Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.

Healthy Eating Learning Opportunities and Nutrition Education

Healthy eating learning opportunities includes nutrition education and other activities integrated into the school day that can give children knowledge and skills to help choose and consume healthy foods and beverages. 1 Nutrition education is a vital part of a comprehensive health education program and empowers children with knowledge and skills to make healthy food and beverage choices. 2-8
US students receive less than 8 hours of required nutrition education each school year, 9 far below the 40 to 50 hours that are needed to affect behavior change. 10,11 Additionally, the percentage of schools providing required instruction on nutrition and dietary behaviors decreased from 84.6% to 74.1% between 2000 and 2014. 9
Given the important role that diet plays in preventing chronic diseases and supporting good health, schools would ideally provide students with more hours of nutrition education instruction and engage teachers and parents in nutrition education activities. 5, 12 Research shows that nutrition education can teach students to recognize how healthy diet influences emotional well-being and how emotions may influence eating habits. However, because schools face many demands, school staff can consider ways to add nutrition education into the existing schedule. 11
Nutrition education can be incorporated throughout the school day and in various locations within a school. This provides flexibility allowing schools to use strategies that work with their settings, daily schedule, and resources.
In the Classroom
Nutrition education can take place in the classroom, either through a stand-alone health education class or combined into other subjects including 2,5 :
- Counting with pictures of fruits and vegetables.
- Learning fractions by measuring ingredients for a recipe.
- Examining how plants grow.
- Learning about cultural food traditions.
Nutrition education should align with the National Health Education Standards and incorporate the characteristics of an effective health education curriculum .

Farm to School
Farm-to-school programs vary in each school or district, but often include one or more of the following strategies:
- Purchasing and serving local or regionally produced foods in the school meal programs.
- Educating students about agriculture, food, health, and nutrition.
- Engaging students in hands-on learning opportunities through gardening, cooking lessons, or farm field trips.
Students who participate in farm-to-school activities have increased knowledge about nutrition and agriculture, are more willing to try new foods, and consume more fruits and vegetables. 14-17

School Gardens
School garden programs can increase students’ nutrition knowledge, willingness to try fruit and vegetables, and positive attitudes about fruits and vegetables. 18-22 School gardens vary in size and purpose. Schools may have window sill gardens, raised beds, greenhouses, or planted fields.
Students can prepare the soil for the garden, plant seeds, harvest the fruits and vegetables, and taste the food from the garden. Produce from school gardens can be incorporated into school meals or taste tests. Classroom teachers can teach lessons in math, science, history, and language arts using the school garden.

In the Cafeteria
Cafeterias are learning labs where students are exposed to new foods through the school meal program, see what balanced meals look like, and may be encouraged to try new foods through verbal prompts from school nutrition staff, 23 or taste tests. 24-25 Cafeterias may also be decorated with nutrition promotion posters or student artwork promoting healthy eating. 24
Other Opportunities
Schools can add messages about nutrition and healthy eating into the following:
- Morning announcements.
- School assemblies.
- Materials sent home to parents and guardians. 24
- Staff meetings.
- Parent-teacher group meetings.
These strategies can help reinforce messages about good nutrition and help ensure that students see and hear consistent information about healthy eating across the school campus and at home. 2
Shared use agreements can extend healthy eating learning opportunities. As an example, an after-school STEM club could gain access to school gardens as learning labs.
CDC Parents for Healthy Schools: Ideas for Parents
Nutrition: Gardening Interventions | The Community Guide
Dietary Guidelines for Americans, 2020–2025
Introduction to School Gardens
Learning Through the Garden
National Farm-to-School Network
National Farm to School Network Resource Database
National Health Education Standards
Team Nutrition Curricula
USDA Farm to School
USDA Team Nutrition
- Centers for Disease Control and Prevention. School health guidelines to promote healthy eating and physical activity. MMWR Morb Mortal Wkly Rep . 2011;60(RR-5):1–76.
- Joint Committee on National Health Education Standards. National Health Education Standards: Achieving Excellence. 2nd ed. Atlanta, GA: American Cancer Society; 2007.
- Centers for Disease Control and Prevention. Health Education Curriculum Analysis Tool, 2012, Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2012. Available at http://www.cdc.gov/healthyyouth/hecat/index.htm. Accessed April 9, 2019.
- Price C, Cohen D, Pribis P, Cerami J. Nutrition education and body mass index in grades K–12: a systematic review. J Sch Health. 2017;87:715–720.
- Meiklejohn S, Ryan L, Palermo C. A systematic review of the impact of multi-strategy nutrition education programs on health and nutrition of adolescents. J Nutr Educ Behav . 2016;48:631–646.
- Silveira JA, Taddei JA, Guerra PH, Nobre MR. The effect of participation in school-based nutrition education interventions on body mass index: A meta-analysis of randomized controlled community trials. Prev Med . 2013;56:237–243.
- County Health Rankings and Roadmaps. School-based Nutrition Education Programs website. http://www.countyhealthrankings.org/take-action-to-improve-health/what-works-for-health/policies/school-based-nutrition-education-programs . Accessed on April 9, 2019.
- Results from the School Health Policies and Practices Study 2014 . Atlanta, GA: Centers for Disease Control and Prevention; 2014.
- Connell DB, Turner RR, Mason EF. Results of the school health education evaluation: health promotion effectiveness, implementation, and costs . J Sch Health . 1985;55(8):316–321.
- Institute of Medicine. Nutrition Education in the K–12 Curriculum: The Role of National Standards: Workshop Summary. Washington, DC: The National Academies Press; 2014.
- Murimi MW, Moyeda-Carabaza AF, Nguyen B, Saha S, Amin R, Njike V. Factors that contribute to effective nutrition education interventions in children: a systematic review. Nutr Rev . 2018;76(8):553–580.
- Hayes D, Contento IR, Weekly C. Position of the American Dietetic Association, School Nutrition Association, and Society for Nutrition Education: comprehensive school nutrition services. J Acad Nutr Diet . 2018; 118:913–919.
- Joshi A, Misako Azuma A, Feenstra G. Do farm-to-school programs make a difference? Findings and future research needs . J Hunger Environ Nutr . 2008;3:229–246.
- Moss A, Smith S, Null D, Long Roth S, Tragoudas U. Farm to school and nutrition education: Positively affecting elementary school-aged children’s nutrition knowledge and consumption behavior. Child Obes . 2013;9(1):51–6.
- Bontrager Yoder AB, Liebhart JL, McCarty DJ, Meinen A, Schoeller D, Vargas C, LaRowe T. Farm to elementary school programming increases access to fruits and vegetables and increases their consumption among those with low intake . J Nutr Educ Behav . 2014;46(5):341–9.
- The National Farm to School Network. The Benefits of Farm to School website. http://www.farmtoschool.org/Resources/BenefitsFactSheet.pdf . Accessed on June 14, 2019.
- Berezowitz CK, Bontrager Yoder AB, Schoeller DA. School gardens enhance academic performance and dietary outcomes in children. J Sch Health . 2015;85:508–518.
- Davis JN, Spaniol MR, Somerset S. Sustenance and sustainability: maximizing the impact of school gardens on health outcomes. Public Health Nutr . 2014;18(13):2358–2367.
- Langellotto GA, Gupta A. Gardening increases vegetable consumption in school-aged children: A meta-analytical synthesis. Horttechnology . 2012;22(4):430–445.
- Community Preventative Services Task Force. Nutrition: Gardening Interventions to Increase Fruit and Vegetable Consumption Among Children. Finding and Rationale Statement .. https://www.thecommunityguide.org/sites/default/files/assets/Nutrition-Gardening-Fruit-Vegetable-Consumption-Children-508.pdf . Accessed on May 16, 2019.
- Savoie-Roskos MR, Wengreen H, Durward C. Increasing Fruit and Vegetable Intake among Children and Youth through Gardening-Based Interventions: A Systematic Review. Journal of the Academy of Nutrition and Dietetics 2017;11(2):240–50.
- Schwartz M. The influence of a verbal prompt on school lunch fruit consumption: a pilot study. Int J Behav Nutr Phys Act. 2007;4:6.
- Fulkerson JA, French SA, Story M, Nelson H, Hannan PJ. Promotions to increase lower-fat food choices among students in secondary schools: description and outcomes of TACOS (Trying Alternative Cafeteria Options in Schools). Public Health Nutr. 2003 ;7(5):665–674.
- Action for Healthy Kids. Tips for Hosting a Successful Taste Test website. http://www.actionforhealthykids.org/tools-for-schools/find-challenges/classroom-challenges/701-tips-for-hosting-a-successful-taste-test . Accessed on May 19, 2019.

Healthy Youth
To receive email updates about this page, enter your email address:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Prev Med Rep
- v.20; 2020 Dec
The effect of teacher-delivered nutrition education programs on elementary-aged students: An updated systematic review and meta-analysis
Wayne cotton.
a The University of Sydney, NSW 2006, Australia
Dean Dudley
b Macquarie University, NSW, Australia
Louisa Peralta
Thea werkhoven.
Research shows that schools can make a positive impact on children’s nutritional outcomes. However, it is also reported that schools and teaching staff note many barriers, which may restrict nutritional education programming and delivery. This is concerning, considering the view that teachers are the key agents for promoting health and nutrition within schools. The purpose of the updated systematic review and meta-analysis was to ascertain the impact that nutrition education programs have on elementary-aged students’ energy intake, fruit, vegetable, sugar consumption and nutritional knowledge. A systematic literature search was conducted using electronic databases (The Cochrane Central Register of Controlled Trials (CENTRAL); A + Education; ERIC; PsycINFO; MEDLINE; ProQuest Central, Journals@Ovid and SAGE Health Sciences Full-Text Collection) from 1990 to 31st October 2018. This process yielded 34 studies for inclusion in this systematic review and meta-analysis. Of these studies, seven studies had a focus on energy intake, five had a focus on sugar consumption, 21 of the studies looked at fruit and vegetable consumption and 13 studies focused on nutritional knowledge. The results suggest that the teaching of nutrition education in elementary schools by qualified teachers can make an important contribution to the knowledge and dietary habits of children. The small and medium effect sizes indicate that prudent, evidence-based decisions need to be made by policy makers and pedagogues as to the teaching strategies employed when delivering nutrition education programs to elementary-aged students.
The review is reported in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (van Sluijs et al., 2007).
1. Introduction
Nutrition‐related health conditions, such as obesity, Type 2 diabetes, and hypertension are becoming prevalent in children ( Goran et al., 2003 , Kelsey et al., 2014 ). Children with these conditions often suffer physical discomfort, ill-health, lower self‐esteem, poorer academic outcomes and negative socio-emotional ( van Geel et al., 2014 , Reilly and Kelly, 2011 ). Furthermore, the risk of these conditions tracking into adulthood is high ( United Nations Educational Scientific and Cultural Organization, 2013 ). As such, there have been international calls to focus on prevention through nutrition education in schools ( World Health Organization, 2012 , Story et al., 2009 ). Schools are ideal settings for preventive nutrition education efforts targeting children due to their reach, structure and cost effectiveness ( Graziose et al., 2017 , Dudley et al., 2015 ). Two recent systematic reviews and meta-analysis suggests nutrition education programs delivered in elementary schools can positively influence children's energy intake, fruit and vegetable consumption, sugar consumption and nutritional knowledge, particularly those programs embedding experiential learning strategies and cross-curricular approaches, engaging parents by means of face-to-face sessions and assuring fidelity by training teachers or recruiting trained experts to support the delivery of the intervention ( Murimi et al., 2018 , Peralta et al., 2016 ).
Despite research showing that schools can make a positive impact on children’s nutritional outcomes, it is also reported that schools and teaching staff note many barriers that restrict nutritional education programming and delivery. First, nutrition education is often seen as unnecessary because the content is not included on standardized tests. Second, elementary school teaching staff do not have access to appropriate resources and may not have the expertise, motivation or capacity to deliver evidence-based nutrition education ( Dudley et al., 2015 ). Third, preservice teachers only receive limited training in nutrition education during their tertiary studies ( de Vlieger et al., 2019 ). Finally, providing professional learning for teachers is time consuming and often requires financial investment that may not align with the school’s professional learning goals ( Porter et al., 2018 ). To overcome these barriers, schools and teachers have sought community organizations, who are experts in nutrition education, to deliver nutrition education programs in elementary schools ( Moher et al., 2009 ). This is concerning, considering the educative view that qualified teachers are the key agents for promoting health and nutrition within schools ( World Health Organization, 2012 ).
To emphasise the importance and effect of elementary school nutrition education programs on children’s energy intake, fruit, vegetable and sugar consumption and nutritional knowledge, and to capture the exponential growth of studies reporting on elementary school nutrition education programs in the previous five years, an updated systematic review and meta-analysis was undertaken ( Murimi et al., 2018 ). The purpose of the updated systematic review and meta-analysis was to ascertain the impact that nutrition education programs have on elementary-aged students’ energy intake, fruit, vegetable, sugar consumption and nutritional knowledge by widening the search through increasing the number of inclusion criteria and reviewing data from more recent studies.
2. Materials and methods
A systematic literature search was conducted using electronic databases (The Cochrane Central Register of Controlled Trials (CENTRAL); A+ Education; ERIC; PsycINFO; MEDLINE; ProQuest Central, Journals@Ovid and SAGE Health Sciences Full-Text Collection) from 1990 to 31st October 2018.
The search strategy included the use of terms in four broad categories: (i) participants; (ii) delivery; (iii) strategies; and (iv) design. The title and abstract fields were searched using the following terms:
- 1. primary student* or primary school* or elementary student* or elementary school* or child* or school-based* and
- 2. teach* or class* or health educ* or nutrition educ* or healthy eat* or curricul* or reward* or nutritional intervention or education program* and
- 3. nutrition* or energy or cook* or food* or fruit* or vegetable* or sugar* or kilojoule* or calorie* or eating or diet* and
- 4. test or RCT or randomi* or control or trial or evaluat* or quasi-exper* or cluster or intervention*.
Reference lists of included studies were manually searched for additional articles.
2.1. Inclusion and exclusion criteria
Studies were included if they: (1) targeted elementary-aged children’s nutritional consumption or knowledge; (2) employed a nutritional education program taught by an elementary school teacher; and (3) reported nutritional consumption and/or knowledge outcomes using independent group difference values.
2.2. Study selection, data extraction and analysis
After duplicate deletion, one author (TW) initially screened all articles based on title and abstracts for preliminary inclusion (Stage 1); before screening remaining articles by full text based on inclusion criteria (Stage 2). In cases where there was uncertainty, a second reviewer (DD) assessed the article and consensus was reached by discussion. See Fig. 1 for an overview of this process.

Flow of information through the different phases of the systematic review.
The standardised mean difference score was calculated for each stated variable by using Cohen’s d. The pooled ES was estimated by using a random-effects model based on the DerSimonian and Laird ( van Sluijs et al., 2007 ) method. We assessed and reported heterogeneity across studies by using the following statistical analyses. 1. The Q-statistic provided a test of the null hypothesis as to whether all studies share a common effect size; 2.the I 2 statistic reports the proportion of the observed variance that are indicative of changes in true effect sizes rather than sampling error; 3.T 2 is the variance of true effect sizes; and 4. Prediction interval is range of true effect size for 95% of all samples observed.
Classic Fail Safe N and Trim and Fill ( Collaboration and Fail-safe, 2011 ) methods were used to assess publication bias. Studies were only included in the meta-analysis if they provided complete data for pre- and post-intervention measurements and included a control or comparison group.
In addition, the following statistical assumptions were applied: (1) when two cohorts were included in studies, their data were investigated as combined samples; (2) when two or more tests measuring the same variable were included in the studies, the combined effect size at the study level was used; (3) when two or more learning outcomes were used, the results were treated as independent samples; and (4) when two or more follow-up measurements were reported, only the last measurement was considered.
Comprehensive Meta-Analysis software, version 3 (Biostat, New York, NY) was used to perform all Statistical analyses.
2.3. Data collection process and data items
Characteristics and results of studies were extracted by all authors. Studies with multiple published articles were reported as a single group. For meta-analysis, final mean and standard deviation (SD) or change in mean and SD were extracted energy intake, sugar consumption, fruit and vegetable consumption and nutritional knowledge. In some studies, the required statistics for meta-analysis were not reported. If available, other statistics e.g., 95% confidence interval (CI) or standard error (SE) were converted to the required form according to the calculations outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Section 7.7 and 16.1.3.2) ( DerSimonian and Laird, 1986 ).
2.4. Quality assessment
The methodological quality of the individual studies were assessed using an assessment scale derived from van Sluijs and colleagues ( van Sluijs et al., 2007 ) (See Table 1 ). For each included article, three reviewers (WC, LP & TW) independently assessed whether the assessed item was present or if the assessed item was absent. If an item was not described sufficiently it was allocated an absent score. For each article, agreement between reviewers for each article was set a priori at 80% ( DerSimonian and Laird, 1986 ) (i.e., reviewers were required to agree that the items were either present or absent for eight of the 10 items). If this did not occur, further discussions were conducted until consensus was reached.
Methodological quality assessment items (Adapted from ( van Sluijs et al., 2007 ).
| A | Key baseline characteristics are presented separately for treatment groups (age, and one relevant outcome (food consumption/energy intake; fruit and vegetable consumption or preference; reduced sugar consumption or preference; nutritional knowledge) and for randomised controlled trials and controlled trials, positive if baseline outcomes were statistically tested and results of tests were provided. |
| B | Randomisation procedure clearly and explicitly described and adequately carried out (generation of allocation sequence, allocation concealment and implementation) |
| C | Validated measures of food consumption/energy intake and/or fruit and vegetable consumption or preference and/or reduced sugar consumption or preference and/or nutritional knowledge (validation in same age group reported and/or cited) |
| D | Drop out reported and ≤20% for <6-month follow-up or ≤30% for ≥6-month follow-up |
| E | Blinded outcome variable assessments |
| F | Food consumption/energy intake and/or fruit and vegetable consumption or preference and/or reduced sugar consumption or preference and/or nutritional knowledge assessed a minimum of 6 months after pre-test |
| G | Intention to treat analysis for food consumption/energy intake and/or fruit and vegetable consumption or preference and/or reduced sugar consumption or preference and/or nutritional knowledge outcomes(s) (participants analysed in group they were originally allocated to, and participants not excluded from analyses because of non-compliance to treatment or because of some missing data) |
| H | Potential confounders accounted for in outcome analysis (e.g. baseline score, group/cluster, age) |
| I | Summary results for each group + treatment effect (difference between groups) + its precision (e.g. 95% confidence interval) |
| J | Power calculation reported, and the study was adequately powered to detect hypothesized relationships |
The standardized effect sizes ( Cohen, 1988 ) were interpreted as minimal (<0.02), small (0.2), medium (0.5), and large (0.8).
