefully. Sch. Psychol. Rev. 43 , 132–152 (2014).
Jackowska, M., Brown, J., Ronaldson, A. & Steptoe, A. The impact of a brief gratitude intervention on subjective wellbeing, biology and sleep. J. Health Psychol. 21 , 2207–2217 (2016).
Krentzman, A. R. et al. Feasibility, acceptability, and impact of a web-based gratitude exercise among individuals in outpatient treatment for alcohol use disorder. J. Posit. Psychol. 10 , 477–488 (2015).
Miller, R. W. & Duncan, E. A pilot randomised controlled trial comparing two positive psychology interventions for their capacity to increase subjective wellbeing. Counsell. Psychol. Rev. 30 , 36–46 (2015).
Otsuka, Y., Hori, M. & Kawahito, J. Improving wellbeing with a gratitude exercise in Japanese workers: a randomized controlled trial. Int. J. Psychol. Counsell. 4 , 86–91 (2012).
Watkins, P. C., Uhder, J. & Pichinevskiy, S. Grateful recounting enhances subjective wellbeing: the importance of grateful processing. J. Posit. Psychol. 10 , 91–98 (2015).
Ghandeharioun, A., Azaria, A., Taylor, S. & Picard, R. W. ‘Kind and Grateful’: a context-sensitive smartphone app utilizing inspirational content to promote gratitude. Psychol. Wellbeing 6 , 9 (2016).
Sergeant, S. & Mongrain, M. Are positive psychology exercises helpful for people with depressive personality styles? J. Posit. Psychol. 6 , 260–272 (2011).
Cunha, L. F., Pellanda, L. C. & Reppold, C. T. Positive psychology and gratitude interventions: a randomized clinical trial. Front. Psychol. 10 , 584 (2019).
Koay, S. H., Ng, A. T., Tham, S. K. & Tan, C. S. Gratitude intervention on Instagram: an experimental study. Psychol. Stud. 65 , 168–173 (2020).
Shin, L. J. Gratitude in collectivist and individualist cultures. J. Posit. Psyshol. 15 , 598–604 (2020).
Bohlmeijer, E. T., Kraiss, J. T., Watkins, P. & Schotanus-Dijkstra, M. Promoting gratitude as a resource for sustainable mental health: results of a 3-armed randomized controlled trial up to 6 months follow-up. J. Happiness Stud. 22 , 1011–1032 (2021).
Kerr, S. L., O’Donovan, A. & Pepping, C. A. Can gratitude and kindness interventions enhance wellbeing in a clinical sample? J. Happiness Stud. 16 , 17–36 (2015).
Lau, R. W. L. & Cheng, S.-T. Gratitude orientation reduces death anxiety but not positive and negative affect. Omega 66 , 79–88 (2012).
Lau, R. W. L. & Cheng, S.-T. Gratitude lessens death anxiety. Eur. J. Ageing 8 , 169 (2011).
O’Connell, B. H., O’Shea, D. & Gallagher, S. Enhancing social relationships through positive psychology activities: a randomised controlled trial. J. Posit. Psychol. 11 , 149–162 (2016).
O’Connell, B. H., O’Shea, D. & Gallagher, S. Examining psychosocial pathways underlying gratitude interventions: a randomized controlled trial. J. Happiness Stud. 19 , 2421–2444 (2018).
Renshaw, T. L. & Rock, D. K. Effects of a brief grateful thinking intervention on college students’ mental health. Ment. Health Prev. 9 , 19–24 (2018).
O’Connell, B. H., O’Shea, D. & Gallagher, S. Feeling thanks and saying thanks: a randomized controlled trial examining if and how socially oriented gratitude journals work. J. Clin. Psychol. 73 , 1280–1300 (2017).
Froh, J. J., Sefick, W. J. & Emmons, R. A. Counting blessings in early adolescents: an experimental study of gratitude and subjective wellbeing. J. Sch. Psychol. 46 , 213–233 (2009).
Drewery, D. W., Cormier, L. A., Pretti, T. J. & Church, D. Improving unmatched co-op students’ emotional wellbeing: test of two brief interventions. Int. J. Work-Integr. Learn. 20 , 43–53 (2019).