The combined search retrieved 5257 peer-reviewed articles published in English from the 1st January 1990 to the 31st October 2018. After removing duplicates, 3922 individual articles were ready for the initial review. Decisions were made about the inclusion of articles in two stages. In Stage 1, one author (TW) scanned the titles and abstracts for relevance (i.e., did they have a nutrition education focus in elementary schools).
This resulted in a subgroup of 280 remaining articles. In Stage 2, three authors (TW, LP & WC) conducted full text reviews of remaining articles, including reference lists. This process yielded 34 studies for final inclusion in this systematic review and meta-analysis. Of these 34 studies, seven studies had a focus on energy intake, five had a focus on sugar consumption, 21 of the studies looked at fruit and vegetable consumption and 13 studies focused on nutritional knowledge.
Fig. 1 shows a diagrammatic overview of the review process.
An overview of methodological quality of the studies are reported in Table 2 .
Methodological quality assessment.
| Paper Author (Year) | Methodological Quality Assessment Items | No. of criteria met | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | G | H | I | J | ||
| √ | x | x | √ | x | √ | x | √ | √ | √ | 6 | |
| √ | x | x | x | x | √ | x | x | √ | x | 3 | |
| √ | x | √ | x | x | √ | x | √ | √ | x | 5 | |
| √ | x | √ | √ | x | √ | x | √ | √ | √ | 7 | |
| √ | x | √ | √ | x | √ | √ | √ | √ | x | 7 | |
| √ | x | √ | x | x | √ | x | √ | √ | x | 5 | |
| x | x | √ | x | x | x | x | x | √ | x | 2 | |
| √ | x | x | √ | x | x | x | x | √ | √ | 4 | |
| √ | x | √ | √ | x | x | x | √ | √ | x | 5 | |
| √ | √ | √ | √ | x | x | x | √ | √ | √ | 7 | |
| √ | x | √ | x | x | x | x | x | x | x | 2 | |
| √ | √ | √ | x | x | √ | x | √ | √ | √ | 7 | |
| √ | x | √ | √ | x | x | x | x | √ | x | 4 | |
| √ | √ | √ | x | x | x | x | x | √ | x | 4 | |
| √ | x | x | √ | √ | √ | x | √ | √ | √ | 7 | |
| √ | √ | √ | x | x | √ | √ | x | √ | x | 6 | |
| √ | x | √ | x | x | x | x | x | √ | x | 3 | |
| √ | x | √ | x | x | x | x | x | √ | x | 3 | |
| √ | x | √ | x | x | x | √ | √ | x | x | 4 | |
| √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | 10 | |
| √ | x | x | √ | x | √ | x | √ | √ | x | 5 | |
| √ | x | √ | √ | x | x | √ | √ | √ | x | 6 | |
| x | x | √ | x | x | √ | x | x | x | x | 2 | |
| √ | x | √ | √ | x | √ | x | √ | √ | x | 6 | |
| √ | x | x | x | x | x | x | x | √ | x | 2 | |
| √ | x | √ | √ | x | √ | x | √ | √ | √ | 7 | |
| √ | x | x | x | x | √ | x | √ | √ | x | 4 | |
| √ | √ | √ | x | x | x | x | x | √ | x | 4 | |
| √ | √ | √ | √ | √ | x | x | x | √ | √ | 7 | |
| √ | √ | √ | √ | x | x | √ | x | √ | x | 6 | |
| √ | x | x | x | x | √ | x | x | x | x | 2 | |
| √ | x | √ | x | x | x | x | √ | √ | √ | 5 | |
| √ | √ | √ | √ | x | x | √ | x | √ | √ | 7 | |
| √ | √ | √ | x | x | √ | x | x | √ | √ | 6 | |
| Percentage/Mean | 94% | 29% | 76% | 47% | 9% | 50% | 21% | 50% | 88% | 35% | 5 |
(N.B. √ = criteria met; x = criteria not met).
Results of the included studies are reported in Table 3 .
An overview of the studies found in the systematic review and included in the meta-analysis.
| Author (Year), Country, Funding agency | Design/Dominant Theory Framework* | Sample | Treatment Length | Teaching Strategy/Approach | Relevant Outcome Categories | Statistical Significance (p /95% CI) |
|---|---|---|---|---|---|---|
| , Italy, Amici di Raoul Follereau (AIFO) | CT / NR | 241 × students Mean age: 12yrs | 24 weeks | Kalèdo Board Game (15-30mins play time p/w) | Nutritional knowledge (31 items) BMI (z-score) | <0.05 NS |
| , UK, Food Standards Agency | CT / TPB | 129 × Grades 1–6 students Mean age: 8yrs | 36 weeks | (Curriculum approach) based on experiential learning, video & literary abstraction Marketing and canteen provisions | - Diet heart disease knowledge - Preference for HFSS foods - FV consumption (g) - Energy (kJ) - Sucrose (g) | 0.001 0.034 0.617 0.327 0.578 |
| , USA, Kraft Foods, Inc., USDA Food and Consumer Services Cooperative, National Institute of Health/Centers for Disease Control and Prevention 5 A Day Evaluation Grant, and The Lindsay Trust. | QE / SCT | 760 students in grades 2–4. Mean age: NR | 16 weekly sessions | (Curriculum approach) Nutrition education sessions | -Fruits -Vegetables -Fruits -Vegetables -FV -School lunches -Wholegrains | < 0.001 < 0.05 < 0.05 < 0.01 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 |
| Baronowski et al. (2000), USA, NR. | RCT / SCT | 1172 children in grades 3–5. Mean age: NR | 6 weeks with 12 sessions | (Curriculum approach) Nutrition education sessions. Videotapes, point of purchase education | Vegetables intake -FVJ eaten at weekday lunch -Knowledge of FVJ | < 0.05 < 0.01 < 0.10 < 0.05 < 0.10 |
| , The Netherlands, Ministry of Economic Affairs of the Netherlands. | QE / NR | 1183 children aged between 9 and 12 years. Mean age: 9yrs. | 10–12 sessions | (Curriculum design) nutrition education Experiential Learning (cooking and tasting food) | Number of foods known -Positive taste -Number of foods tasted -Willingness to taste food -Knowledge -Awareness -Attitude | < 0.05 NS < 0.05 NS < 0.01 NS NS |
| Bere et al. (2006), Norway, Norwegian Research Council. | CT / SCT | 369 × Grade 6 students Mean age: 11yrs | 28 weeks | (Curriculum approach) Experiential learning (Cooking/Food Prep) | - FV consumption (Servings per day) Curriculum enjoyment (Likert scale) | 0.41 0.004 |
| Campbell et al. ( ), Canada, the Provincial Health Service Authority (PHSA) and by the Child and Family Research Institute (CFRI). | RCT / NR | 873 students in grades 3–7. Mean age NR | 21 lessons spanning 1 year | (Curriculum design) nutrition education, peer to peer instruction | -Grades K to 3 -Grades 4 to 7 -Grades K to 3 -Grades 4 to 7 -Grades K to 3 -Grades 4 to 7 | < 0.001 NS < 0.001 < 0.001 < 0.001 < 0.001 |
| , UK, Medical Research Council National Prevention Research Initiative | CT / mixed | 442 × Kindergarten students Mean age: 6yrs | 2 weeks | Contingent reinforcement for vegetable tasting | Liking of vegetables (Likert scale) Intake of vegetables | 0.001 0.001 |
| Day et al. ( ), Canada, NR | CT / NR | 444 × Grades 4–5 students Mean age: 10yrs | 12 weeks | Integrates classroom learning, environmental change strategies, and a family/community component to promote the consumption of FV | - Fruit consumption (Servings) - Vegetable consumption (Servings) - F V consumption (Servings) - Variety of FV consumption (Servings) | <0.05 NS <0.05 <0.05 |
| Evans et al. ( ), UK, NR. | Meta-analysis / NR | Trials of children aged 5 to 11 years. Mean age NR | NR | NR | Fruit portions -Vegetable portions | Significant Significant |
| Fahlman et al. ( ) USA, NR | QE / NR | 576 × students Mean age: 12yrs | 4 weeks | (Curriculum approach) adapted Health Belief Model | - Grain consumption (Servings/day) - Fruit consumption(Servings/day) - Vegetable consumption(Servings/day) - Dairy consumption (Servings/day) - Meat consumption (Servings/day) - Eat more FV - Eat less fat - Drink less SLB - Eat healthy at FF restaurants | NS 0.047 0.018 NS NS NS NS NS NS |
| Francis et al. ( ) Trinidad & Tobago, Self-funded | RCT / NS | 579 × Grade 6 students Mean age: 10yrs | 32 weeks | (Curriculum approach) Bloom’s mastery learning model | Children’s Eating Attitude Test-26 (M) SLB consumption (Servings/wk) Fried food consumption (Servings/day) HFSS food consumption (<502 kJ/day) | <0.05 NS 0.04 NS |
| Friel et al. ( ), Ireland, the Department of Health. | QE / SLT | 821 children aged 8–10 years. Mean age NR | 20 sessions over 10 weeks | (Curriculum approach) Worksheets, homework tasks. Aerobic exercise regimen. | | < 0.01 < 0.01 NS |
| Gatto et al. ( ), USA, The NIH and a Community Benefit grant from the Keck School of Medicine. | RCT / Self-Efficacy | 375 elementary school students. Mean age: 9yrs | 12x weekly sessions of 90 min | School gardening and cooking lessons | -Fruit -Vegetables | <0.05 NS |
| Gibbs et al. ( ), Australia, NR | CT / mixed | 764 × Grades 3 to 6: Mean age: NR | 2 years | (Curriculum approach) Stephanie Alexander’s Kitchen Garden Program. Experiential (gardening and cooking classes) | - Fruit consumption /d - Vegetable consumption /d | 0.11 0.59 |
| Gortmaker et al. ( ), USA, Walton Family Foundation. | QE / SCT BCT | 336 × Grades 4–5 students. Mean age: 9yrs | 2 years | Cross-curricular (Math, science, language, social studies, physical education) coupled with a Social Marketing Approach | - Energy from fat (%) - FV consumption (Servings/4184 kJ) | 0.04 0.01 |
| Govula et al. ( ), USA, NR | QE / NR | 33 × Grade 3 students Mean age: NR | 6 weeks | (Curriculum approach) MyPyramid and Medicine Wheel Nutrition for Native Americans Culturally appropriate lessons | - F&V consumption (Servings/per day) - Fruit consumption (Servings/per day) - Vegetable consumption (Servings/per day) - Knowledge Questionnaire (% correct) | 0.10 0.519 <0.001 <0.001 |
| Horne et al. ( ) UK, Horticultural Development Council, Fresh Produce Consortium, ASDA, Co-operative Group, Safeway, Sainsbury, Somerfield, Tesco, Bird’s Eye | QE / SLT | 749 × Grades K-6 students Mean age: NR | 16 weeks | Animation abstraction and contingent reinforcement for F&V consumption | − 5–7 yr/old fruit (%) − 5–7 yr/old vegetable (%) − 7–11 yr/old fruit (%) − 7–11 yr/old vegetable (%) | <0.002 NR <0.002 NR |
| , USA, NR | RCT / NR | 1180 × Grades 2–4 students. Mean age: NR | 3 months | (Curriculum approach) developed with teachers and supported by homework, letters to parents and information evenings with parents. | - Food label quiz score Calories (kcal) Carbohydrates (g) | 0.04 0.51 0.51 |
| , UK, UK National Institute for Health Research (NIHR) Public Health Research Programme | RCT / SCT | 2121 × Grade 5 students. Mean age: 9yrs | 12 months | (Curriculum approach) Active For Life Year 5 intervention. Included teacher training, provision of lesson and child-parent interactive homework plans, all materials required for lessons and homework, and written materials for school newsletters and parents. | - F&V consumption (no./day) | 0.42 |
| , Iceland, The University of Iceland, The Icelandic Centre for Research, Brim Seafood | CT / NR | 171 × Grade 2 students Mean age: NR | 2 years | (Curriculum approach) co developed with teachers and supported by homework, letters to parents and meetings with parents | - FV consumption (g/day) - Fruit consumption (g/day) - Vegetable consumption (g/day) | <0.001 0.001 <0.001 |
| Lakshman et al. (2010), UK, Health Enterprise East, NHS innovations hub for East of England. | RCT / NR | 2519 × Grades 5–6 students. Mean age: NR | 9 weeks | (Curriculum approach) Healthy eating curriculum + Top Grub card game to be implemented in classroom and at home. | - Knowledge | 0.042 |
| Liquori et al. ( ) USA, NR. | QE / SCT | 590 × Grades K-6 students Mean age: NR | 1 year | Experiential learning (Cooking, environment and community garden) | - Preference for plant food - Attitudes - Knowledge - Self efficacy in cooking - Food intentions - Paired food choice | <0.01 <0.001 NS <0.05 NS <0.01 <0.01 |
| , Greece, Kellogg’s, Greek Ministry of Sport, Greek Ministry of Education. | QE / NR | 1006 × Grade 1 students Age range: 5.5–6.5yrs Mean age: NR | 6 years | (Curriculum approach) Literary abstraction | - Energy (kJ) - Total fat (g) - Protein (g) - Carbohydrate (g) | <0.05 <0.05 <0.05 NS |
| McAleese & Rankin ( ), USA, NR. | QE / NR | 99 × Grade 6 students Mean age: 11yrs | 12 weeks | (Curriculum approach) Experiential learning (School garden) | - Fruit (Servings/day) - Vegetables (Servings/day) - Vitamin A (µg/day) - Vitamin C (mg/day) - Fibre (g/day) | <0.001 <0.001 0.004 0.016 0.001 |
| Morgan et al. ( ) Australia, Hunter Medical Research, Coles. | QE / SCT | 127 × Grades 5–6 students Age range: 11-12yrs Mean age: NR | 10 weeks | (Curriculum approach) – Modified Experiential learning (School garden) | FV knowledge (Gimme 5 Questionnaire) - Vegetable intake (Servings/day) - Fruit intake (Servings/day) | <0.02 0.22 0.23 |
| , USA, NR | CT / ELT | 115 × 2nd Grade students Mean age: 7yrs | 28 weeks | (Curriculum approach) Nutrition lessons + school garden Experiential Learning (Gardening + Food Prep) | - MyPyramid food groups - Nutrient–food association - Nutrient–job association - F V identification - Vegetable choice (Servings) - Vegetable consumption (Servings) | NS < 0.001 < 0.001 < 0.01 <0.01 <0.01 |
| Prelip et al. ( ), USA, the Network for a Healthy California through the United States Department of Agriculture. | QE / SCT,TPB | 399 × Grades 3–5. Age range: 8-11yrs Mean age: NR | 1 year of schooling | (Curriculum approach) National curriculum and teacher training workshops | - Fruit intake - Vegetable intake - Fruit availability - Vegetable availability Food grp knowledge - FV related attitudes - FV attitude influence from parent - FV influence from teacher | < 0.01 NS NS NS <. 05 < 0.01 NS < 0.05 |
| Ransley et al. ( ), United Kingdom, NR. | QE / NR | 3703 × Children Age range: 4 – 6yrs. Mean age 6 yrs | 11 months | Provision of fruit and vegetables at school | At reception age - In year 1 - In year 2 At reception age - In year 1 - In year 2 At reception age - In year 1 - In year 2 At reception age - In year 1 - In year 2 | 95% CI (7mth follow up) 0.2 (0.1–0.4) 0.3 (0.1 – 0.6) 0 (-0.2 – 0.3) −0.2 (-0.5 – 0.1) −0.2 (-0.5–0.2) −0.3 (-0.6 – 0.1) 0.2 (0.3 – 0.1) 0.2 (−0.2 – 0.6) −0.2 (−0.5 – 0.2) −0.03 (-0.25 – 0.19) 0.03 (-0.35 – 0.4) −0.63 (-1.01 – 0.25) |
| , Portugal, NR | RCT / SCT, Health Promotion Model | 464 × Grades 1–4. Mean age: 8yrs | 6 months of lessons | (Curriculum approach) Nutrition lessons | Fruit (grams) - Vegetables (grams) - Fruits and vegetables (grams) - BMI - Weight control | < 0.01 <0.05 < 0.001 < 0.01 < 0.05 |
| Simons-Morton et al. (1991), USA, NHLBI funded | RCT / SCT | Total sample size NR. Children in kindergarten – 4th grade. Mean age NR | 3x spring sessions spanning 3 years | (Curriculum approach) Classroom nutrition lessons, Physical activity, School lunches | - Energy (kcal) [School 3] - Energy (kcal) [School 4] | Value (95% CI range) 849.3 (816.8 – 881.8) 840.9 (800.7 – 881.1) |
| Struempler et al. ( ), USA, Alabama Cooperative Extension System and the US Department of Education SNAP | QE / Experiential Learning Theory | 2477 × third graders. Mean age NR | 17 weeks | (Curriculum approach) Nutrition lessons | Fruit intake (weekly servings) - Vegetable intake (weekly servings) | < 0.001 < 0.001 |
| van de Gaar et al. (2014), The Netherlands, ZonMw, the Netherlands Organization for Health Research and Development and The Netherlands Organization for Scientific Research (NWO) | RCT / NR | 1288 × Grades 2 – 7. Mean age NR | 1 year | (Curriculum based) Healthy lifestyle promotion, Physical activity | - SSB consumed daily (% of cohort) - SSB consumption (Litres) - SSB servings - SSB consumed daily (% of cohort) - SSB consumption (Litres) - SSB servings | 0.79 (0.47 – 1.34) −0.19 (−0.28 - −0.10) −0.54 (-0.82 - −0.26) 1.32 (0.78 – 2.24) 0.04 (-0.10 – 0.19) 0.05 (-0.36 – 0.47) 0.51 (0.36 – 0.72) |
| Italy, Second University of Naples, Associazione Culturale Kaledo, Regione Campania (Assessorato all’Istruzione), Provincia di Napoli, Provincia di Salerno Assessorato allo Sport, Comune di Cercola (Assessorato all’istruzione) and Fondazione per l’Assistenza all’Infanzia | RCT / NR | 3110 × 9–19 year olds. Mean age 13yrs. | 20 weeks | Board game based education | − 6 month follow up score − 18 month follow up score − 6 month follow up score − 18 month follow up score − 6 month follow up score − 18 month follow up score − 6 month follow up score − 18 month follow up score | < 0.001 NS < 0.001 NS < 0.001 NS < 0.001 NS |
(N.B. TPB = Theory of Planned Behaviour; SCT = Social Cognitive Theory; SLT = Social Learning Theory; BCT = Behavioural Choice Theory; RCT = Randomised controlled trial; QE = Quasi-experimental; CT = Cluster-controlled trial; NR = Not reported; NS = Not significant; FV = Fruit and vegetable; SLB = Sugar-laden beverages; HFSS = High fat, sugar & salt; HFF = High Fat Food; FF = Fast food, BMI = Body Mass Index).