Hoeppner, B. B., Schick, M. R., Carlon, H. & Hoeppner, S. S. Do self-administered positive psychology exercises work in persons in recovery from problematic substance use? An online randomized survey. J. Subst. Abus. Treat. 99 , 16–23 (2019).
Tagalidou, N., Baier, J. & Laireiter, A. R. The effects of three positive psychology interventions using online diaries: a randomized-placebo controlled trial. Internet Intervent. 17 , 100242 (2019).
Gander, F., Proyer, R. T., Hentz, E. & Ruch, W. Working mechanisms in positive interventions: a study using daily assessment of positive emotions. J. Posit. Psychol. 15 , 633–638 (2020).
Martínez-Martí, M. L., Avia, M. D. & Hernández-Lloreda, M. J. Effects of an appreciation of beauty randomized-controlled trial web-based intervention on appreciation of beauty and wellbeing. Psychol. Aesthet. Creat. Arts 12 , 272 (2018).
Buchanan, K. E. & Bardi, A. Acts of kindness and acts of novelty affect life satisfaction. J. Soc. Psychol. 150 , 235–237 (2010).
Alden, L. E. & Trew, J. L. If it makes you happy: engaging in kind acts increases positive affect in socially anxious individuals. Emotion 13 , 64–75 (2013).
Ko, K., Margolis, S., Revord, J. & Lyubomirsky, S. Comparing the effects of performing and recalling acts of kindness. J. Posit. Psychol. 16 , 73–81 (2021).
Wang, M.-C., Tran, K. K., Nyutu, P. N. & Fleming, E. Doing the right thing: a mixed-methods study focused on generosity and positive wellbeing. J. Creativity Ment. Health 9 , 318–331 (2014).
Hurley, D. B. & Kwon, P. Results of a study to increase savoring the moment: differential impact on positive and negative outcomes. J. Happiness Stud. 13 , 579–588 (2012).
Layous, K., Kurtz, J., Chancellor, J. & Lyubomirsky, S. Reframing the ordinary: imagining time as scarce increases wellbeing. J. Posit. Psychol. 13 , 301–308 (2018).
Smith, J. L. & Bryant, F. B. Enhancing positive perceptions of aging by savoring life lessons. Aging Ment. Health 23 , 762–770 (2019).
Palmer, C. A. & Gentzler, A. L. Adults’ self-reported attachment influences their savoring ability. J. Posit. Psychol. 13 , 290–300 (2018).
Wellenzohn, S., Proyer, R. T. & Ruch, W. Humor-based online positive psychology interventions: a randomized placebo-controlled long-term trial. J. Posit. Psychol. 11 , 584–594 (2016).
Martinez-Marti, M. L., Avia, M. D. & Hernandez-Lloreda, M. J. The effects of counting blessings on subjective wellbeing: a gratitude intervention in a Spanish sample. Span. J. Psychol. 13 , 886–896 (2010).
van der Spek, N. et al. Efficacy of meaning-centered group psychotherapy for cancer survivors: a randomized controlled trial. Psychol. Med. 47 , 1990–2001 (2017).
Chancellor, J., Margolis, S., Jacobs Bao, K. & Lyubomirsky, S. Everyday prosociality in the workplace: the reinforcing benefits of giving, getting, and glimpsing. Emotion 18 , 507–517 (2018).
Chancellor, J., Layous, K. & Lyubomirsky, S. Recalling positive events at work makes employees feel happier, move more, but interact less: a 6-week randomized controlled intervention at a Japanese workplace. J. Happiness Stud. 16 , 871–887 (2015).
Hurley, M. V., Walsh, N. E., Mitchell, H., Nicholas, J. & Patel, A. Long-term outcomes and costs of an integrated rehabilitation program for chronic knee pain: a pragmatic, cluster randomized, controlled trial. Arthritis Care Res. 64 , 238–247 (2012).
Cook, E. A. Effects of reminiscence on life satisfaction of elderly female nursing home residents. Health Care Women Int. 19 , 109–118 (1998).
Davis, M. C. Life review therapy as an intervention to manage depression and enhance life satisfaction in individuals with right hemisphere cerebral vascular accidents. Issues Ment. Health Nurs. 25 , 503–515 (2004).
Franklin, F. C. & Cheung, M. Legacy interventions with patients with co-occurring disorders: legacy definitions, life satisfaction, and self-efficacy. Subst. Use Misuse 52 , 1840–1849 (2017).