3.1. Studies included in energy intake Meta-Analysis
In the seven studies included in the energy intake meta-analysis ( Anderson et al., 2005 , Evans et al., 2010 , Gatto et al., 2017 , Gortmaker et al., 1999 , Liquori et al., 1998 , Manios et al., 2002 , Simons-Morton et al., 1991 ), the researchers reported the energy intake of elementary school-aged children as taught through a curriculum approach, experiential learning activities or provision of food at school through lunches or the school canteen. In these studies, researchers included information on energy intake using food diaries that were completed by: (1) parents of children in the study; (2) self-reported; or (3) teacher estimates.
3.1.1. Study quality
Of the seven studies whose quality was assessed by using the methodological quality assessment items adapted from van Sluijs et al. (2007) , only three of the six papers met five or more of the assessment criteria ( Evans et al., 2010 , Gortmaker et al., 1999 , Manios et al., 2002 ). One paper met four of the criteria ( Gatto et al., 2017 ), one met three criteria ( Anderson et al., 2005 ) and two studies met only two of the prescribed criteria ( Liquori et al., 1998 , Simons-Morton et al., 1991 ). All seven papers reported their findings using validated measures.
3.1.2. Summary
The analysis is based on seven studies that evaluated the effect of teaching-based interventions on energy intake of students aged 5–12 years of age attending primary/elementary schools. In each study, students were assigned to either a reduction of energy intake teaching intervention or their regular curricular and the researchers recorded their energy intake at the conclusion of the intervention period. The effect size is the standardised mean difference and is reported using Cohen’s d . The Cohen’s d effect size estimate is calculated using a relative weight assignment to each of the included studies based on the precision of the effect reported. In other words, studies that reported higher degrees of precision (i.e. less variance around the mean) contribute more to the overall Cohen’s d that those with less precision (i.e. greater variance around the mean).
The studies in this analysis were sampled from a universe of possible studies defined by the inclusion/exclusion criteria defined earlier in the paper. For this reason, the random-effects model was employed for analysis. The conclusion (below) applies to that universe.
3.1.3. Do teaching-based interventions affect student energy intake?
The standardised difference in means is d = 0.396. On average, students receiving the teaching-based intervention reduced their energy intake by over a third of a standard deviation than those students who did not receive a nutrition teaching intervention.
The confidence interval for the standardised difference in means is 0.042 to 0.751, which tells us that the mean effect size in the universe of studies could fall anywhere in this range.
The Z-value for testing the null hypothesis (that d is 0.0) is 2.190, with a p = 0.029. Thus, we can reject the null that teaching-based interventions have no effect on student energy intake with greater than 95% certainty.
3.1.4. How much does the effect size vary across studies (Heterogeneity)?
To test the null hypothesis that all studies in the analysis share a common effect size the Q-statistic was used in conjunction with the I 2 statistic (what proportion of the observed variance reflects differences in true effect sizes rather than sampling error), T (the standard deviation of true effects) and T 2 (the variance of true effect sizes). The Q-value is 71.783 with 6 degrees of freedom and p < 0.001. Thus, we reject the null hypothesis that the true effect size is identical in all studies. The I 2 is 91.681%, T 2 is 0.184 and T is 0.429 indicating considerable heterogeneity among the included studies.
The prediction interval is −0.8009 to 1.5929. We would expect the true effect size for 95% of all populations receiving the interventions to fall within this range.
3.1.5. To what extent would publication bias or the small-study effect alter these findings?
Publication bias suggests that not all completed studies are published, instead studies that have large effects are more likely to be submitted and/or accepted for publication than studies that do not have such large effect sizes. As the treatment effect estimated was calculated from a potentially biased collection of studies, the following analyses were applied to assess the extent of that bias.
Initially, the Classic fail-safe analysis was undertaken. The results showed that the incorporated data from seven studies yielded a z-value of 5.59397 and corresponding 2-tailed p < 0.0001. The fail-safe N in this case is 51. This suggests that 51 ‘null’ studies would need to be included for a combined 2-tailed p > 0.05 i.e., for the effect to be nullified.
Next, we applied Duval and Tweedie’s ( Duval and Tweedie, 2000 ) ‘Trim and Fill’ method that looks for missing studies in a symmetric funnel plot. This method looks for missing studies to the left side of the mean effect. The result suggests that no studies should be trimmed from the left or right of the mean to reduce the potential publication bias in this instance.
3.2. Studies included in sugar consumption Meta-Analysis
Five studies ( Anderson et al., 2005 , Evans et al., 2010 , Fahlman et al., 2008 , Francis et al., 2010 , van de Gaar et al., 2014 ) were included that investigated the sugar intake of elementary school- aged children as taught through a curriculum approach, experiential learning and provision of fruits and vegetables at school. The sugar consumption was reported through the variables of: (1) sugar-sweetened beverage consumption; (2) 24-hour dietary recalls; and (3) self-reported intake of sugary foods.
3.2.1. Study quality
Of the five studies whose quality was assessed by using the methodological quality assessment items adapted from van Sluijs et al. ( van Sluijs et al., 2007 ), three of the five studies met seven of the assessment criteria ( Evans et al., 2010 , Francis et al., 2010 , van de Gaar et al., 2014 ). One study met three criteria ( Anderson et al., 2005 ) and the last met only two of the criteria ( Fahlman et al., 2008 ). All five papers reported their findings using validated measures.
3.2.2. Summary
The analysis is based on five studies that evaluated the effect of teaching-based interventions on sugar consumption of students aged 5–12 years of age attending primary/elementary schools. In each study, students were assigned to either a reduction of sugar consumption teaching intervention or their regular curricular and the researchers recorded their sugar consumption at the conclusion of the intervention or follow-up period (whichever was the latter).
3.2.3. Do teaching-based interventions affect student sugar consumption?
The standardised difference in means is d = 0.144. On average, students receiving the teaching-based intervention reduced their sugar consumption by an eighth of a standard deviation than those students who did not receive a nutrition teaching intervention.
The confidence interval for the standardised difference in means is 0.004 to 0.284. This range does not include an effect size of zero, which tells us that the true effect size is probably not zero.
In addition, for testing the null hypothesis, the Z-value is 2.023, with a p = 0.043. Thus, we can reject the null that teaching-based interventions have no effect on student sugar consumption with greater than 95% confidence.
3.2.4. How much does the effect size vary across studies (Heterogeneity)?
The Q-value is 23.919 with 4 degrees of freedom and p = 0.004. We reject the null hypothesis that the true effect size is identical in all studies. I 2 is 71.630%, T 2 is 0.017 and T is 0.130. The prediction interval is −0.3291 to 0.6171. We concluded that here is substantial heterogeneity across these studies.
3.2.5. To what extent would publication bias or the small-study effect alter these findings?
The Classic fail-safe analysis that showed this meta-analysis incorporated data from five studies and yield a z-value of 3.76678 and corresponding 2-tailed p < 0.0002. The fail-safe N in this case is 14, indicating that there would need to be less than three missing studies for every observed study for the effect to be nullified.
The ‘Trim and Fill’ method suggests that no studies are missing to the left of the mean, but one study is potentially missing from the right of the mean. If three studies were to be trimmed to account for this bias, the adjusted standardised difference in means would be d = 0.181.
3.3. Studies included in FV consumption Meta-Analysis
The fruit and vegetable consumption of elementary school aged children was reported in 21 studies ( Fahlman et al., 2008 , Anderson et al., 2005 , Evans et al., 2010 , Gatto et al., 2017 , Gortmaker et al., 1999 , Amaro et al., 2006 , Auld et al., 1998 , Baranowski et al., 2000 , Bere et al., 2006 , Cooke et al., 2011 , Day et al., 2008 , Fairclough et al., 2013 , Gibbs et al., 2013 , Govula et al., 2007 , Horne et al., 2004 , McAleese and Rankin, 2007 , Morgan et al., 2010 , Prelip et al., 2012 , Ransley et al., 2007 , Rosário et al., 2016 , Struempler et al., 2014 ) included in this meta-analysis through experiential learning in schools, curricular approaches, the use of board games, and providing fruits and vegetables to children at school. The 21 studies included information on fruit and vegetable intake using the following variables: (1) 24-hour dietary recalls; (2) teacher estimates of consumption; (3) nutrition knowledge test scores; (4) scales measuring how much children like fruits and vegetables; and (5) parent surveys.
3.3.1. Study quality
Of the 21 studies whose quality was assessed using the methodological quality assessment items adapted from van Sluijs et al. ( van Sluijs et al., 2007 ), 13 had between 5 and 7 of the assessment criteria ( Bere et al., 2006 , Morgan et al., 2010 , Day et al., 2008 , Fairclough et al., 2013 , Gibbs et al., 2013 , Ransley et al., 2007 , Rosário et al., 2016 , Struempler et al., 2014 ), 6 had between 3 and 4 of the assessment criteria ( Anderson et al., 2005 , Gatto et al., 2017 , Cooke et al., 2011 , Govula et al., 2007 , Horne et al., 2004 , Prelip et al., 2012 ) and 2 studies had only 2 of the assessment criteria ( Fahlman et al., 2008 , McAleese and Rankin, 2007 ). All 21 papers reported their findings using validated measures.
3.3.2. Summary
The analysis is based on 21 studies that evaluated the effect of teaching-based interventions on the fruit and vegetable consumption of students aged 5–12 years of age attending primary/elementary schools. In each study, students were assigned to either a nutrition focussed teaching intervention or their regular curricular and the researchers recorded their fruit/vegetable consumption at the conclusion of the intervention period.
3.3.3. Do teaching-based interventions affect fruit and vegetable consumption?
The standardised difference in means is d = 0.228. On average, students receiving the teaching-based intervention consumed almost a quarter of a standard deviation more fruit and vegetables than those students who did not receive a teaching intervention. The confidence interval for the standardised difference in means is 0.141 to 0.315.
Similarly, the Z-value for testing the null hypothesis (that d is 0.0) is 5.127, with a p < 0.001. We can reject the null that teaching-based interventions have no effect on student fruit and vegetable consumption.
3.3.4. How much does the effect size vary across studies (Heterogeneity)?
The Q-value is 129.223 with 20 degrees of freedom and p < 0.001. We reject the null hypothesis that the true effect size is identical in all studies. I 2 is 84.523%, T 2 is 0.029, and T = 0.169 indicating that considerable heterogeneity exists across the included studies. The prediction interval is −0.1403 to 0.5963.
3.3.5. To what extent would publication bias or the small-study effect alter these findings?
The Classic fail-safe analysis showed this meta-analysis incorporated data from 21 studies and yield a z-value of 10.70147 and corresponding 2-tailed p < 0.0001 for observed studies. The fail-safe N in this case is 606. There would need to be 29 missing studies for every observed study for the effect to be nullified.
The ‘Trim and Fill’ method based on a random effects model suggests that no studies were missing from the left of the mean and three studies from the right of the mean. If three studies were to be trimmed to account for this bias, the adjusted standardised difference in means would only slightly decrease to d = 0.272.
3.4. Studies included in nutritional knowledge Meta-Analysis
Thirteen studies were included ( Anderson et al., 2005 , Liquori et al., 1998 , Fahlman et al., 2008 , Francis et al., 2010 , Govula et al., 2007 , Morgan et al., 2010 , Prelip et al., 2012 , Amaro et al., 2006 , Auld et al., 1998 , Baranowski et al., 2000 , Campbell et al., 2012 , Friel et al., 1999 , Lakshman et al., 2010 ), with researchers reporting on elementary school children’s level of nutrition knowledge as taught through curriculum approaches in the classroom, the use of board games and experiential learning tasks including school gardens. Knowledge of nutrition was measured using: (1) eating attitude tests; (2) self efficacy scales; (3) nutrition knowledge questionnaires; and (4) attitudes to food questionnaires.
3.4.1. Study quality
Of the 13 studies whose quality was assessed by using the methodological quality assessment items adapted from van Sluijs et al. ( van Sluijs et al., 2007 ), only six of the 13 papers met five or more of the assessment criteria ( Francis et al., 2010 , Morgan et al., 2010 , Lakshman et al., 2010 , Amaro et al., 2006 , Auld et al., 1998 , Baranowski et al., 2000 ) and seven studies met between two and four of the assessment criteria ( Anderson et al., 2005 , Liquori et al., 1998 , Fahlman et al., 2008 , Govula et al., 2007 , Prelip et al., 2012 , Campbell et al., 2012 , Friel et al., 1999 ). All 13 papers reported their findings using validated measures.
3.4.2. Summary
The analysis is based on 13 studies that evaluated the effect of teaching-based interventions on nutritional knowledge of students aged 5–12 years of age attending primary/elementary schools. In each study, students were assigned to either a nutrition focussed teaching intervention or their regular curricular and the researchers recorded their nutritional knowledge at the conclusion of the intervention period.
3.4.3. Do teaching-based interventions affect student nutritional knowledge?
The standardised difference in means is d = 0.224. On average, students receiving the teaching-based intervention scored nearly a quarter of a standard deviation higher in terms of nutritional knowledge than those students who did not receive a nutrition teaching intervention.
The confidence interval for the standardised difference in means is 0.142 to 0.305. Similarly, the Z-value for testing the null hypothesis (that d is 0.0) is 5.384, with a p < 0.001. We can reject the null that teaching-based interventions have no effect on student nutritional knowledge.
3.4.4. How much does the effect size vary across studies (Heterogeneity)?
The Q-value is 29.446 with 12 degrees of freedom and p < 0.001. The I 2 statistic reflecting the proportion of the observed variance differences in true effect sizes rather than sampling error is 59.248%, T 2 is 0.010 and T = 0.102. The prediction interval is −0.0142 to 0.4662. Again, in this instance we are led to conclude that substantial heterogeneity exists across the studies included in this analysis.
3.4.5. To what extent would publication bias or the small-study effect alter these findings?
The Classic fail-safe analysis that showed this meta-analysis incorporated data from 13 studies and yield a z-value of 9.18895 and corresponding 2-tailed p < 0.0001. The fail-safe N in this case is 3246. There would need to be 21 missing studies for every observed study for the effect to be nullified.
Secondly, the ‘Trim and Fill’ method using a random effects model suggests that six studies are missing to the left of the mean but none from the right. It suggests six studies could be trimmed from the left of the mean to reduce bias which would decrease the observed effect to d = 0.156.
4. Discussion
The main findings of this review and meta-analysis indicate that nutrition education programs in elementary schools that are delivered by teachers can have modest effects on a child’s nutritional knowledge and eating behaviours. It appears that elementary school teachers and nutritional education programs can have a small to medium effect on reducing children’s energy intake (d = 0.396), followed by smaller effects on increasing fruit and vegetable consumption (d = 0.228) and nutritional knowledge (d = 0.224). The smallest effect was found on reducing children's sugar consumption, with teachers and nutritional education programs having a very small effect (d = 0.144).
Previous research focusing on elementary school-based nutritional education programs shows that effectiveness depends on the duration of the program, having a few focused nutrition-related outcomes, the appropriate use of theoretical frameworks, fidelity of nutritional education programs, support from school leadership and policy makers, changes in the food school environment, provision of professional learning alongside the delivery of the nutritional education program for teachers, and strategies embedded to engage parents and families ( Murimi et al., 2018 , Peralta et al., 2016 , Dudley et al., 2015 , Australian Bureau of Statistics. Australian health survey: nutrition first results – foods and nutrients, 2014 , Colley et al., 2018 ).
In regards to energy intake, unhealthy foods, such as sugary, salty snacks and sugar-sweetened beverages, can contribute up to 40% of 2- to 13-year-old children’s total energy intake, with the greatest increase in this intake occurring with children aged 3 to 4 years and 5 to 8 years ( Department of Health FSA, 2012 , Keast et al., 2013 , Van Cauwenberghe et al., 2010 ). When these behaviours are targeted through multifaceted school-based nutrition education programs, with regular curricular and non-curricular lessons, delivered by nutritionists or teachers, and engaged parents ( Micha et al., 2018 ), energy intake can be reduced, and reduced substantially as shown through this meta-analysis.
When focusing on increasing fruit and vegetable consumption only, findings of two previous reviews ( Murimi et al., 2018 , Savoie-Roskos et al., 2017 ) emphasise that multifaceted interventions that include improved availability of fruit and vegetables, a nutrition education curriculum delivered by teachers with embedded experiential learning experiences, and parental involvement can improve intake of fruits and vegetables. As such, it is not surprising that there has been a proliferation of elementary school nutrition education programs that have used these findings and assessed the impact of gardening and curriculum programs on elementary school children’s fruit and vegetable consumption. A systematic review of gardening interventions ( World Health Organization. Guideline: Sugars intake for adults and children. Geneva, Switzerland;, 2015 ) found that 10 of the 14 articles reviewed produced statistically significant increases in fruit or vegetable consumption among children. Due to many of the 10 studies being limited by the use of convenience samples, small sample sizes, and self-reported measurements of fruit and vegetable consumption, it is important to note that the evidence is not yet clear, with future studies needing to include control groups, randomized designs, and assessments of fruit and vegetable consumption over at least 1 year to advance the literature.
Estimates on sugar consumption suggests that approximately 5% of energy is attributed to sugar sweetened beverage consumption ( Bleich and Vercammen, 2018 ). This is concerning, as it would appear that sugar sweetened beverage consumption alone is already meeting the new World Health Organization's guidelines for maximum free-sugar consumption ( Bleich and Vercammen, 2018 ) and therefore should be a prime target for reducing sugar consumption in children. Despite the clear and consistent evidence that consumption of sugar sweetened beverage consumption increases obesity risk and dental caries among children, and emerging evidence supporting an association with insulin resistance and caffeine-related effects ( Nathan et al., 2019 ), reducing children’s sugar consumption seems to be challenging and complex. A recent systematic review and meta-analysis focusing on the effectiveness of lunchbox interventions in elementary and pre-schools ( Nathan et al., 2019 ), found that removing items that are less healthy from students’ lunchboxes may be more difficult than adding healthier options like fruit and vegetables. Consequently, the researchers suggested that greater formative evaluation with the lunch box packers (i.e., the parents) may be required to improve the shape and impact of future interventions that target high sugar foods.
Only one study included in our meta-analysis included parental engagement as a teaching strategy but reported the second largest effect size recorded ( van de Gaar et al., 2014 ; d = 0.144). A qualitative paper interviewing elementary school-aged children and their perceptions of sugar sweetened beverage consumption, reported that children had a high level of awareness of beverages, the sugar content and health effects ( Battram et al., 2016 ). Hence, children highlighted that they made choices based on taste, parental control practices, accessibility, and advertising, and offered suggestions or strategies for school nutrition education programs that focused on sugar consumption. These included limiting advertising of sugar sweetened beverage consumption, providing incentives to purchase healthy options, and increasing the cost of sugar sweetened beverages or lowering the cost of healthy beverage choices, more education at school and education for parents ( Battram et al., 2016 ).
A limitation of this study was that only one author screened the articles based on titles and abstracts (stage 1) and that a second author was only used in cases of uncertainty in stage 2. This could increase the risk of bias ( Cooper, 2015 ).
5. Conclusion
The findings of this systematic review and meta-analysis suggest that the teaching of nutrition education in elementary schools by teachers can make an important contribution to the knowledge and dietary habits of children. A subsequent finding also suggests that parents and caregivers have an important role to play. The small and medium effect sizes indicate that prudent and evidence-based decisions need to be made by policy makers and pedagogues as to the teaching strategies they employ however not all nutrition education approaches render the same effect. Future intervention research in this field would be well served by augmenting strategies that demonstrate higher effects in nutritional knowledge, reducing energy intake, and increasing fruit and vegetable consumption. New, and a greater number of studies, need to be employed that reduce sugar consumption by children.
The University of Sydney’s Research Recognition and Incentive Fund partly funded this study. The funding was used to employ a research assistant to conduct, record and collate initial literature searches.
CRediT authorship contribution statement
Wayne Cotton: Conceptualization, Methodology, Investigation, Writing - original draft, Writing - review & editing, Validation, Supervision, Project administration, Funding acquisition. Dean Dudley: Conceptualization, Methodology, Formal analysis, Writing - original draft. Louisa Peralta: Conceptualization, Writing - original draft, Writing - review & editing, Validation. Thea Werkhoven: Data curation, Resources, Investigation, Writing - original draft, Visualization, Writing - review & editing.
- Amaro S., Viggiano Alessandro, Di Costanzo Anna, Madeo Ida, Viggiano Andrea, Baccari Maria Ena, Marchitelli Elena, Raia Maddalena, Viggiano Emanuela, Deepak Sunil, Monda Marcellino, De Luca Bruno. a new educational board-game, gives nutritional rudiments and encourages healthy eating in children: a pilot cluster randomized trial. Eur. J. Pediatr. 2006; 165 (9):630. [ PubMed ] [ Google Scholar ]
- Anderson A.S., Porteous L.E.G., Foster E., Higgins C., Stead M., Hetherington M. The impact of a school-based nutrition education intervention on dietary intake and cognitive and attitudinal variables relating to fruits and vegetables. Public Health Nutr. 2005; 8 (6):650–656. [ PubMed ] [ Google Scholar ]
- Auld G.W., Romaniello C., Heimendinger J., Hambidge C., Hambidge M. Outcomes from a school-based nutrition education program using resource teachers and cross-disciplinary models. J. Nutr. Educ. 1998; 30 (5):268–280. [ Google Scholar ]
- Australian Bureau of Statistics. Australian health survey: nutrition first results – foods and nutrients, 2011–12: Australian Government; 2014 [Available from: http://www.abs.gov.au/ausstats/[email protected]/Lookup/4364.0.55.007main+features12011-12 .
- Baranowski T., Davis M., Resnicow K., Baranowski J., Doyle C., Lin L.S. Gimme 5 Fruit, Juice, and Vegetables for Fun and Health: Outcome Evaluation. Health Educ. Behavior. 2000; 27 (1):96–111. [ PubMed ] [ Google Scholar ]
- Battjes-Fries M.C.E., Haveman-Nies A., Renes R.-J., Meester H.J., van't Veer P. Effect of the Dutch school-based education programme 'Taste Lessons' on behavioural determinants of taste acceptance and healthy eating: a quasi-experimental study. Pub. Health Nut. 2015; 18 (12):2231–2241. doi: 10.1017/S1368980014003012. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Battram D.S., Piche L., Beynon C., Kurtz J., He M. Sugar-Sweetened Beverages: Children's Perceptions, Factors of Influence, and Suggestions for Reducing Intake. J. Nutr. Educ. Behav. 2016; 48 (1):27–34.e1. [ PubMed ] [ Google Scholar ]
- Bere E., Veierød M.B., Bjelland M., Klepp K.-I. Outcome and process evaluation of a Norwegian school-randomized fruit and vegetable intervention: fruits and Vegetables Make the Marks (FVMM) Health Educ. Res. 2006; 21 (2):258. [ PubMed ] [ Google Scholar ]
- Bleich S.N., Vercammen K.A. The negative impact of sugar-sweetened beverages on children’s health: an update of the literature. BMC Obesity. 2018; 5 (1):6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Campbell A.C., Barnum D.B., Ryden V.B., Ishkanian S.B., Stock S., Chanoine J.P. The Effectiveness of the Implementation of Healthy Buddies™, a School-Based, Peer-Led Health Promotion Program in Elementary Schools. Can. J. Diabetes. 2012; 36 (4):181–196. [ Google Scholar ]
- Cohen J. 2nd ed. Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. Statistical power analysis for the behavioral sciences. [ Google Scholar ]
- The Cochrane Collaboration. Fail-safe N 2011 [updated March 2011. 5.1.0: [Available from: https://handbook-5-1.cochrane.org/index.htm#chapter_10/10_4_4_3_fail_safe_n.htm .
- Colley P., Myer B., Seabrook J., Gilliland J. The impact of Canadian school food programs on children's nutrition and health: a systematic review. Can. J. Dietetic Practice and Res. 2018; 80 (2):79–86. [ PubMed ] [ Google Scholar ]
- Cooke L.J., Chambers L.C., Anez E.V., Croker H.A., Boniface D., Yeomans M.R. Eating for pleasure or profit: The effect of incentives on children's enjoyment of vegetables. Psychol. Sci. 2011; 22 (2):190–196. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cooper H. Sage publications; London: 2015. Research Synthesis and Meta-Analysis: A Step-by-Step Approach. [ Google Scholar ]
- Day M.E., Strange K.S.P., McKay H.A.P., Naylor P.-J.P. Action Schools! BC - Healthy Eating: Effects of a Whole-school Model to Modifying Eating Behaviours of Elementary School Children. Can. J. Public Health. 2008; 99 (4):328–331. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- de Vlieger N., Riley N., Miller A., Collins C., Bucher T. Nutrition education in the Australian New South Wales primary school curriculum: an exploration of time allocation, translation and attitudes in a sample of teachers. Health Promot. J. Austr. 2019; 30 (1):94–101. [ PubMed ] [ Google Scholar ]
- Department of Health FSA . Department of Health; England, UK: 2012. National diet and nutrition survey headline results from years 1, 2 and 3 (combined) of the rolling programme (2008/2009–2010/11) [ Google Scholar ]
- DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986; 7 (3):177–188. [ PubMed ] [ Google Scholar ]
- Dudley D.A., Cotton W.G., Peralta L.R. Teaching approaches and strategies that promote healthy eating in primary school children: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Activity. 2015; 12 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dudley D., Peralta L., Cotton W., Baxter D. NSW Department of Education and Communities,; Sydney, Australia: 2015. Teaching healthy eating to primary school students: A review of evidence and best practice. [ Google Scholar ]
- Duval S., Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000; 56 (2):455–463. [ PubMed ] [ Google Scholar ]
- Evans C.E.L., Greenwood D.C., Cade J.E. 068 Systematic review and meta-analysis of school-based interventions to improve fruit and vegetable intake. J. Epidemiol. Community Health. 2010; 64 [ Google Scholar ]
- Fahlman M.M., Dake J.A., McCaughtry N., Martin J. A Pilot Study to Examine the Effects of a Nutrition Intervention on Nutrition Knowledge, Behaviors, and Efficacy Expectations in Middle School Children. J. Sch. Health. 2008; 78 (4):216–222. [ PubMed ] [ Google Scholar ]
- Fairclough S.J., Hackett A.F., Davies I.G., Gobbi R., Mackintosh K.A., Warburton G.L. Promoting healthy weight in primary school children through physical activity and nutrition education: a pragmatic evaluation of the CHANGE! randomised intervention study. BMC Public Health. 2013; 13 :626. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Francis M., Nichols S.S.D., Dalrymple N. The effects of a school-based intervention programme on dietary intakes and physical activity among primary-school children in Trinidad and Tobago. Public Health Nutr. 2010; 13 (5):738–747. [ PubMed ] [ Google Scholar ]
- Friel S., Kelleher C., Campbell P., Nolan G. Evaluation of the Nutrition Education at Primary School (NEAPS) programme. Public Health Nutr. 1999; 2 (4):549–555. [ PubMed ] [ Google Scholar ]
- Gatto N.M., Martinez L.C., Spruijt-Metz D., Davis J.N. LA sprouts randomized controlled nutrition, cooking and gardening programme reduces obesity and metabolic risk in Hispanic/Latino youth. Pediatric Obesity. 2017; 12 (1):28–37. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gibbs L., Staiger P.K., Johnson B., Block K., Macfarlane S., Gold L. Expanding Children's Food Experiences: The Impact of a School-Based Kitchen Garden Program. J. Nutr. Educ. Behavior. 2013; 45 (2):137–146. [ PubMed ] [ Google Scholar ]
- Goran M.I., Ball G.D., Cruz M.L. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J. Clin. Endocrinol. Metab. 2003; 88 (4):1417–1427. [ PubMed ] [ Google Scholar ]
- Gortmaker S.L., Cheung L.W.Y., Peterson K.E., Chomitz G., Cradle J.H., Dart H. Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children: eat well and keep moving. Arch. Pediatr. Adolesc. Med. 1999; 153 (9):975–983. [ PubMed ] [ Google Scholar ]
- Govula C., Kattelman K., PhD R.D., Ren C. Culturally appropriate nutrition lessons increased fruit and vegetable consumption in American Indian children. Top Clin Nutr. 2007; 22 (3):239–245. [ Google Scholar ]
- Graziose M.M., Koch P.A., Wang Y.C., Lee Gray H., Contento I.R. Cost-effectiveness of a nutrition education curriculum intervention in elementary schools. J. Nutr. Educ. Behav. 2017; 49 (8):684–969. [ PubMed ] [ Google Scholar ]
- Horne P.J., Tapper K., Lowe C.F., Hardman C.A. Increasing children's fruit and vegetable consumption: A peer-modelling and rewards-based intervention. Eur. J. Clin. Nutr. 2004; 58 (12):1649–1660. [ PubMed ] [ Google Scholar ]
- Katz D.L., Katz C.S., Treu J.A., Reynolds J., Njike V., Walker J.…Michael J. Teaching healthful food choices to elementary school students and their parents: the nutrition detectives[TM] program. J. School Health. 2011; 81 (1):21–28. [ PubMed ] [ Google Scholar ]
- Keast D.R., Fulgoni V.L., 3rd, Nicklas T.A., O'Neil C.E. Food sources of energy and nutrients among children in the United States: National Health and Nutrition Examination Survey 2003–2006. Nutrients. 2013; 5 (1):283–301. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kelsey M.M., Zaepfel A., Bjornstad P., Nadeau K.J. Age-related consequences of childhood obesity. Gerontology. 2014; 60 (3):222–228. [ PubMed ] [ Google Scholar ]
- Kipping R.R., Howe L.D., Jago R., Campbell R., Wells S., Chittleborough C.R.…Lawlor D.A. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ: British Medical Journal. 2014; 348 doi: 10.1136/bmj.g3256. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kristjansdottir A.G., Johannsson E., Thorsdottir I. Effects of a school-based intervention on adherence of 7-9-year-olds to food-based dietary guidelines and intake of nutrients. Pub. Health Nut. 2010; 13 (8):1151–1161. doi: 10.1017/S1368980010000716. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lakshman Rajalakshmi R., Sharp Stephen J., Ong Ken K., Forouhi Nita G. A novel school-based intervention to improve nutrition knowledge in children: cluster randomised controlled trial. BMC Public Health. 2010; 10 :123. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Liquori T., Koch P.D., Contento I.R., Castle J. The Cookshop Program: Outcome evaluation of a nutrition education program linking lunchroom food experiences with classroom cooking experiences. J. Nutr. Educ. 1998; 30 (5):302–313. [ Google Scholar ]
- Manios Y., Moschandreas J., Hatzis C., Kafatos A. Health and nutrition education in primary schools of Crete: changes in chronic disease risk factors following a 6-year intervention programme. Br. J. Nutr. 2002; 88 (3):315. [ PubMed ] [ Google Scholar ]
- McAleese J.D., Rankin L.L. Garden-based nutrition education affects fruit and vegetable consumption in sixth-grade adolescents. J. Am. Diet. Assoc. 2007; 107 (4):662–665. [ PubMed ] [ Google Scholar ]
- Micha R., Karageorgou D., Bakogianni I., Trichia E., Whitsel L.P., Story M. Effectiveness of school food environment policies on children's dietary behaviors: A systematic review and meta-analysis. PLoS ONE. 2018; 13 (3) [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., The P.G. Preferred Reporting Items For Systematic Reviews And Meta-Analyses: The PRISMA statement. PLoS Med. 2009; 6 (7) [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Morgan P.J., Warren J.M., Lubans D.R., Saunders K.L., Quick G.I., Collins C.E. The impact of nutrition education with and without a school garden on knowledge, vegetable intake and preferences and quality of school life among primary-school students. Public Health Nutr. 2010; 13 (11):1931–1940. [ PubMed ] [ Google Scholar ]
- Murimi M.W., Moyeda-Carabaza A.F., Nguyen B., Saha S., Amin R., Njike V. Factors that contribute to effective nutrition education interventions in children: a systematic review. Nutr. Rev. 2018; 76 (8):553–580. [ PubMed ] [ Google Scholar ]
- Nathan N., Janssen L., Sutherland R., Hodder R.K., Evans C.E.L., Booth D. The effectiveness of lunchbox interventions on improving the foods and beverages packed and consumed by children at centre-based care or school: a systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2019; 16 (1):38. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Parmer S.M., Salisbury-Glennon J., Shannon D., Struempler B. School gardens: an experiential learning approach for a nutrition education program to increase fruit and vegetable knowledge, preference, and consumption among second-grade students. J. Nut. Edu. Behav. 2009; 41 (3):212–217. [ PubMed ] [ Google Scholar ]
- Peralta L.R., Dudley D.A., Cotton W.G. Teaching Healthy Eating to Elementary School Students: A Scoping Review of Nutrition Education Resources. J. Sch. Health. 2016; 86 (5):334–345. [ PubMed ] [ Google Scholar ]
- Porter K.J., Koch P.A., Contento I.R. Why and how schools make nutrition education programs “Work” J. Sch. Health. 2018; 88 (1):23–33. [ PubMed ] [ Google Scholar ]
- Prelip M., Kinsler J., Thai C.L., Erausquin J.T., Slusser W. Evaluation of a school-based multicomponent nutrition education program to improve young children's fruit and vegetable consumption. J. Nutr. Educ. Behavior. 2012; 44 (4):310–318. [ PubMed ] [ Google Scholar ]
- Ransley J.K., Greenwood D.C., Cade J.E., Blenkinsop S., Schagen I., Teeman D. Does the school fruit and vegetable scheme improve children’s diet? A non-randomised controlled trial. J. Epidemiol. Community Health. 2007; 61 (8):699. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Reilly J.J., Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int. J. Obesity 2014. 2011; 35 (7):891–898. [ PubMed ] [ Google Scholar ]
- Rosário R., Oliveira B., Araújo A., Lopes O., Padrão P., Moreira A.…Moreira P. The impact of an intervention taught by trained teachers on childhood overweight. Int. J. Environ. Res. Public Health. 2012; 9 (4):1355–1367. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rosário R., Araújo A., Padrão P., Lopes O., Moreira A., Abreu S., Vale S., Pereira B., Moreira P. Impact of a school-based intervention to promote fruit intake: a cluster randomized controlled trial. Public Health. 2016; 136 :94. [ PubMed ] [ Google Scholar ]
- Savoie-Roskos M.R., Wengreen H., Durward C. Increasing Fruit and Vegetable Intake among Children and Youth through Gardening-Based Interventions: A Systematic Review. J. Acad. Nutr. Dietetics. 2017; 117 (2):240–250. [ PubMed ] [ Google Scholar ]
- Simons-Morton B.G., Parcel G.S., Baranowski T., Forthofer R., O'Hara N.M. Promoting physical activity and a healthful diet among children: results of a school-based intervention study. Am. J. Public Health. 1991; 81 (8):986. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Story M., Nanney M.S., Schwartz M.B. Schools and obesity prevention: creating school environments and policies to promote healthy eating and physical activity. The Milbank Quarterly. 2009; 87 (1):71–100. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Struempler B.J., Parmer S.M., Mastropietro L.M., Arsiwalla D., Bubb R.R. Changes in fruit and vegetable consumption of third-grade students in body quest: Food of the warrior, a 17-class childhood obesity prevention program. J. Nutr. Educ. Behavior. 2014; 46 (4):286–292. [ PubMed ] [ Google Scholar ]
- United Nations Educational Scientific and Cultural Organization . UNESCO; Paris: 2013. Making Education a Priority in the Post-2015 Development Agenda. [ Google Scholar ]
- Van Cauwenberghe E., Maes L., Spittaels H., van Lenthe F.J., Brug J., Oppert J.M. Effectiveness of school-based interventions in Europe to promote healthy nutrition in children and adolescents: systematic review of published and 'grey' literature. Br. J. Nutr. 2010; 103 (6):781–797. [ PubMed ] [ Google Scholar ]
- van de Gaar V., Jansen W., Grieken A., Borsboom G., Kremers S., Raat H. Effects of an intervention aimed at reducing the intake of sugar-sweetened beverages in primary school children: A controlled trial. Int. J. Behav. Nutr. Phys. Activity. 2014; 11 (1):98. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- van Geel M., Vedder P., Tanilon J. Are overweight and obese youths more often bullied by their peers? A meta-analysis on the correlation between weight status and bullying. Int. J. Obesity 2014. 2014; 38 (10):1263–1267. [ PubMed ] [ Google Scholar ]
- van Sluijs E.M.F., McMinn A.M., Griffin S.J. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ (Clinical research ed). 2007; 335 (7622):703–707. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Viggiano A., Viggiano E., Di Costanzo A., Viggiano A., Andreozzi E., Romano V.…Amaro S. Kaledo, a board game for nutrition education of children and adolescents at school: cluster randomized controlled trial of healthy lifestyle promotion. Euro. J. Ped. 2015; 174 (2):217–228. doi: 10.1007/s00431-014-2381-8. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization . World Health Organization; Geneva, Switzerland: 2012. Population-Based Approaches to Childhood Obesity Prevention. [ Google Scholar ]
- World Health Organization. Guideline: Sugars intake for adults and children. Geneva, Switzerland; 2015 31 March. [ PubMed ]
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Supplement Archive
- Article Collection Archive
- Author Guidelines
- Submission Site
- Open Access
- Call for Papers
- Why Publish?