Hallford, D. J. & Mellor, D. Brief reminiscence activities improve state wellbeing and self-concept in young adults: a randomised controlled experiment. Memory 24 , 1311–1320 (2016).
Latorre, J. M. et al. Life review based on remembering specific positive events in active aging. J. Aging Health 27 , 140–157 (2015).
Mei, Y., Lin, B., Li, Y., Ding, C. & Zhang, Z. Effects of modified 8-week reminiscence therapy on the older spouse caregivers of stroke survivors in Chinese communities: a randomized controlled trial. Int. J. Geriatr. Psychiatry 33 , 633–641 (2018).
Preschl, B. et al. Life-review therapy with computer supplements for depression in the elderly: a randomized controlled trial. Aging Ment. Health 16 , 964–974 (2012).
Rattenbury, C. & Stones, M. J. A controlled evaluation of reminiscence and current topics discussion groups in a nursing home context. Gerontologist 29 , 768–771 (1989).
Yousefi, Z., Sharifi, K., Tagharrobi, Z. & Akbari, H. The effect of narrative reminiscence on happiness of elderly women. Iran. Red Crescent Med. J. 17 , e19612 (2015).
Cook, E. A. The effects of reminiscence on psychological measures of ego integrity in elderly nursing home residents. Arch. Psychiatr. Nurs. 5 , 292–298 (1991).
Westerhof, G. J., Lamers, S. M. A., Postel, M. G. & Bohlmeijer, E. T. Online therapy for depressive symptoms: an evaluation of counselor-led and peer-supported life review therapy. Gerontologist 59 , 135–146 (2019).
Dong, X. et al. Telephone-based reminiscence therapy for colorectal cancer patients undergoing postoperative chemotherapy complicated with depression: a three-arm randomised controlled trial. Support. Care Cancer 27 , 2761–2769 (2019).
Bryant, F. B., Osowski, K. A. & Smith, J. L. Gratitude as a mediator of the effects of savoring on positive adjustment to aging. Int. J. Aging Hum. Dev. 92 , 275–300 (2021).
Westerhof, G. J., Korte, J., Eshuis, S. & Bohlmeijer, E. T. Precious memories: A randomized controlled trial on the effects of an autobiographical memory intervention delivered by trained volunteers in residential care homes. Aging Ment. Health 22 , 1494–1501 (2018).
Korte, J., Bohlmeijer, E., Cappeliez, P., Smit, F. & Westerhof, G. Life review therapy for older adults with moderate depressive symptomatology: a pragmatic randomized controlled trial. Psychol. Med. 42 , 1163–1173 (2012).
Lan, X., Xiao, H., Chen, Y. & Zhang, X. Effects of life review intervention on life satisfaction and personal meaning among older adults with frailty. J. Psychosoc. Nurs. Ment. Health Serv. 56 , 30–36 (2018).
Zhou, W. et al. The effects of group reminiscence therapy on depression, self-esteem, and affect balance of Chinese community-dwelling elderly. Arch. Gerontol. Geriatr. 54 , e440–e447 (2012).
Lai, C. K. Y., Chin, K. C. W., Zhang, Y. & Chan, E. A. Psychological outcomes of life story work for community‐dwelling seniors: a randomised controlled trial. Int. J. Older People Nurs. 14 , e12238 (2019).
Hijazi, A. M. et al. Brief narrative exposure therapy for posttraumatic stress in Iraqi refugees: a preliminary randomized clinical trial. J. Trauma. Stress 27 , 314–322 (2014).
Hilpert, P., Bodenmann, G., Nussbeck, F. W. & Bradbury, T. N. Improving personal happiness through couple intervention: a randomized controlled trial of a self-directed couple enhancement program. J. Happiness Stud. 17 , 213–237 (2016).
Tsivos, Z.-L., Calam, R., Sanders, M. R. & Wittkowski, A. A pilot randomised controlled trial to evaluate the feasibility and acceptability of the Baby Triple P Positive Parenting Programme in mothers with postnatal depression. Clin. Child Psychol. Psychiatry 20 , 532–554 (2015).