- About Nutrition Reviews
- About International Life Sciences Institute
- Editorial Board
- Early Career Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, school-age health and nutrition terminology and knowledge gaps, specificities of growth and development in school age, role of nutrition in school age, global status of nutrition in school age, recovery from nutrient deficiencies, growth faltering, and cognition in school-age children, revisiting priorities, acknowledgments.
- < Previous
Nutrition in school-age children: a rationale for revisiting priorities
- Article contents
- Figures & tables
- Supplementary Data
Jose M Saavedra, Andrew M Prentice, Nutrition in school-age children: a rationale for revisiting priorities, Nutrition Reviews , Volume 81, Issue 7, July 2023, Pages 823–843, https://doi.org/10.1093/nutrit/nuac089
- Permissions Icon Permissions
Middle childhood and early adolescence have received disproportionately low levels of scientific attention relative to other life stages, especially as related to nutrition and health. This is partly due to the justified emphasis on the first 1000 days of life, and the idea that early deficits and consequences may not be fully reversible. In addition, these stages of life may superficially appear less “eventful” than infancy or late adolescence. Finally, there has been historical ambiguity and inconsistency in terminology, depending on whether viewing “childhood” through physiologic, social, legal, or other lenses. Nevertheless, this age bracket, which encompasses most of the primary education and basic schooling years for most individuals, is marked by significant changes, inflection points, and sexually driven divergence in somatic and brain growth and development trajectories. These constitute transformative changes, and thus middle childhood and early adolescence represents a major and last opportunity to influence long-term health and productivity. This review highlights the specificities of growth and development in school age, with a focus on middle childhood and early adolescence (5 years–15 years of age, for the purposes of this review), the role of nutrition, the short- and long-term consequences of inadequate nutrition, and the current global status of nutrition in this age group. Adequate attention and emphasis on nutrition in the school-age years is critical: (a) for maintaining an adequate course of somatic and cognitive development, (b) for taking advantage of this last major opportunity to correct deficits of undernutrition and “catch-up” to normal life course development, and (c) for addressing the nutritional inadequacies and mitigating the longer-term consequences of overnutrition. This review summarizes and provides a rationale for prioritizing nutrition in school-age children, and for the need to revisit priorities and focus on this part of the life cycle to maximize individuals’ potential and their contribution to society.
The last three decades of academic and public health efforts have enthusiastically embraced the importance of early life nutrition as a foundational component of lifelong health. The gestational period through the first 2 years of age (the first 1000 d) and early childhood through 5 years of age have received justified attention over the last few decades. However, the ultimate realization of an individual’s potential requires a successful bridging from early childhood to adulthood. The subsequent periods in the life cycle—5 years to 9 years of age, referred to as “middle childhood,” and 10 years–15 years, “early adolescence”—are commonly encompassed in the “school years.”
Middle childhood and early adolescence bridge the period between the relatively steady growth occurring from 2 years to 5 years of age and the final maturation period of late adolescence to adulthood. This period is characterized by multiple dramatic inflection points in the course of growth and development, as well as behavioral and psychosocial events occurring around the arrival of puberty. These inflections represent transformational changes in the brain and cognitive processing, linear bone growth and bone mineralization, body composition, and other organ systems. It is also during this period that major sex-driven inflections and divergences occur in growth and development. The nutrition of children during this period is critical for supporting these changes. In addition, can help overcome early deficits, and may help correct dietary excesses that have been occurring since infancy. Thus, school age constitutes a final major window of opportunity to influence growth and development, and the associated health consequences in mature life.
Unfortunately, relative to other life stages, school-age nutrition has received a disproportionately low level of scientific attention, in part due to a misleading but widespread perception that early deficits in growth and development cannot be rectified. In the last few years, scientific, public health, and other academic voices have been calling attention to this life stage as a critical and potentially last major window of opportunity for intervention in maximizing the potential of individuals as productive members of society. 1–5
This aim of this review was to highlight the critical growth, developmental, and nutritional aspects of these transformative school-age years, and the challenges and gaps in knowledge around these, and to provide arguments for why nutrition during school age deserves greater and more focused attention to maximize individuals’ growth, development, and ultimate productivity.
To achieve this aim, a comprehensive review of the literature was conducted, using PubMed to identify eligible and relevant publications through 2021. Papers were identified by combining the following Medical Subject Heading keywords: children, school age, middle childhood, adolescence, nutrition, nutrients, growth, development (multiple aspects/organ systems), malnutrition, stunting, overweight, and obesity. Literature was selected and prioritized that included information and data for the 5–15-year age group, primarily based on population, cohort, or epidemiologic studies and reviews, as well as literature addressing biologic aspects of specific areas of growth and development for this age group, with a focus on somatic growth, body composition, and neurologic development. Nutrition- and diet-related behavioral, psychologic, or social aspects were not included in the scope of this review.
Compared with the nutrition and health research literature for other life stages, there is a historical neglect of middle childhood and adolescence. Estimates of the published literature describing child health (PubMed sources 2005–2016) show 95.3% of this literature is dedicated to early childhood (<5 y), 3.5% to 5 years–9 years, 0.55% to 10 years–14 years, and 0.61% to 15 years–19 years. 6 The health and nutritional status of school-age children, particularly that during middle childhood, remains the least studied of all life stages.
Public databases of most agencies track rates of malnutrition, stunting, and other health markers for children, but usually do so only until 5 years of age, and only pick up again during adolescence or adulthood. 7 Regional or international databases of nutritional data for middle childhood (5 y–10 y of age) are extremely scarce. Many reviews for this age group rely on extrapolations, eg, using Demographic and Health Surveys (DHS) data for children 4 years–5 years of age 8 or including data of 10-year-olds to 14-year-olds within child surveys. 9 On the other end of school age, most research and data for children 10 years–15 years (early adolescence) is sometimes conflated with the data of adults, eg, Multiple Indicator Cluster Surveys (MICS) and DHS data for females 15 years–19 years. As discussed below, research, particularly concerning child growth and cognition, led to the notion that the consequences of nutritional and environmental insults in the first 2 years of age were irreversible. This may have resulted in reduced interest and research bias, due to underestimating the significant potential for growth and developmental catch-up possible during middle childhood and adolescence.
In part, inadequate research in this age group is also due to ambiguity, inconsistency, and overlapping terminology, resulting from viewing this age group through different lenses: physiologic, reproductive, social, legal, or school system, etc. Terms such as “early childhood,” “middle childhood,” “late childhood,” “school age”, “adolescence,” and “young adulthood” often overlap. From the general physiologic point of view, “middle childhood” (ages 5 y–9 y) is a period of growth and consolidation, followed by an adolescent growth spurt (ages 10 y–14 y), each associated with specific behavioral changes, before a final growth consolidation (ages 15 y to early 20s), and subsequent maturation into adulthood. 1 More broadly speaking, the developmental stages in the life cycle have been classified into 3 main categories: physical growth, cognitive development, and socioemotional/psychosocial development. 10 And while interdependent, the rate of progress for each of these life-stage categories can vary individually, making it hard to propose a purely chronological or age-based approach.
Many organizations and legal systems define “child” as an individual 0 years–18 years. 8 , 11 WHO defines an “adolescent” as aged 10 years to 19 years, “youth” in general as 15 years–24 years, and “young people” covers 10 years–24 years. 2 , 12 More recently, a broader definition for “adolescence” has been advocated as including the entire 10-year-old to 24-year-old group within the term. As explained by the 2016 Lancet Commission on Adolescent Health and elsewhere, 9 , 12 this would support consideration of appropriate social and economic policies, service systems, and legal frameworks for this broad age group. While useful for certain objectives, this approach fails to distinguish the significant differences between the transitional aspects of development (and therefore the distinct difference in needs) of early adolescence versus late adolescence. Others support the use of “young people” (not “adolescents”) as a term for all 10–24-year-olds, distinguishing “adolescents” (10 y–19 y) from “young adults” or “emerging adults” (20 y–24 y). And some suggest that considering people in their early 20s as adolescents could lead to underestimating their competencies and capabilities. 13 Clearly, no definition should be rigid. Approaches to defining “school age” and “adolescence” can vary by setting and should consider the cultural and societal context.
Schools are a significant platform, not always adequately utilized, for delivering nutrition as well as education in nutrition. “Schooling” plays a role as a defining factor in a person’s development, includes what is generally called “primary” and “secondary” schooling, and is quite variable from country to country. Globally, most children in primary school are between 5 years and 14 years of age, and there tends to be late entry into school in low- and middle-income countries. Many consider that “high school” and “preparatory school” fall into this category; others do not. Schooling provides opportunities for promoting nutrition and health. Research and interventions can leverage society’s investment in education and take advantage of the potential synergy between health and education investments. 1 , Figure 1 summarizes the terminology most commonly used for childhood growth and developmental stages. Acknowledging there is no perfect life-stage categorization, given the physiologic and growth changes, most agree that data should be disaggregated for 5 years–9 years (middle childhood), 10 years–14 years (early adolescence), 15 years–20 years (late adolescence), and 20 years–24 years (older adolescents or young adults). 1 , 9 ”School age” defined as comprising “middle childhood” (5 y–9 y) and “early adolescence” (10 y–15 y) will be the age group of focus and the terminology used in this paper.

Major developmental life stages (in gray) and commonly used terminology for specific developmental stages as related to age . Modified and adapted from Bundy et al 2017 1 and Sawyer et al 2018 9
What makes school age of particular significance nutritionally is that it encompasses numerous changes in trajectory from the relatively steady growth of the preschool child, through sex differentiation, and into the final consolidation period of late adolescence. These changes are driven by pubertal onset and course, with population variations primarily dependent on genetic, environmental, and nutritional factors. Pubertal sex hormone secretion will also determine changes in growth rate and growth termination. However, much work still remains to be done in understanding the underlying genetics, the timing of puberty (including early-life determining factors), growth variability during puberty, and adiposity and weight gain. 14
Two specific processes contribute to the sex-differentiating physical developmental changes during this period: adrenarche and gonadarche. Adrenarche occurs between 6 years and 8 years of age, earlier in girls and later in boys, and refers to the maturation of the adrenal cortex and increased secretion of adrenal androgens, namely dehydroepiandrosterone. It is involved in the development of pubic hair (pubarche), body odor, skin oiliness, and axillary hair. Gonadarche is initiated by specialized neurons of the hypothalamus that secrete gonadotropin-releasing hormone (GnRH) in a cyclical pattern that regulates the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) by the anterior pituitary, leading to gonadarche, starting at around 9 years–10 years of age in girls, and around 10 years–12 years in boys. In girls, FSH stimulates estrogen production, follicle formation, and eventually ovulation and menarche. In boys, LH stimulates testosterone production and eventually maturation of spermatozoa.
Finally, these changes during middle childhood and early adolescence are directly related to a differentiated phase of social learning and experimentation, heralding shifts in cognition, motivation, and social behavior, with significant implications for the ultimate development of each child’s personality. These shifts encompass major domains such as the development of independence and decision-making, acquisition of cultural norms, increase in complex moral reasoning, increase in understanding of social hierarchies, increase in sense of gender identity, gender segregation, and romantic attraction, as well as changes in food preferences and dietary habits, the expansion of which are beyond the scope of this paper. 15
These growth and change phenomena and influential factors are interrelated, and nutrition plays a fundamental role. Protein-energy malnutrition is associated with delayed puberty, and subsequently poor growth and development. Secular trends have changed the timing of these processes in different populations, likely reflecting nutrition and health changes in the last century. In Europe and North America, from the early 19th century to the mid 20th century, age at menarche decreased from approximately 17 years to about 12 years–13 years. 16 In China, in just the past 25 years, the mean age of menarche has decreased by 4.5 months per decade. 17 As discussed below, changes in growth patterns, particularly in height and body–mass index (BMI), are interrelated with the onset of puberty. Increases in height and BMI are associated with an earlier onset of puberty, and earlier puberty is associated with an increased rate of later obesity. 14 Obesity, which has risen dramatically in children, is associated with a shift towards earlier onset of puberty, particularly in girls; the situation is less clear in boys. 16
The course of sex hormone secretion will determine the termination of growth during late adolescence into adulthood. The pubertal process is usually complete 2 years to 4 years after physical changes begin to occur. However, physical maturation will continue into the third decade of life. For instance, bone and brain development continues into the 20 s. Hormonal differences during puberty will also affect the size and function of organ systems related to aerobic and anaerobic physical fitness. Heart size and cardiac function, lung size, bone development, muscle volume and strength, erythropoiesis, and substrate utilization will diverge and determine different ultimate fitness and strength levels. 18
Puberty happens in the middle of the school-age years and marks and determines the changes in trajectory and the switch in somatic and brain growth and development rates, which characterize this part of the life cycle. Two significant phenomena arise in this period:
Several inflection points and trajectory changes occur in somatic and brain growth and development, at different time points, for various measures of development (eg, height, adiposity, lean mass accretion, bone mineralization, brain growth and reorganization, with subsequent cognitive development, and secondary sexual characteristics) and social and behavioral changes
Sex divergences appear or become significantly more pronounced in these measures.
The dynamic somatic, cognitive, and behavioral changes that occur during school age underscore the importance of preparing children during middle childhood and facilitating their transition into adolescence during this period. Figure 2 shows the changes in trajectory for key anthropometric changes during the school years.

Growth trajectories in school-age years (gray-shaded area) . Fat and fat mass: estimates. All others are medians . Compiled and adapted from Tanner and Davies 1985 24 (height velocity), Weaver et al 2016 33 (BMC gain), Veldhuis et al 2005 21 (fat and fat mass), US CDC 19 (BMI). BMC: bone mineral content; BMI: body–mass index
Body composition
Although height velocity decreases during the preschool years, height gain remains relatively steady, and the amount of body fat remains relatively constant; therefore, most children in middle school will appear slimmer than when they were toddlers. In fact, median BMI will be at its lowest in life at about 5.2 years in girls and at about 5.75 years in boys, ie, just as they enter school age. 19 During this period, a child’s adiposity (corresponding to an increase in number of adipocytes) will rise, giving way to what is called the “adiposity rebound” or second rise in BMI during life. BMI, a reflection of adiposity, is the first anthropometric inflection point to appear in the school-age years. 20
The age at which this inflection happens is inversely proportional to their BMI percentile (children with higher BMI will rebound earlier). Furthermore, an earlier adiposity rebound is associated with a higher risk of later obesity. As mentioned above, secular trends show an interplay between nutritional status and puberty. In addition, overweight and obesity in girls will lead to earlier puberty. Boys, however, show a less clear pattern: overweight boys seem to mature earlier, but obese boys mature later. The mechanisms are not yet clear, and there appears to be a bidirectional influence between puberty and weight gain. 16
Body compositional changes during the school years also mark significant changes in trajectory and sex divergence. Large-scale normative data for body compositional changes for middle childhood and early adolescence are lacking, although some estimations and extrapolations have been done. Fat mass, fat-free mass, and percentage body fat have been estimated by aggregating data from several cross-sectional analyses from European and American populations. 21 During the preschool years, actual fat mass in kilograms is similar in both sexes. Between 5 years and 10 years, girls will accumulate fat mass faster than boys, gaining approximately 6% (2 kg) more than boys. After this, with the onset of puberty, girls will gain about 1.14 kg of fat, while boys will maintain a relatively fixed fat mass. Throughout the school years, until 15 years, girls will have increased their fat mass almost 5-fold, while boys will have increased theirs by around 3-fold. Ultimately, fat mass will increase from 10%–12% of body weight at birth to approximately 15% in young men and approximately 25% in young women. In boys, after a prepubertal increase in percentage body fat, this percentage actually declines with puberty and stabilizes with maturation. 21 The rate of accumulation of fat-free mass (including muscle mass) remains comparable by sex until the onset of puberty. With the onset of puberty, boys will accumulate lean mass significantly faster and for a longer period than girls. Gains in adipose tissue are primarily driven by an increase in the number and size of fat cells, while muscle development happens mainly by an increase in muscle cell mass (hypertrophy). The increase in body weight gain during puberty is mainly attained through an increase in lean tissue in boys.
Skeletal muscle mass, which represents about 25% of body weight at birth, will increase to 40%–45% body weight in late adolescence. 18 , 20 Girls will reach adult stabilization by 15 years–16 years, while boys will do so by 18 years–20 years. 21 Skeletal muscle mass has been estimated for children of school age using appendicular lean tissue mass extracted from dual photon absorptiometry measurements 22 and bioelectrical impedance. 23 Both approaches show that muscle mass and rates of gain are similar in both sexes until middle childhood. At around 5 years of age, boys maintain a slightly higher muscle mass, and girls a higher fat mass, after which trajectories increasingly diverge. This results in an approximately 3.5–5-fold increase in muscle mass in boys and a 3–4-fold increase in muscle mass in girls between 5 years and 15 years, in part depending on the methodology used. Conversely, fat mass will increase more in girls than in boys during this period.
Height and linear bone growth
The increase in height gain is the most noticeable change in trajectory in anthropometric measures of the school years. About 40% of an individual’s linear growth will occur during this time. Based on the United States CDC growth curve medians, by 5 years of age, boys and girls will, on average, be at 61% and 65%, respectively, of their ultimate height. By 15 years, they will be at 96% and 99%, respectively of ultimate height. 19 There are major differences between the first 5 and second 5 years of school age.
During middle childhood, height velocity actually decreases, to the lowest levels of the entire life cycle, only to quickly increase in the middle of the school years to the highest rate of linear gain of all post-infancy years. In North America, CDC growth velocity charts 19 show median height velocity will be at its lowest since birth just before 9 years of age in girls and at approximately 10.5 years in boys. At that point, before the puberty-related acceleration, both girls and boys will have reached ∼80% of their final height. Thus, height at that point will be a strong predictor of ultimate height in most individuals. This speaks to the importance of adequate nutrition and sustained growth between 5 years and 10 years of age.
With the onset of puberty, height velocity rapidly increases. In early adolescence, median peak height velocity in girls reaches its peak at around 11.5 years of age, with growth rates similar to those at 2 years of age (∼8.3 cm/y). In boys, a peak growth rate of about 9.5 cm/year happens at around 13.5 years of age, surpassing the 2 years of age rate of height attainment. 24 In girls, this growth spurt starts earlier (∼9 y in girls vs ∼10.5 y in boys) and ends earlier (∼11.5 y vs ∼13.5 y), lasting at least 0.5 years less than in boys. The ultimate median height in males will be greater due to greater height at the onset of puberty (boys ∼9 cm–10 cm taller than girls), a more prolonged growth spurt period, and a greater increase following pubertal onset (boys gaining ∼3 cm more than girls between the onset and end of the growth spurt). The pubertal growth rate declines rapidly after their gender-specific peak in both sexes, to 1 cm/year or less after 14.5 years in girls and 17 years in boys. 21 , 24
Height gains are dependent on longitudinal bone growth determined by epiphyseal growth plate function. Growth plate chondrocytes proliferate by mitosis, mature, become hypertrophic, lengthen the bone, and ultimately replace osteoblasts to form new calcified bone tissue. Growth hormone and insulin-like growth factor are the key hormonal drivers of this process. Adequate nutrition is critical for providing substrates for epiphysial growth, particularly energy, protein, and zinc. Calcium and vitamin D may play lesser roles in longitudinal bone growth. Very importantly, independent of nutrient provision, bone growth regulation can be blocked by corticosteroids and inflammatory cytokines. Chronic inflammation from infection, environmental factors, autoimmune disease, and the use of corticosteroids can all curtail linear bone growth. In addition, inflammation can lead to insulin and growth hormone resistance, which can further inhibit linear bone growth, thus compounding the effect of undernutrition, as often occurs in underserved populations. 25–27 As discussed below, poor linear growth and stunting (two standard deviations beyond the normal curve median) remain the most prevalent clinical manifestation of undernutrition globally. 28
Bone mineralization
Linear bone growth is followed by increases in bone mass and bone mineralization. Bone matrix becomes mineralized with the deposition of calcium phosphate nanocrystals (carbonated hydroxyapatite). The degree of deposition will determine bone mineral content (BMC), measured in grams, for a specific skeletal location or for the total body. This sequence of events will be similar, with variations by sex.
Total BMC will rapidly increase in early adolescence. Data derived from North American individuals show that by the end of middle childhood, prior to the onset of the growth spurt (2.5 y to 3 y before peak height), children will have achieved 37%–40% of ultimate total body BMC. In the short period between the 2 years before and 2 years after peak height is attained, another 39% of ultimate BMC is accrued. By the end of school age, more than 80% of total body BMC will have been attained, and final total body BMC appears to plateau at around 18 years of age in girls and 20 years in boys. 29 , 30
Similar to height gain, the BMC accretion will increase rapidly with the onset of puberty, and the median peak rate of BMC accretion will occur at around 12.5 years in girls and 14 years in boys. Thus, the peak BMC accretion rate will lag compared with the peak height velocity, which occurs at around 11.5 years and around 13.5 years in girls and boys, respectively. Therefore, there is a transient decrease in bone density relative to height and bone elongation, and consequently an increase in bone fragility lasting about 12 months in girls and 6 months in boys (see Figure 2 ). This may partially explain the higher rate of forearm fractures reported in girls between 8 years and 10 years, and in boys between 10 years and 12 years. 30 , 31
Ultimate bone mass, measured as bone mineral density (BMD) or mineral content divided by bone area, will depend on genetic and environmental factors. Studies in twins suggest that genetics can explain 50%–85% of the variance in peak bone mass, with multiple genes being involved, some of which may interact with environmental factors, including diet. 32 Thus diet and “lifestyle” factors, including exercise, can still significantly influence BMC and BMD. As stated above, middle childhood and early adolescence are the periods of fastest mineral accrual, and more than 90% bone mass is achieved by 18 years–20 years. By the late 20s, bone mass will begin a gradual process of decline, leading to varying degrees of osteoporosis, which can only partially be modified by diet and other environmental factors. It follows that school age becomes a critical age of intervention and “investment” in bone health by maximizing peak bone mass and decreasing the risk of fractures in later life. This includes optimizing nutrition, particularly provision of protein, calcium, and vitamin D, as well as activity and exercise during this life stage. 31 , 33
Brain and cognition
Brain size increases by 4-fold during the preschool years, reaching approximately 90% of adult volume by age 6. 34 However, brain development will be a continuous process with age-specific phases until adulthood. The growth rate of cortical gray matter peaks during school age, by 10 years–12 years of age. Cerebral white matter volume increases through school age until mid-to-late adolescence, peaking by 18 years–20 years. 35 , 36 Total brain size is about 9% greater in males than females, and the difference persists, even if controlling for height and weight. These differences should not be understood as conferring advantage or disadvantage, as they do not represent neuronal or synaptic connectivity or other components of brain architecture and function (see Figure 3 ). 37 , 38

Neuromaturational and cognitive development trajectories in school-age years (gray-shaded area) . Compiled and adapted from Peterson et al 2021 38 (brain and gray matter growth), Tapert and Schweinsburg 2005 114 (neuromaturation process rate), Lee et al 2014 115 (brain region development), and Anderson 2002 46 (cognitive development executive domains)
During the school years, though at a slower rate than during the preschool years, total brain size increases, as does the sex-driven divergence, with boys being faster and peaking by 14.5 years, and girls peaking earlier by 11.5 years. 37 During this period, brain development is also marked by a significant increase in 2 major neuro-maturational processes: continued myelination and an increase in synaptic refinement and pruning, both of which are important for the efficiency of neuronal networks. Dendritic synaptic pruning eliminates unused or weak connections, and a reduction in myelination rates improves connectivity. This fine-tuning within and between brain regions strengthens a number of particular pathways, which increases brain efficiency, critical to the development of cognitive abilities. 39 , 40
School age will be marked by the highest rate of development of specific areas of the brain, particularly the posterior sensorimotor cortex, temporal association complex, and prefrontal cortex, and this development peaks at between 5 years and 15 years of age, in the middle of school age. All these areas are “associative cortices,” which process input from the sensory cortices and ultimately generate behaviors (see Figure 3 ). These structures are the key determinants of higher-order functions, particularly cognitive development (including language, mathematics, and executive function [EF]) and socio-emotional regulation, which among other things, allows for organization of information to serve goal-directed behaviors, decision-making, peer affiliation, and social behaviors. 41 , 42 The parietal and temporal association cortex, responsible for language skills, also develops at a fast rate and this development peaks during school age. For example, language acquisition and proficiency, especially the ability to master a second language as a native speaker, decreases at the end of school age, by 15 years of age. 43
The development of the prefrontal cortex peaks in the middle of the school years and continues to mature into the third decade. The gray matter volume in the frontal cortex peaks at 11 years of age in girls and at just after 12 years in boys. 44 This part of the brain supports higher-level integration and processing, allowing for abstract thinking, problem-solving, understanding others’ thoughts and intentions, and the relating of thoughts temporally, allowing for goal setting. Thus, the prefrontal cortex is generally regarded as the “seat” of EF. EF is a broad term that incorporates a collection of mental processes that (a) enable individuals to hold and recall relevant information (working memory), (b) focus their attention, inhibiting automatic responses to stimuli (inhibitory control), and (c) shift the focus of attention to the managing of problems or multiple-aspect tasks successfully (cognitive flexibility), to yield purposeful, goal-directed behaviors. Ultimately, these processes influence behavior, emotional control, and social interaction. EF is associated with academic performance as well as intelligence quotient (IQ). 42 , 45 , 46
One well-recognized model of EF conceptualizes and maps chronologically 4 distinct and interrelated developmental domains, each of which gathers and processes stimuli from multiple sources: attention control, information processing, cognitive flexibility, and goal setting. Attentional control matures relatively early, by the end of preschool age; information processing and cognitive flexibility are mostly developed by the end of middle childhood; and goal setting is well developed before the end of early adolescence (see Figure 3 ). 46
In addition, the increased synaptic pruning and myelination that occurs during this period significantly reshapes and modifies circuitry and allows malleability and adaptation to environmental experiences, or brain plasticity. There is evidence, eg, that both synaptic pruning and myelination are driven or modified by an individual’s experiences. 47 Thus, behaviors toward the environment are shaped by biologic changes in the brain, which in turn may be shaped by environmental, social, and cultural learning experiences. School age marks a major development of the associative brain regions and the resulting cognitive development and EFs, as well as the maturation of reward and emotional sensitivity areas, which interact with higher function control areas to develop emotional regulation, identity development, and longer-term planning and purpose. Adequate provision of nutrition, healthy social interactions, and cultural experiences, as well as adequate sleep, are all key to physical and psychosocial well-being. 41
The onset of early adolescence will be marked by an increase in social and cultural interactions, and changes in the home, community, and school relationships, which influence behavior. The interaction between behavior resulting from brain functions and external influences appears to be bidirectional. At the onset of puberty, the prefrontal associative brain areas continue to develop, but at a slower pace than some subcortical brain areas. These limbic emotion- and reward-related regions, such as the amygdala, appear to mature earlier than the prefrontal areas, which are responsible for inhibitory control of impulses and regulation of gratification and other emotions. This “mismatch” may in part explain the increase in risk-taking, emotion-driven behaviors seen in adolescence. 48
In summary, between the age of 5 years and 15 years, children go through major accelerations and inflections in their somatic growth, from a prepubertal state in the first 5 years to early adolescence changes in the next 5 years. By the end of school age, and before entering the final stages of “late adolescence,” healthy boys and girls, respectively, will have attained approximately 96% and 95% of their adult height, 19 92% and 77% of their total BMC, 49 89% and 85% of their fat mass, 21 and 84% and 95% of their muscle mass. 22 During this period, neuro-maturational processes will have also undergone significant changes. These include peaks in the development of specific areas of the brain and particularly the prefrontal cortex (implicated in complex cognitive behavior, planning, personality expression, decision-making, and moderation of social behavior) in the middle of the school years. Processes like synaptic pruning, which increase brain efficiency, will also peak by the end of this period, allowing for plasticity and increased brain efficiency. Delaying, altering, or blunting these accelerations and inflection points can significantly affect the ultimate attainment of physical growth, and cognitive, and socioemotional/psychosocial development. The necessity of preparing the child for these changes and supporting them through these accelerations and inflections, leading to the final maturational phase of late adolescence and ultimately adulthood, cannot be overstated.
The number of changes and dynamics of development mentioned above make the school years a particularly sensitive time, especially since most of the final growth and development is attained, which if not achieved will limit physical, cognitive, and social potential. These changes happen against a genetic backdrop expressed in, and dependent upon, multiple environmental and social scenarios that modulate physical and psychosocial development.
All these changes are underpinned by adequate nutrition in this period, as is true for all life cycle phases. Inadequate nutrition will slow or blunt physical and neurocognitive development trajectories during this last period of growth and development, with long-term consequences, inhibiting an individual’s ultimate potential. If environmental conditions, particularly nutrition, are favorable, the growth course and final height and overall body shape will be determined by an individual’s genes. 27 The acceleration and change in growth trajectories discussed above increase the chances for curtailing growth and development if increased nutritional demands are not met. Because of the growth dynamics in this period, the school years become critical for the necessary nutrition (a) to maintain adequate growth trajectories until maturity, or (b) to correct inadequacies and imbalances (deficits and excesses) for a healthy transition to a productive adulthood.
WHO, the US Institute of Medicine, the European Food Safety Authority (EFSA), and other regional authoritative groups all distinguish and define specific energy, macro-, and micro-nutrient requirements for the school-age years (early childhood and early adolescence) distinct from those of other life stages.
Energy and protein
As the child grows, changes in metabolism are directly related to total energy requirements and indirectly to growth, and consist of basal metabolic rate, energy cost of growth, and activity energy expenditure. 50 As a fraction of the total energy requirements, the energy cost of growth is highest in the newborn period, decreases to about 3% at 1 year of age, and goes up again between middle childhood and early adolescence to about 4%. 51 Imbalances between energy intake and expenditure can result in deficits (leading to a decrease in body fat and a deceleration of growth) or excesses (in the form of fat accumulation, increased body weight, and its related consequences).
The factors that affect child energy requirements are growth and body composition (which are sex-dependent), as well as physical activity. Daily energy requirements diverge by sex at the start of school age, and will remain different throughout the life cycle. Sex differences in metabolic rate and energy expenditure are in part driven by differences in body fat and fat-free mass that emerge during school age.
Between 5 years and 15 years of age, physical activity is a particularly important factor in energy balance. In adults, the estimated difference in energy requirements between a sedentary individual and an active individual is below 20%, while in 5-year-olds to 15-year-olds it is around 35%, indicating the need for adequate energy provision—in proportion to the recommended “active” level of physical activity during this period of the life cycle. 51 Energy provision throughout the day is also critical for brain activity, where increased neuronal activity drives increased energy consumption. In addition to all the neurodevelopmental changes occurring during school age mentioned above, the cerebral metabolic rate of glucose utilization is at its highest in middle childhood and early adolescence (apart from during the newborn period), then drops towards the end of adolescence. The mature brain is only approximately 2% of the body weight in adulthood, but is responsible for around 20% of energy consumption. Estimations for 12-year-old children suggest that brain energy consumption is as high as 30%. 52–54 Lastly, this increase in energy requirement and utilization is also dependent on the presence of adequate quantities of several micronutrients. These include riboflavin (vitamin B2), niacin (nicotinamide; vitamin B3), pyridoxine (vitamin B6), cobalamin (vitamin B12), vitamin C, vitamin D, calcium, iron, and phosphorus. They all act as co-factors for key enzymes in the metabolic pathways that generate and use energy.
Protein is the major functional and structural component of every cell in the body. The quality of a source of dietary protein depends on its ability to provide the nitrogen and amino acid requirements necessary for the body’s growth, maintenance, and repair. Through to the end of the growth years, enough protein is required to maintain the nitrogen equilibrium plus protein deposition in tissues. Low consumption of protein, often associated with low protein quality, is strongly associated with stunting, and if marked, other signs of undernutrition. As opposed to requirements for energy and some micronutrients, protein requirements do not change significantly by age or sex during the school years. The United States recommended dietary allowance is 0.95 g/kg/day, representing 10%–30% of total calories, from 4 years to 13 years of age. The recommended dietary allowance decreases slightly after adolescence. In general, proteins from animal sources such as meat, poultry, fish, eggs, milk, cheese, and yogurt provide all indispensable amino acids and are referred to as “complete proteins.” Proteins from plants, legumes, grains, nuts, seeds, and vegetables tend to be deficient in one or more of the indispensable amino acids.Thus, attention needs to be paid to children whose diets are low in animal protein sources to avoid essential amino acid deficiencies. 51
Micronutrients
In the United States, the Estimated Adequate Requirements, and Dietary Reference Intakes for micronutrients are the same for all children up to age 8 years. For the first time, they diverge for boys and girls during the school years: there are small differences (eg, for iron) for 9 years–13 years, and larger differences in requirements for late adolescence, at 14 years–18 years. 51 EFSA has slightly different and more specific age cut-offs for Population Reference Intakes (PRIs) for most vitamins and minerals. 55 Recommendations are made for 4 years–6 years, 7 years–10 years, 11 years–14 years of age, and separately define PRIs for 4 years–10 years and 11 years–17 years for calcium, 1 year–6 years, 7 years–11 years, and 12 years–17 years for iron, and 3 years–9 years and 10 years–17 years for copper, with some differences for sex in these nutrients. EFSA also differentiates requirements in energy and protein for boys and girls starting at 4 years. While specific benefits have been well established in relation to deficiencies for many micronutrients, consensus on optimal doses and combinations of these nutrients for promotion of specific health benefits in otherwise healthy school-age children is not universal and would benefit from further clinical research and substantiation.