Yamada, T., Kawamata, H., Kobayashi, N., Kielhofner, G. & Taylor, R. R. A randomised clinical trial of a wellness programme for healthy older people. Br. J. Occup. Ther. 73 , 540–548 (2010).
Fabrizio, C. S. et al. Parental emotional management benefits family relationships: a randomized controlled trial in Hong Kong, China. Behav. Res. Ther. 71 , 115–124 (2015).
Simkiss, D. E. et al. Effectiveness and cost-effectiveness of a universal parenting skills programme in deprived communities: multicentre randomised controlled trial. 3 , e002851 (2013).
McGowan, S. K. & Behar, E. A preliminary investigation of stimulus control training for worry: effects on anxiety and insomnia. Behav. Modif. 37 , 90–112 (2013).
Reinke, B. J., Holmes, D. S. & Denney, N. W. Influence of a ‘friendly visitor’ program on the cognitive functioning and morale of elderly persons. Am. J. Community Psychol. 9 , 491–504 (1981).
Cheng, S.-T., Fung, H. H., Chan, W. C. & Lam, L. C. W. Short-term effects of a gain-focused reappraisal intervention for dementia caregivers: a double-blind cluster-randomized controlled trial. Am. J. Geriatr. Psychiatry 24 , 740–750 (2016).
Larson, J. et al. The impact of a nurse-led support and education programme for spouses of stroke patients: a randomized controlled trial. J. Clin. Nurs. 14 , 995–1003 (2005).
Arola, A., Dahlin-Ivanoff, S. & Haggblom-Kronlof, G. Impact of a person-centred group intervention on life satisfaction and engagement in activities among persons aging in the context of migration. Scand. J. Occup. Ther. 27 , 269–279 (2020).
Braganza, D. J., Piedmont, R. L., Fox, J., Fialkowski, G. M. & Gray, R. M. Examining the clinical efficacy of core transformation: a randomized clinical trial. J. Counsel. Dev. 97 , 293–305 (2019).
Kruizinga, R. et al. An assisted structured reflection on life events and life goals in advanced cancer patients: outcomes of a randomized controlled trial (Life InSight Application (LISA) study). Palliat. Med. 33 , 221–231 (2019).
Sullivan, G. J., Hain, D. J., Williams, C. & Newman, D. Story-sharing intervention to improve depression and wellbeing in older adults transitioning to long-term care. Res. Gerontol. Nurs. 12 , 81–90 (2019).
Hajisabbagh, N., Fereidooni-Moghadam, M., Masoudi, R. & Etemadifar, M. The effect of an emotional intelligence component program on happiness in patients with epilepsy. Epilepsy Behav. 106 , 106972 (2020).
Contractor, A. A., Banducci, A. N., Jin, L., Keegan, F. S. & Weiss, N. H. Effects of processing positive memories on posttrauma mental health: A preliminary study in a non-clinical student sample. J. Behav. Ther. Exp. Psychiatry 66 , 10156 (2020).
Zhang, T., Fu, H. & Wan, Y. The application of group forgiveness intervention for courtship-hurt college students: a Chinese perspective. Int. J. Group Psychother. 64 , 298–320 (2014).
Muller, A., Heiden, B., Herbig, B., Poppe, F. & Angerer, P. Improving wellbeing at work: a randomized controlled intervention based on selection, optimization, and compensation. J. Occup. Health Psychol. 21 , 169–181 (2016).
Read, A., Mazzucchelli, T. G. & Kane, R. T. A preliminary evaluation of a single session behavioural activation intervention to improve wellbeing and prevent depression in carers. Clin. Psychol. 20 , 36–45 (2016).
Xie, J. et al. A randomized study on the effect of modified behavioral activation treatment for depressive symptoms in rural left-behind elderly. Psychother. Res. 29 , 372–382 (2019).
Soucy, I., Provencher, M. D., Fortier, M. & McFadden, T. Secondary outcomes of the guided self-help behavioral activation and physical activity for depression trial. J. Ment. Health 28 , 410–418 (2019).
Hojjat, S. K. et al. The effectiveness of group assertiveness training on happiness in rural adolescent females with substance abusing parents. Glob. J. Health Sci. 8 , 156–164 (2015).
Coote, H. M. J. & MacLeod, A. K. A self-help, positive goal-focused intervention to increase wellbeing in people with depression. Clin. Psychol. Psychother. 19 , 305–315 (2012).