Linear growth appears particularly sensitive to restrictions in energy, protein (particularly essential amino acids), zinc, iodine, and phosphorus, as well as some electrolytes. Protein quantity and quality remain fundamental components of adequate growth and function at all ages. Yet, the minimum protein necessary for adequate linear growth remains to be ascertained. Animal proteins, including dairy protein sources, have a selective effect in promoting height gain in undernourished and well-nourished children. In populations with low consumption of foods from animal sources, protein and zinc deficiencies will be more common. While iron and vitamin A are essential for multiple other reasons, intervention studies suggest that their deficiency does not affect linear growth. As discussed further below, calcium is critical for bone mineralization but appears to be of less consequence regarding linear growth. 27
Independent of nutrient provision, as mentioned above, bone growth regulation can be blocked by inflammation, such as recurrent childhood infections, which, if bi-directionally compounded by undernutrition, result in poor growth led to stunting. The term “environmental enteric dysfunction” has been used to refer to chronic and recurrent infections and infestations in areas with poor sanitation, where infection, inflammation, and malabsorption coalesce and perpetuate undernutrition. These conditions may explain why nutrition or dietary interventions alone may not be sufficient to address stunting in children. Current interventions to reduce stunting need to target sanitation and environmental factors as well as nutrition in low- and middle-income country settings. 25 , 27
Calcium is essential for adequate mineralization of bones, and 99% of all calcium in humans is found in bones and teeth. Dietary calcium can be absorbed passively, but the active transport of calcium in the gut is mediated by vitamin D. Both nutrients are inextricably linked in determining BMC. Low calcium intake in young children is associated with low BMC, and sustained low intakes (below 200 mg daily) with radiographic signs of rickets. 56
There is clear evidence suggesting that peak bone mass and risk of fractures in later life are influenced by bone mineral accretion throughout childhood, including school age. As discussed above, peak rates of bone mineralization are reached 6 months–12 months after the peak rate of bone elongation is reached. By the end of school age, median peak height has been achieved in girls (achieved a year later in boys), and more than 80% BMC has been accrued. The exact cessation of mineral accrual varies depending on the skeletal site, but appears to be complete by 18 years in the spine and femoral neck. After peak BMC is reached, the rate of bone mass and mineral content accretion gradually and continually decreases for the rest of an individual’s life. 33 , 57 Therefore, the rate and amount of BMC attained in the school years will greatly determine peak bone mass and be a major contributor to the relative risk of low bone mass and eventual osteoporosis and bone fractures for the rest of an individual’s life. Recent estimates from the United States in adults older than 50 years show a prevalence of low bone mass of 51.5% in women and 33.5% in men, and frank osteoporosis of 19.6% in women and 4.4% in men. 58 Estimates from the International Osteoporosis Foundation indicate that, worldwide, after 50 years of age, 30% of women and 20% of men will have hip, vertebral, or wrist fractures from osteoporosis in the remainder of their lives. 59 Thus, meeting dietary protein and calcium requirements, maintaining adequate vitamin D through diet and sunlight exposure, and physical activity during school-age years constitute critical investments in achieving long-term bone health. 31 , 60
Iron, zinc, polyunsaturated fatty acids (especially docosahexaenoic acid), vitamin B12, and folate have all been specifically identified as critical nutrients for adequate brain growth, cognition, and EF development. However, as for other aspects of life-stage nutrition, most data have been accumulated for these nutrients and their longer-term effects in relation to consumption in the first 5 years of life. They have often not been the primary focus of studies and are poorly investigated in healthy school-age populations. 61
Deficiency in iron deserves highlighting in relation to nutritional consequences for later life, due to its prevalence in and coexistence with all forms of malnutrition. Iron deficiency is the most common nutritional deficit in people worldwide and the most common deficiency in children, whether suffering or not from acute or chronic malnutrition. Anemia, half of which is due to iron deficiency, affects around 33% of the global population. Globally in 2019, iron deficiency was the leading cause of years lived with disability in children and young adults (aged 10 y–24 y), with the highest prevalence in most African and many Asian countries. 62 While its prevalence is higher in low- and middle-income countries, it persists in varying degrees in all socio-economic levels. Iron is a crucial nutrient in maintaining levels of neurotransmitters, including dopamine and serotonin. And its deficiency can decrease brain myelination, alter synaptogenesis, and decrease the functioning of basal ganglia. The consequences in childhood include deficits in motor function and impaired cognitive development, leading to lower cognitive skills, lower school achievement, impaired psychomotor and behavioral development, and ultimately lower work capacity and productivity in adulthood. 63 , 64
The consequences of iron deficiency in childhood, some of which may be irreversible, have been recognized for a long time and have led to global efforts in improving iron status through supplementation in infancy and childhood. 64 , 65 Given the significant changes in brain structure and function that happen during the school years, and the potential long-term consequences of deficiency, iron remains a major nutrient of interest, highlighting the need for adequate preventive interventions as well as treatment of deficiencies during this life stage. There is increasing and robust evidence that improving iron status, particularly in the presence of anemia, significantly affects cognitive performance in school-age children older than 5 years. Interestingly, the evidence for this effect of iron on older children appears stronger than for interventions in children under 2 years of age. 66
Consequences of inadequate nutrition in school age on growth and development
Inadequate nutrition in school age ultimately results from inadequate diets, which in turn are a consequence of multiple factors. On the one hand, food security, availability, and provision are essential. On the other, a healthy diet requires appropriate food choices, which depend on many environmental influences—from home, the community, the school, and broader society. These influences will not only determine the delivery of adequate foods but shape the behavior of children and thus their food choices for the long term. Influences at this age are critical, when cognitive, socioemotional, and psychosocial development are associated with increasing independence, decision-making, and self-image and awareness. Addressing all these factors remains critical for increasing an individual’s chances for long-term health. Discussion of these is beyond the scope of this review.
The immediate and most visible consequences of not meeting nutritional requirements are loss of body weight and adipose tissue (thinness/wasting/low BMI). Prolonged marginal provision of macronutrients, most often accompanied by micronutrient deficits, leads to slowing of linear growth (low height for age). In both cases, infection, or other inflammatory states, coupled with enteropathies related to poor sanitation, can further increase requirement for an effective immune response, lead to a negative nitrogen balance, mobilization of protein from muscle tissues, as well as inhibition of linear bone growth. 25 , 28 Wasting and stunting are often linked and can occur together in the same population, often in the same child. 67 Longitudinal analyses show that wasting is a precursor to stunting. 68 In addition, low BMI and wasting are related to delayed pubertal onset, which in school-age children affects growth trajectories. Globally, stunting (height-for-age greater than 2 standard deviations below the WHO reference) remains by far the most prevalent clinical manifestation of undernutrition, including micronutrient deficiencies. 28
Stunting in early life is associated with poor cognitive development, lower development of EF, lower rates of schooling and school achievement, and ultimately decreased productivity and earning power. These associations, however, do not necessarily infer causality. Stunting is often accompanied by multiple nutrient deficiencies and their consequences, beyond iron deficiency anemia. And the occurrence of stunting due to poor nutrition, and its cognitive and other consequences, cannot be delinked from the effects of the physical and social environments where stunting occurs 69–71 ; nonetheless, it is likely they are causally related. Beyond cognitive impact, not achieving an individual’s height potential can also be associated with higher psychologic dysfunction all the way to late adolescence, with increased chances of developing low self-esteem, anxiety, depressive symptoms, and anti-social behaviors. 72 , 73
Stunting can occur at any age before adulthood, but for most school-age children, it is a continuation of poor growth in early infancy. WHO and World Bank global estimates show that globally, stunting in children under 5 years of age has decreased from 33% (203.6 million children) to 22% (149.2 million children) from 2000 to 2020, 7 with the highest prevalence in Africa and parts of Asia and Latin America. Thus, a great number of children are stunted when entering school age. Stunting prevalence in school age will result from stunting occurring under 5 years, with some “new” cases being added or a decrease in cases from “catch-up” growth. 74 Although most stunting may start in infancy, it can continue or worsen in the school years. As discussed below, given school age is the last and second fastest period of height attainment after infancy, this life stage may offer the last “window of opportunity” for correcting deficits and potentially achieving catch-up growth and catch-up cognitive development, ameliorating its negative consequences for individuals and society.
Lastly, children who remain stunted through school years may be at increased risk for obesity. There is growing evidence that stunted infants and children who gain weight rapidly in later childhood have an increased risk of overweight, obesity, and noncommunicable diseases as adults. 75 , 76 However, stunting at 1 year alone does not seem to raise obesity risk consistently. 77 This is becoming increasingly important, as the secular transition from undernutrition to obesity is accelerating in many populations, as discussed below. The peak incidence of obesity by age has been occurring earlier and earlier in life in many populations (see below). Its consequences (related to metabolic disease, diabetes, cardiovascular disease, and other noncommunicable conditions) constitute the greatest health challenges of this century.
Specific nutrient deficiencies, individually or in combination, and their syndromes are both present and prevalent in school age. The consequences of these in addition to those mentioned above are beyond this review. Suffice it to say that persistent deficiencies such as of iron (and its effects on long-term cognitive function) as well as calcium and vitamin D (and their potential in preventing osteoporosis and fractures well into adult and mature life) are prime examples of the need for maintaining adequacy or correcting deficiencies during school age.
Compared with infant data, apart from some recent increase in data on the adolescent years, there is a serious lack of information on nutritional status and its consequences for middle childhood through adolescence. One analysis showed that, a literature search for 2004–2017 including the terms “health,” “mortality,” or “cause of death in the first 20 years of life” found that about 99% of the publications in Google Scholar and 95% of the publications in PubMed focused on children under age 5 years. 8 Global School-based Student Surveys, a collaboration of WHO, CDC, UNICEF, UNESCO, and UNAIDS, have primarily included only 13-year-olds to 17-year-olds. 78 In addition, data for this age group is often embedded and difficult to disaggregate from “childhood studies” that may include preschool and school-age children, or from studies on “adolescents” that include children of 10 years or 12 years and above. Overall, the ages 5 years–9 years and 10 years–14 years have the least number of research data sources for estimating morbidity and mortality risk factors compared with 0 years–5 years and 15 years–19 years. Another recent large population-based study showed that, within the relatively small amount of available data for height, weight, and BMI in school-age children, 78.9% of studies had data for 15 years–19 years, but only 50.3% had data for 10 years–14 years, and 39.9% for 5 years–9 years of age. 79 In another larger analysis, less than half of the studies included data for middle childhood (5 y–9 y), compared with nearly 90% with data for adolescents (10 y–19 y). Overall, the quantity and quality of data vary significantly by country and region. Still, the relative lack of data for middle childhood is notable across the board, limiting the capacity to compare growth or nutrition outcomes of this age group with earlier or later life stages. 80
A systematic review, one of the few studies focusing on school age (6 y–12 y) in low- and middle-income countries (LMICs), showed underweight and thinness were most prevalent (21%–36%) in South-East Asian and African countries, with lower prevalence in Latin America (8%–6%). The prevalence of overweight and obesity was highest in Latin America (∼26%), compared with 13% in Southeast Asia and 7% in Africa. The mean prevalence of iron deficiency ranged from 29% in Africa to 20% in Southeast Asia, and 14% in Latin America. Iodine, vitamin A, and zinc deficiencies are the most common. The prevalence of vitamin A deficiency was 9% in Latin America (on the lower end), to 54% zinc deficiency prevalence in Africa (on the highest end). 81
Very recently, data from population-based studies supported by the Non-Communicable Disease Risk Factor Collaboration 79 , 80 and the B&M Gates Foundation 82 are shedding light on this global picture. These are the most comprehensive reviews on growth and temporal trends available to date for this age group, and the only available review addressing this age group at a global level. One analysis, NCD RisC 2017, 79 included 31.5 million children from 200 countries aged 5 years–19 years, and estimated trends from 1975 to 2016. The other, NCD RisC 2020, 80 pooled data from 2181 population-based studies, with height and weight measurements for 65 million participants in 200 countries, and estimated trends from 1985 to 2019 in height and BMI for children 5 years–19 years. In this study, data were reported without specific cut-off points for over- or under-nutrition. Data and trends from these studies are summarized immediately below.
Thinness and wasting
From 1975 to 2016, the overall global prevalence of moderate and severe underweight (thinness and wasting) in children 5 years–19 years decreased from 9.2% to 8.4% in girls and from 14.8% to 12.4% in boys, with the expected large variations regionally. The prevalence of moderate and severe underweight remained highest in south Asia, with 22.7% among girls and 30.7% among boys in India. Although the populations increased in most regions, the number of moderately and severely underweight school-age children actually decreased. And while prevalence declined, the relatively small change at the global level was partly due to greater population growth in countries where the prevalence of underweight is higher. 79
Mean BMI trends showed increases in almost every country over the last 30 years, with the greatest increases seen in Sub-Saharan Africa. Low BMI (compared with the WHO reference median in 5-year-old children) persisted primarily in Southeast Asia and Sub-Saharan Africa. In most countries, it decreased as they entered adolescence, and in some countries it disappeared by age 19 years. 80 The trends showed that, globally, the absolute number of underweight children peaked around the year 2000 and has since been decreasing, reaching levels in 2016 close to those in 1975. 79
Data from surveys in 57 LMICs between 2003 and 2013, comprising children 12 years–15 years, showed a global prevalence of stunting of 10%. 75 However, the limited data available on stunting in this age group shows very wide variations. Stunting in adolescent girls (15 y–19 y) in LMICs range from 52% in Guatemala and 44% in Bangladesh to 6% in Brazil. 83
The 2 most extensive global studies including children 5 years–19 years of age 79 , 80 did not report height based on a particular cut-off for stunting. Nevertheless, in age-related trends, most countries showed that height was at or above the WHO median for children at 5 years of age, with girls doing better than boys. Still, in approximately 20% of countries for girls and 30% of countries for boys, the mean height during the school years was significantly below the WHO median. Today, the estimated difference in height of 19-year-olds between countries with the tallest populations (eg, the Netherlands, Denmark) and the shortest populations (eg, Timor-Leste, Laos, Guatemala, Bangladesh) was 20 cm. More concerning is that, in some countries, height adequacy in middle childhood may decrease as children grow older. Children who have optimal height at 5 years of age fall under the WHO median at 19 years by 2 cm or more, particularly in some middle-income countries.
In terms of temporal trends, with rare exceptions, the last 3 decades show significant gains in height in most countries and all regions for boys and girls, except for Sub-Saharan Africa (for both sexes) and Oceania (for boys). The greatest gains have been made in countries with emerging economies, including China and South Korea, and parts of Southeast Asia, the Middle East, and in some countries in North Africa, Latin America, and the Caribbean. 80
Overnutrition
Over the last 40 years, obesity has increased in every country in the world. The NCD-RisC 2017 study 79 showed that, from 1975 to 2016, the global prevalence of obesity in 5-year-olds to 29-year-olds increased from 0.7% to 5.6% in girls, and from 0.9% in 1975 to 7.8% in boys. The number of girls with obesity increased from about 5 million to 50 million in 2016, and the number of boys from about 6 million to 74 million. Trends in mean BMI have continued accelerating, particularly in east and south Asia. Southern African countries had the greatest rise in obesity (∼400% per decade), given the obesity prevalence was minimal 40 years ago.
On the other hand, since about 2000, the increase in prevalence has begun to plateau, and it recently flattened in northwestern Europe, in “high-income English-speaking” and Asia-Pacific regions for both sexes, in southwestern Europe for boys, and in central and Andean Latin America for girls. While not exactly comparable, these findings are consistent with another earlier large study 82 that analyzed 1769 population-based surveys and studies in 19 244 children aged 2 years–19 years (not reporting disaggregated data for school age). These investigators found that, from 1980 to 2013, in developed countries, the prevalence of overweight and obesity for 2-year-old to 19-year-old children (as a group) increased from 16.9% to 23.8% in boys and 16.2% to 22.6% in girls. In the same period, in developing countries, the prevalence of overweight and obesity increased from 8.1% to 12.9% in boys and 8.4% to 13.4% in girls. All studies show that globally, the peak prevalence of obesity is shifting to younger ages. While the prevalence remains higher in developed countries, the great majority of overweight and obese girls and boys (in absolute numbers) are from LIMCs, 79 thus representing a double burden of poor nutrition for the most populous countries in the world.
The NCD RisC 2020 study 80 showed that the difference between the highest mean BMI (eg, Pacific Island countries, the United States, Chile, South Africa) and lowest mean BMI (eg, India, Bangladesh, Ethiopia, and Chad) was 9 kg/m 2 –10 kg/m 2 in girls. Thus, the mean BMI difference, between these countries, was greater than 2 standard deviations in BMI for a 15-year-old girl. Trends by age varied significantly, and they worsened with age in many countries. In some countries (eg, Mexico, South Africa, New Zealand), 5-year-old children with healthy BMI progressively gained more in BMI than in height through the school-age years. Over time, some countries showed too little height gain, and/or too much weight gain for height (eg, Sub-Saharan Africa, New Zealand, the United States, Malaysia, some Pacific Island nations, and Mexico), with some differences by sex.
In summary, though the landscape has changed significantly in the last few decades, undernutrition (wasting/thinness/low BMI) and poor linear growth (low height for age/stunting), as well as overnutrition (elevated BMI with or without low height), remain major nutritional challenges globally. Today, still, despite the increase in overweight and obesity, more school-age children worldwide are moderately or severely underweight than overweight or obese. That said, in most countries, the prevalence increases in overweight and obesity are greater than the declines in prevalence of underweight. So, if current trends continue globally, the prevalence of obesity in school age will be higher than that of moderate and severe underweight before 2025. 80
The considerable global differences in these markers of nutritional adequacy reflect the geographic and socio-economic gaps that also persist globally. While genetics and other factors play a role, a difference of 20 cm in height and 9 kg/m 2 –10 kg/m 2 in BMI between extremes in populations is a partial reflection of the persistence of undernutrition and the large global nutritional and environmental gaps. Lastly, a rapid closing of those gaps may signal a “too rapid” transition from a mostly underweight population to a mostly overweight and obese population, as has occurred in parts of Asia and Latin America, accelerating and increasing the burden of nutrition-related conditions, particularly for LMIC populations.
While trajectories vary regionally, in many countries, based on height and BMI, nutritional status appears to be adequate at 5 years (which may reflect efforts over the last decades in improving early childhood health and nutrition) but deteriorates as children move through the school years. This heightens the relative neglect in attention to school-age nutritional focus, particularly for the 5–10 year-old population.
The global rise in obesity related to socio-economic and other environmental changes, including changes in nutrition, contributes to increases and exacerbations of type 2 diabetes, cardiovascular disease, and other noncommunicable diseases, exacerbating the double burden of disease and of cost to society. Prevention, starting prenatally, remains the most cost-effective and realistic approach. 84 So far, however, no clear or strong regional or national success stories have been demonstrated in the last decades. 82
Micronutrient deficiencies
Micronutrient deficiencies continue to be considered a major contributor to the global burden of disease. Despite this, a recent global report confirms a persistent and wide gap in data and information around micronutrient intake and nutrient status for all ages. 85 Individual deficiencies rarely occur in isolation. As for other indicators of nutrition and health, some school-age micronutrient data is available for some nutrients, and some are available from studies in adolescents and young adults. Still, data in 5-year-old to 15-year-old children is the least available across the board.