Sheldon, K. M., Kasser, T., Smith, K. & Share, T. Personal goals and psychological growth: testing an intervention to enhance goal attainment and personality integration. J. Pers. 70 , 5–31 (2002).
Leung, S. S. K. & Lam, T. H. Group antenatal intervention to reduce perinatal stress and depressive symptoms related to intergenerational conflicts: a randomized controlled trial. Int. J. Nurs. Stud. 49 , 1391–1402 (2012).
Elliott, T. R., Brossart, D., Berry, J. W. & Fine, P. R. Problem-solving training via videoconferencing for family caregivers of persons with spinal cord injuries: a randomized controlled trial. Behav. Res. Ther. 46 , 1220–1229 (2008).
Elliott, T. R., Berry, J. W. & Grant, J. S. Problem-solving training for family caregivers of women with disabilities: a randomized clinical trial. Behav. Res. Ther. 47 , 548–558 (2009).
Berry, J. W., Grant, J. S., Elliott, T. R., Edwards, G. & Fine, P. R. Does problem-solving training for family caregivers benefit their care recipients with severe disabilities? A latent growth model of the project clues randomized clinical trial. Rehabil. Psychol. 57 , 98–112 (2012).
Oliver, J. & Macleod, A. K. Working adults’ wellbeing: An online self-help goal-based intervention. J. Occup. Organ. Psychol. 91 , 665–680 (2018).
Roch, R. M., Rosch, A. G. & Schultheiss, O. C. Enhancing congruence between implicit motives and explicit goal commitments: results of a randomized controlled trial. Front. Psychol. 8 , 1540 (2017).
Kenny, R., Fitzgerald, A., Segurado, R. & Dooley, B. Is there an app for that? A cluster randomised controlled trial of a mobile app-based mental health intervention. Health Inform. J. 26 , 1538–1559 (2020).
Crawford, J., Wilhelm, K. & Proudfoot, J. Web-based benefit-finding writing for adults with type 1 or type 2 diabetes: preliminary randomized controlled trial. JMIR Diabetes 4 , e13857 (2019).
Nelson, S. K., Fuller, J. A. K., Choi, I. & Lyubomirsky, S. Beyond self-protection: self-affirmation benefits hedonic and eudaimonic wellbeing. Pers. Soc. Psychol. Bull. 40 , 998–1011 (2014).
Roche, L., Dawson, D. L., Moghaddam, N. G., Abey, A. & Gresswell, D. M. An acceptance and commitment therapy (Act) intervention for chronic fatigue syndrome (CFS): a case series approach. J. Contextual Behav. Sci. 6 , 178–186 (2017).
Lyubomirsky, S. & Lepper, H. S. A measure of subjective happiness: preliminary reliability and construct validation. Soc. Indic. Res. 46 , 137–155 (1999).
Mueller, R. M., Lambert, M. J. & Burlingame, G. M. Construct validity of the outcome questionnaire: A confirmatory factor analysis. J. Pers. Assess. 70 , 248–262 (1998).
Topp, C. W., Østergaard, S. D., Søndergaard, S. & Bech, P. The WHO-5 Wellbeing Index: a systematic review of the literature. Psychother. Psychosom. 84 , 167–176 (2015).
Shepherd, J., Oliver, M. & Schofield, G. Convergent validity and test–retest reliability of the authentic happiness inventory in working adults. Soc. Indic. Res. 124 , 1049–1058 (2015).
Wallace, K. A. & Wheeler, A. J. Reliability generalization of the life satisfaction index. Educ. Psychological Meas. 62 , 674–684 (2002).
Huebner, E. S. Initial development of the student’s life satisfaction scale. Sch. Psychol. Int. 12 , 231–240 (1991).
Seligson, J. L., Huebner, E. S. & Valois, R. F. Preliminary validation of the brief multidimensional students’ life satisfaction scale (BMSLSS). Soc. Indic. Res. 61 , 121–145 (2003).
Moum, T., Næss, S., Sørensen, T., Tambs, K. & Holmen, J. Hypertension labelling, life events and psychological wellbeing. Psychol. Med. 20 , 635–646 (1990).
Cummins, R. A., Eckersley, R., Pallant, J., Van Vugt, J. & Misajon, R. Developing a national index of subjective wellbeing: The Australian Unity Wellbeing Index. Soc. Indic. Res. 64 , 159–190 (2003).
Kammann, R. & Flett, R. Affectometer 2: a scale to measure current level of general happiness. Aust. J. Psychol. 35 , 259–265 (1983).
Campbell, A., Converse, P. & Rodgers, W. The Quality of American Life: Perceptions, Evaluations and Satisfactions (Russell Sage Foundation, 1976).
Post, M. W., van Leeuwen, C. M., van Koppenhagen, C. F. & de Groot, S. Validity of the life satisfaction questions, the life satisfaction questionnaire, and the satisfaction with life scale in persons with spinal cord injury. Arch. Phys. Med. Rehabil. 93 , 1832–1837 (2012).
Fugl-Meyer, A. R., Melin, R. & Fugl-Meyer, K. S. Life satisfaction in 18-to 64-year-old Swedes: in relation to gender, age, partner and immigrant status. J. Rehabil. Med. 34 , 239–246 (2002).
Stones, M. in Encyclopedia of Quality of Life and Wellbeing Research (ed Michalos, A. C.) 3987–3990 (Springer, 2014).
Dambrun, M. et al. Measuring happiness: from fluctuating happiness to authentic-durable happiness. Front. Psychol. 3 , 16–16 (2012).
Nieboer, A., Lindenberg, S., Boomsma, A. & Bruggen, A. C. V. Dimensions of wellbeing and their measurement: the Spf-Il scale. Soc. Indic. Res. 73 , 313–353 (2005).
Gilbert, P. et al. Feeling safe and content: A specific affect regulation system? Relationship to depression, anxiety, stress, and self-criticism. J. Posit. Psychol. 3 , 182–191 (2008).
Chiang, Y. C., Lee, C. Y. & Hsueh, S. C. Happiness or hopelessness in late life: a cluster RCT of the 3L‐Mind‐Training programme among the institutionalized older people. J. Adv. Nurs. 76 , 312–323 (2020).
Cheng, S. T., Mak, E. P. M., Kwok, T., Fung, H. & Lam, L. C. W. Benefit-finding intervention delivered individually to Alzheimer family caregivers: longer-term outcomes of a randomized double-blind controlled trial. J. Gerontol. B 75 , 1884–1893 (2020).
Hills, P. & Argyle, M. The Oxford Happiness Questionnaire: a compact scale for the measurement of psychological wellbeing. Pers. Individ. Differ. 33 , 1073–1082 (2002).
Diener, E. et al. New wellbeing measures: short scales to assess flourishing and positive and negative feelings. Soc. Indic. Res. 97 , 143–156 (2010).
De Beni, R., Borella, E., Carretti, B., Marigo, C. & Nava, L. Portfolio per la Valutazione del Benessere e delle Abilità Cognitive Nell’età Adulta e Avanzata (Giunti, OS, 2008).
Waterman, A. S. et al. The questionnaire for eudaimonic wellbeing: psychometric properties, demographic comparisons, and evidence of validity. J. Posit. Psychol. 5 , 41–61 (2010).
Watson, D. & Clark, L. A. The PANAS-X: Manual for the Positive and Negative Affect Schedule-Expanded Form (Univ. Iowa, 1999).
Laurent, J. et al. A measure of positive and negative affect for children: scale development and preliminary validation. Psychological Assess. 11 , 326 (1999).
Boyle, G. J. Reliability and validity of Izard’s differential emotions scale. Pers. Individ. Differ. 5 , 747–750 (1984).
Cohn, M. A., Fredrickson, B. L., Brown, S. L., Mikels, J. A. & Conway, A. M. Happiness unpacked: positive emotions increase life satisfaction by building resilience. Emotion 9 , 361 (2009).
Bradburn, N. M. The Structure of Psychological Wellbeing (Aldine, 1969).
Derogatis, L. The Affects Balance Scale (Clinical Psychometric Research, 1975).
Mroczek, D. K. & Kolarz, C. M. The effect of age on positive and negative affect: a developmental perspective on happiness. J. Pers. Soc. Psychol. 75 , 1333–1349 (1998).
Mayer, J. D. & Gaschke, Y. N. The experience and meta-experience of mood. J. Pers. Soc. Psychol. 55 , 102–111 (1988).
Cheng, S.-T. Age and subjective wellbeing revisited: a discrepancy perspective. Psychol. Aging 19 , 409–415 (2004).
Steyer, R., Schwenkmezger, P., Notz, P. & Eid, M. Testtheoretische analysen des mehrdimensionalen befindlichkeitsfragebogen (MDBF). Diagnostica 40 , 320–328 (1994).
Diener, E. & Emmons, R. A. The independence of positive and negative affect. J. Pers. Soc. Psychol. 47 , 1105 (1984).
Denollet, J. Emotional distress and fatigue in coronary heart disease: the Global Mood Scale (GMS). Psycholog. Med. 23 , 111–111 (1993).
Bradley, C. Handbook of Psychology and Diabetes: A Guide to Psychological Measurement in Diabetes Research and Practice (Harwood Academic Publishers, 1994).
Lamers, S. M. A., Westerhof, G. J., Bohlmeijer, E. T., ten Klooster, P. M. & Keyes, C. L. M. Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF). J. Clin. Psychol. 67 , 99–110 (2011).
Bisseling, E. et al. Development of the therapeutic alliance and its association with internet-based mindfulness-based cognitive therapy for distressed cancer patients: secondary analysis of a multicenter randomized controlled trial. J. Med. Internet Res. 21 , e14065 (2019).
Su, R., Tay, L. & Diener, E. The development and validation of the Comprehensive Inventory of Thriving (CIT) and the Brief Inventory of Thriving (BIT). Appl. Psychol. Health Well Being 6 , 251–279 (2014).
Hervas, G. & Vazquez, C. Construction and validation of a measure of integrative wellbeing in seven languages: The Pemberton Happiness Index. Health Qual. Life Outcomes 11 , 66 (2013).
Massé, R. et al. Elaboration and validation of a tool to measure psychological wellbeing: WBMMS. Can. J. Public Health 89 , 352–357 (1998).
Shah, N. & Stewart-Brown, S. The Warwick–Edinburgh Mental Wellbeing Scale: role and impact on public health policy and practice. Eur. J. Public Health https://doi.org/10.1093/eurpub/ckx186.237 (2017).
Stewart-Brown, S. et al. Internal construct validity of the Warwick–Edinburgh mental wellbeing scale (WEMWBS): a Rasch analysis using data from the Scottish health education population survey. Health Qual. Life Outcomes 7 , 15 (2009).
Butler, J. & Kern, M. L. The PERMA-Profiler: a brief multidimensional measure of flourishing. Int. J. Wellbeing 6 , 1–48 (2016).
Kokko, K., Korkalainen, A., Lyyra, A.-L. & Feldt, T. Structure and continuity of wellbeing in mid-adulthood: a longitudinal study. J. Happiness Stud. 14 , 99–114 (2013).
Download references
Acknowledgements
The authors thank colleagues at the South Australian Health and Medical Research Institute, Wellbeing and Resilience Centre, for their support during the creation of this review, S. Brown and N. May, for their help in crafting the search strategy. This work was supported by a grant by the James and Diana Ramsay Foundation. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Author information
Authors and affiliations.
Wellbeing and Resilience Centre, Lifelong Health Theme, South Australian Health and Medical Research Institute, Adelaide, South Australia, Australia
Joep van Agteren, Matthew Iasiello, Laura Lo, Jonathan Bartholomaeus, Marissa Carey & Michael Kyrios
Órama Institute for Mental Health and Wellbeing, Flinders University, Adelaide, South Australia, Australia
Joep van Agteren, Matthew Iasiello & Michael Kyrios
College of Nursing and Health Sciences, Flinders University, Adelaide, South Australia, Australia
Matthew Iasiello
School of Psychology, The University of Adelaide, Adelaide, South Australia, Australia
Jonathan Bartholomaeus
Registry of Senior Australians (ROSA), South Australian Health and Medical Research Institute, Adelaide, South Australia, Australia
Australian Centre for Precision Health, Division of Health Sciences, University of South Australia, Adelaide, South Australia, Australia
Zoe Kopsaftis
Respiratory Medicine Unit, The Queen Elizabeth Hospital, Central Adelaide Local Health Network, Woodville South, South Australia, Australia
Faculty of Health and Medical Sciences, The University of Adelaide, Adelaide, South Australia, Australia
College of Education, Psychology and Social Work, Flinders University, Adelaide, South Australia, Australia
Michael Kyrios
You can also search for this author in PubMed Google Scholar
Contributions
J.v.A.: review methodology, screening of literature, data extraction, risk of bias, meta-analysis and writing. M.I.: review methodology, screening of literature, data extraction, risk of bias and writing. L.L.: screening of literature, data extraction, risk of bias and writing. J.B.: data extraction, risk of bias and writing. Z.K.: risk of bias and writing. M.C.: data extraction and writing. M.K.: input into methodology, focus of review and writing.
Corresponding author
Correspondence to Joep van Agteren .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Peer review information Nature Human Behaviour thanks Pete Harris, Laura Anne Weiss and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information.
Supplementary Tables 1–7 and Supplementary Figs. 1–4.
Reporting Summary
Peer review information, rights and permissions.
Reprints and permissions
About this article
Cite this article.
van Agteren, J., Iasiello, M., Lo, L. et al. A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nat Hum Behav 5 , 631–652 (2021). https://doi.org/10.1038/s41562-021-01093-w
Download citation
Received : 06 January 2020
Accepted : 05 March 2021
Published : 19 April 2021
Issue Date : May 2021
DOI : https://doi.org/10.1038/s41562-021-01093-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Psychological capital educational program and its effect on nurse interns’ innovative behavior.
- Ahmed Hussien Ahmed Kotb
- Mona Mostafa Shazly
- Hemat Abdel-Azeem Mostafa
BMC Nursing (2024)
Distinct associations between gratitude, self-esteem, and optimism with subjective and psychological well-being among Japanese individuals
- Norberto Eiji Nawa
- Noriko Yamagishi
BMC Psychology (2024)
Enhancing mental wellbeing by changing mindsets? Results from two randomized controlled trials
- Carina Schreiber
- Marijke Schotanus-Dijkstra
Positive affect and reward processing in the treatment of depression, anxiety and trauma
- Michelle G. Craske
- Barnaby D. Dunn
- Charles T. Taylor
Nature Reviews Psychology (2024)
The process and mechanisms of personality change
- Joshua J. Jackson
- Amanda J. Wright
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

IMAGES
COMMENTS
The most recent definition comprises four broad domains aligned with current definitions of health literacy: ‘1) understanding how to obtain and maintain positive mental health; 2) understanding mental disorders and their treatments; 3) decreasing stigma related to mental disorders, and 4) enhancing help-seeking efficacy (knowing when and ...
This scoping review summarizes the existing literature regarding the mental health of physicians and physicians-in-training and explores what types of mental health concerns are discussed in the literature, what is their prevalence among physicians, what are the causes of mental health concerns in physicians, what effects mental health concerns ...
The aim of this paper is to provide a systematic review of evidence for positive effects in children and adolescents' mental health resulting from interventions conducted in schools and communities in which interaction among different agents is an integral component.
One particular body of work has focused on ‘mental health literacy’ (MHL) defined as knowledge about mental health disorders that are associated with their recognition, management, and...
The primary aim of this literature review: to address the aforementioned challenges, we have synthesized recent research on the biological, psychological, and social deter-minants of depression and we have reviewed research from fields including genetics, immunology, neurology, psychology, public health, and epidemiology, among others.
Mental disorders are a significant contributor to disease burden. However, there is a large treatment gap for common mental disorders worldwide. This systematic review summarizes the factors associated with mental health service use.
To review the relationship between mental health and lost productivity and undertake a critical review of the published literature. Methods.
This is an overall review on mindfulness-based interventions (MBIs). We identified studies in PubMed, EMBASE, CINAHL, PsycINFO, AMED, Web of Science and Google Scholar using keywords including ‘mindfulness’, ‘meditation’, and ‘review’, ...
Abstract. Background. Mental health and mental illness have been contested concepts for decades, with a wide variety of models being proposed. To date, there has been no exhaustive review that provides an overview of existing models. Aim. To conduct a quasi-systematic review of theoretical models of mental health problems. Methods.
This systematic review and meta-analysis aimed to create a clear synthesis of the impact of different types of psychological interventions on mental wellbeing, irrespective of their theoretical...