Based on the high prevalence of their deficiencies, WHO considers iron, vitamin A, vitamin D, zinc, iodine, and folate the most critical micronutrients globally. It is estimated that 25% of school-age children (around 305 million children) have anemia and that 50% of it is primarily associated with iron deficiency. 86 A 2004 report estimated the prevalence of vitamin A deficiency in school-age children in South Asia to be 23.4% or 83 million children, 9 million of whom had xerophthalmia. 87 In low-income countries, vitamin A deficiency prevalence has been estimated at 20% among early adolescent (10–14-year-old) girls and 18% among late adolescent (15–19-year-old) girls. 83 Worldwide, inadequate zinc intake is estimated at around 17%, with little data disaggregated for school children, 88 90% of which is in Africa and Asia. 89 The prevalence of inadequate iodine intake in 6-year-old to 12-year-old school-age children has been estimated at around 30% (241 million children), ranging from 13% in the Americas to 39% in Africa. 90 Limited data on folate deficiency in females 12 years–49 years (reproductive age) indicate a prevalence of more than 20% in lower-income and less than 5% in higher-income countries. There are no good global estimates of folate deficiency for school-age children. 88 , 91
In one report, vitamin D deficiency in 6-year-old to 12-year-old children ranged from 16% in North America, to 28% in Mexico, to 88% in China. 92 For calcium, as opposed to most other nutrients where adequacy can be measured using biomarkers, there is no universally accepted definition for deficiency. So dietary intake is used as the best proxy for adequacy. In addition, recommended intakes vary significantly by regional or expert groups. For school-age children, EFSA has stated a PRI of 800 mg/day for 4-year-olds to 10-year-olds and 1150 mg/day for 11-year-olds to 17 year-olds. The Institute of Medicine in the United States has stated a recommended dietary allowance of 1000 mg/day for 4-year-olds to 8-year-olds and 1300 mg for 9-year-olds to 13-year-olds. 55 While good estimates are lacking, average calcium intake in the United States for children 1 year to 14 years has been estimated at between 856 mg/day and 993 mg/day, depending on methodology, suggesting that many children fall below recommendations. There are no good global estimations, but from the little data available, it is evident that the great majority of children in developing countries fall far below any current recommendations. 93 Micronutrient deficiencies further compound the total burden of poor nutrition, as they coexist with wasting and obesity.
Studies and systematic reviews of micronutrient supplementation and fortification that include school-age children clearly show that micronutrient status can be improved. The demonstration of clinical effects, including growth and morbidity, varies significantly. The best documented is iron supplementation and fortification, which has been shown to improve iron status and reduce anemia in school-age children 5 years–12 years old. 94 A positive effect of iron supplementation on cognitive development has been shown, and interestingly, effectiveness appears greater for children older than 7 years than for younger ages. 95 Other effects of micronutrient supplementation, including growth and morbidity, are less clear. 81 , 96
Early attention to the significant effect of nutrition until 2 years of age and the assertions, even until recently, that stunting and cognitive delays were irreversible 97 , 98 may have contributed to the lower attention to middle childhood and adolescence as opportunities for recovery, particularly as related to stunting and cognitive deficits. Evidence today suggests this is not the case.
Catch-up growth through the school-age years is possible with the right interventions. Historical reports and observational studies of immigrant populations and adopted children document that in situations where environmental and nutritional conditions change positively, meaningful linear catch-up is possible. 99 Longitudinal observational data from the COHORT multicounty study and longitudinal data from rural Gambia have shown that significant catch-up in height can be achieved between 2 years of age and the end of middle childhood (10 y of age), and between middle childhood and adulthood, even in the absence of any nutrition or health interventions. 2 Catch-up growth is also possible in chronic conditions, including celiac disease and inflammatory bowel disease, with the right medical and nutritional interventions. 100 , 101
Although results are not always consistent, some longitudinal studies that include school-age populations (6 y–11 y old) show linear catch-up is possible with multiple micronutrient supplementation. 102 , 103 A recent systematic review and meta-analysis of the effectiveness of several nutrition-based interventions after 2 years of age (where more than half of the studies included children older than 5 years of age) showed including supplementation of protein, vitamin A, and/or multiple micronutrients, and particularly zinc supplementation, can improve linear growth, especially in children that have experienced early stunting. However, supplementation of other micronutrients, including iodine, iron, calcium, or food-based interventions, did not significantly affect growth, even if resolving anemia or other deficiencies. 96
Although populations and methodologies vary, some studies have not found a correlation between linear growth recovery and cognitive measures in short-term studies over 6 months, 104 while others have. Data from a longitudinal observational cohort in several LMICs found that children who had stunting by 1 year of age with linear growth catch-up by age 8 years had significantly better cognitive outcomes than those who remained stunted. 105 Height catch-up in these children was positively associated with improvements in mathematics achievement, reading comprehension, and receptive vocabulary. Children who remained stunted performed less well, and children who were never stunted remained ahead of the other groups. A subsequent study of the same cohort 74 analyzed catch-up growth between the ages of 8 years and 15 years and showed that more than one third of those stunted at age 8 years caught up to their peers by age 15 years, and also improved their cognitive scores compared with those who did not catch up in height. Notably, linear growth faltering was also accompanied by a decrease in cognitive outcomes in those children who became stunted between 8 years and 15 years. Thus, associations between linear growth and cognitive development vary from country to country and do not always persist from middle childhood through adolescence. 74 , 106 The extent of linear catch-up effect in various studies will vary obviously due to the timing of the initial insult, the timing of the intervention, the duration of the intervention, and other environmental conditions beyond nutrition. Given the obvious genetic, epigenetic, and environmental carryover between young mothers and their offspring, it seems likely also that reversing the cycle of undernutrition will probably require cross-generational catch-up. 107
Inadequate bone mass and mineral accretion in school-age children can have long-term consequences. While no good markers (except assessment of calcium intake and vitamin D) are available, adequate intakes remain important for reducing long-term risks. During the school-age years, a higher milk intake is associated with higher BMC, BMD, and reduced fracture risk in adulthood. Consuming less than one serving of milk a day in childhood was associated with a 2-fold increase in fracture risk as adults. 108 Establishing healthy dietary behaviors with a well-balanced diet that includes adequate calcium and vitamin D, particularly with inclusion of dairy products and regular physical activity, can bring about long-term bone health.
Despite the limited knowledge we have, the nutritional objectives for school-age children appear quite clear: providing energy and protein adequacy (including avoiding excesses), decreasing deficiencies of iron, iodine, vitamin A, vitamin D, calcium, zinc, and folate, and avoiding excesses of simple sugars and sodium. Long-term studies are still lacking, and there appears to be no “magic bullet” for improving dietary intakes and avoiding excesses. However, there is increasing evidence to support school dietary and physical activity–based interventions in schoolchildren to prevent deficiencies and address overweight and obesity. 109–111 The school setting has excellent potential for providing a significant part of daily intake to improve diet quality tailored to the local environment and educate children in nutrition and diet. The potential remains to be tapped.
This can only be accomplished with adequate individual, community, and population education, as well as policies that support these endeavours at multiple levels and by multiple stakeholders—a discussion that is beyond the scope of this review.
Very recently, the last 4 years to 5 years have brought about an increasing level of attention and calls for action to address the health and nutrition of middle childhood and adolescence. In 2017, Bundy et al published a comprehensive volume as part of the World Bank’s Disease Control Priorities series, with support from the Bill and Melinda Gates Foundation, highlighting child and adolescent health, with a focus on ages 5 years–19 years, as “neglected potential” that needs to be realized. 1 They noted an “asymmetry between the public investment in formal education versus health during the age range of 5 years–19 years, and a lack of recognition that the developmental returns from education are themselves dependent on concurrent good health and diet.” This “historical neglect of investments… [beyond the first 1000 d], including the next 7000 days of middle childhood and adolescence… is also reflected in investment in research into the older age-groups.” 1
Around this time, collaborative efforts in population-based studies are finally presenting a more comprehensive and clearer global picture of the nutritional status of children above 5 years of age. 79 , 80 Several research groups have reported on the significant potential that nutrition and health interventions have on improving outcomes during school age, thus constituting a true (and possibly last) major window of opportunity for supporting adequate nutrition, overcoming deficits from earlier life, shaping future dietary behaviors, and improving long-term health and well-being. 2–5
Even more recently, UNICEF’s Nutrition Strategy for 2020–2030 Framework called for “strategic shifts” in upholding children’s right to nutrition and ending child malnutrition in all its forms (as part of the global Sustainable Development Goals). The Strategy includes a comprehensive life cycle approach to nutrition programming, and maternal and child nutrition during the first 1000 days as core to UNICEF programs, and also explicitly states that “nutrition during middle childhood and adolescence is both a right and a window of opportunity for growth, development and learning, particularly for girls, and for breaking the intergenerational cycle of malnutrition.” The 2 first measurable Results areas for the Strategy are 1. Early Childhood Nutrition and 2. Nutrition in Middle Childhood and Adolescence. 112 UNICEF’s Programmatic Guidance for Nutrition in Middle Childhood and Adolescence includes specific priorities of nutritious foods, healthy food environments in schools and beyond, micronutrient supplementation and deworming, nutrition education in school curricula, and healthy dietary practices for school-age children and adolescents. 113
While not neglecting early-life nutrition, a life-cycle approach to nutrition requires increased attention and a re-prioritization of middle childhood and early adolescence. The school-age years provide unique opportunities that will need to be embraced, even more so now, given the added challenges placed on the world by the recent COVID pandemic and climate change.
Nutrition during the formative years remains the foundation for long-term health and productivity of the individuals who make up society. Of these formative years, the first 5, with good reason, have received great attention over the last few decades. Decreasing infant mortality, including the vicious cycle of undernutrition and disease, and a better understanding of health and disease’s developmental origins, have improved our focus and understanding of the critical first few years of life. This, however, was coupled with the poorly documented notion that somatic and cognitive harm or delay in the first 2 years of life were irreversible, and hindered in part the attention given to the rest of childhood, particularly middle childhood and early adolescence. Middle childhood and early adolescence remain the most underrepresented of all life stages in health and nutrition research and clinical, nutritional, and epidemiologic data.
After the first 1000 days, the school-age years represent the most dynamic period of change in somatic and cognitive development before an individual reaches maturity, with multiple changes and inflection points in growth and development trajectories. Figure 4 summarizes key milestones in somatic and brain growth and development and shows how “eventful” this life-cycle period truly is. Deficits in growth, bone health, cognitive development, and alterations in body composition during this period have a life-long impact. It is possible and critical that we intervene during school age (a) to maintain an adequate course of somatic and cognitive development and a bridge to adult life, (b) to correct deficits of undernutrition and “catch-up” to the normal course of growth and development, and (c) to modulate or mitigate inadequacies of overnutrition and avoid longer-term consequences. Middle childhood and adolescence are thus a last major opportunity for investment, to affect growth, nutrition, and ultimate health and cognitive outcomes.

The figure depicts key events in somatic and brain growth and development trajectories occurring in middle childhood and early adolescence. The timing is meant to show sequence, and the ages are best approximations. Divergence relates to differences between sexes. See text for related references. BMC: bone mineral content.
Childhood education, the basis for societal development, is not possible without adequate nutrition. In addition, child education and school systems themselves provide significant tangible opportunities for influencing dietary intake as well as for educating future generations on diet and nutrition. Therefore, it is imperative to improve our understanding of the opportunities presenting themselves during this period of life, and to develop policies and strategies to improve the current level of response to those opportunities. Only very recently has this understanding led to a revisiting of priorities in combating poor nutrition and its long-term consequences. The emphasis on intervention during the school-age years needs to be nurtured and reinforced.
The authors would like to thank Dr Francois-Pierre Martin, Dr Laurence Donato-Capel, and Dr Marie-Claire Fichot for reviewing and providing valuable suggestions regarding the manuscript.
Author contributions . All authors participated in the planning, review, and final approval of the manuscript. The content is solely and entirely the work of the authors.
Funding . The collection of material for this manuscript was partially supported by the Société des Produits Nestlé.
Declaration of interest . J.M.S. is a consultant for Société des Produits Nestlé, and Scaled Microbiomics. A.P. is a board member of the Nestlé Nutrition Institute.
Bundy DAP , Silva ND , Horton AP , et al. Child and adolescent health and development: realizing neglected potential. In: Bundy DAP , Silva ND , Horton S , Jamison DT , Patton GC , eds. Child and Adolescent Health and Development . 3rd ed. Washington, DC : The International Bank for Reconstruction and Development/the World Bank ; 2017: 1–23.
Google Scholar
Google Preview
Prentice AM , Ward KA , Goldberg GR , et al. Critical windows for nutritional interventions against stunting . Am J Clin Nutr. 2013 ; 97 : 911 – 918 .
Best C , Neufingerl N , van Geel L , et al. The nutritional status of school-aged children: why should we care? Food Nutr Bull. 2010 ; 31 : 400 – 417 .
Akseer N , Al-Gashm S , Mehta S , et al. Global and regional trends in the nutritional status of young people: a critical and neglected age group [published correction appears in Ann N Y Acad Sci . 2017;1396(1):236] . Ann NY Acad Sci. 2017 ; 1393 : 3 – 20 .
Georgiadis A , Penny ME. Child undernutrition: opportunities beyond the first 1000 days . Lancet Public Health. 2017 ; 2 : e399 .
Bundy DAP , de Silva N , Horton S , et al. Annex 1A. Supplemental material. In: Bundy DAP , Silva ND , Horton S , Jamison DT , Patton GC , eds. Child and Adolescent Health and Development . 3rd ed. Washington, DC : The International Bank for Reconstruction and Development/the World Bank ; 2017 :1. Available at: http://www.dcp-3.org/chapter/2754/annexes . Accessed May 11, 2022.
WHO . UNICEF, World Bank, and the Demographic and Health Surveys (DHS)/USAID database. 2021 . Available at: https://dhsprogram.com/data/ . Accessed May 11, 2022.
Galloway R. Global nutrition outcomes at ages 5 to 19. In: Bundy DAP , Silva ND , Horton S , Jamison DT , Patton GC , eds. Child and Adolescent Health and Development . 3rd ed. Washington, DC : The International Bank for Reconstruction and Development/the World Bank ; 2017 : 37 – 45 .
Sawyer SM , Azzopardi PS , Wickremarathne D , et al. The age of adolescence . Lancet Child Adolesc Health. 2018 ; 2 : 223 – 228 .
Alderman H , Behrman JR , Glewwe P , et al. Evidence of impact of interventions on growth and development during early and middle childhood. In: Bundy DAP , Silva ND , Horton S , Jamison DT , Patton GC , eds. Child and Adolescent Health and Development . 3rd ed. Washington, DC : The International Bank for Reconstruction and Development/the World Bank ; 2017 : 79 – 98 .
United Nations Children’s Fund (UNICEF) . Convention on the Rights of the Child. 1990 . Available at: https://www.unicef.org/child-rights-convention/convention-text . Accessed May 11, 2022.
Patton GC , Sawyer SM , Santelli JS , et al. Our future: a Lancet commission on adolescent health and wellbeing . Lancet. 2016 ; 387 : 2423 – 2478 .
McDonagh JE ; European Training Effective Care and Health Faculty . The age of adolescence…and young adulthood . Lancet Child Adolesc Health. 2018 ; 2 : e6 .
Cousminer DL , Berry DJ , Timpson NJ , et al. ; The ReproGen Consortium . Genome-wide association and longitudinal analyses reveal genetic loci linking pubertal height growth, pubertal timing and childhood adiposity . Hum Mol Genet . 2013 ; 22 : 2735 – 2747 .
DelGiudice M. Middle childhood: an evolutionary–developmental synthesis. In: Halfon N , Forrest CB , Lerner RM , Faustman EM , eds. Handbook of Life Course Health Development . Cham (CH ): Springer ; 2017 : 95 – 107 .
Reinehr T , Roth CL. Is there a causal relationship between obesity and puberty? Lancet Child Adolesc Health . 2019 ; 3 : 44 – 54 .
Song Y , Ma J , Wang HJ , et al. Trends of age at menarche and association with body mass index in Chinese school-aged girls, 1985–2010 . J Pediatr. 2014 ; 165 : 1172 – 1177.e1 .
Goswami B , Roy AS , Dalui R , et al. Impact of pubertal growth on physical fitness . Am J Sports Med. 2014 ; 2 : 34 – 39 .
USA Centers for Disease Control and Prevention (CDC): National Center for Health Statistics. CDC Growth Charts . Available at: https://www.cdc.gov/growthcharts/cdc_charts.htm . Accessed May 11, 2022.
Cole TJ. Children grow and horses race: is the adiposity rebound a critical period for later obesity? BMC Pediatr. 2004 ; 4 : 6 .
Veldhuis JD , Roemmich JN , Richmond EJ , et al. Endocrine control of body composition in infancy, childhood, and puberty . Endocr Rev. 2005 ; 26 : 114 – 146 .
Webber CE , Barr RD. Age- and gender-dependent values of skeletal muscle mass in healthy children and adolescents . J Cachexia Sarcopenia Muscle. 2012 ; 3 : 25 – 29 .
McCarthy HD , Samani-Radia D , Jebb SA , et al. Skeletal muscle mass reference curves for children and adolescents . Pediatr Obes. 2014 ; 9 : 249 – 259 .
Tanner JM , Davies PS. Clinical longitudinal standards for height and height velocity for North American children . J Pediatr. 1985 ; 107 : 317 – 329 .
Nijjar JK , Stafford D. Undernutrition and growth in the developing world . Curr Opin Endocrinol Diabetes Obes. 2019 ; 26 : 32 – 38 .
Owino V , Ahmed T , Freemark M , et al. Environmental enteric dysfunction and growth failure/stunting in global child health . Pediatrics . 2016 ; 138 : e20160641 .
Millward DJ. Nutrition, infection and stunting: the roles of deficiencies of individual nutrients and foods, and of inflammation, as determinants of reduced linear growth of children . Nutr Res Rev. 2017 ; 30 : 50 – 72 .
Prendergast AJ , Humphrey JH. The stunting syndrome in developing countries . Paediatr Int Child Health. 2014 ; 34 : 250 – 265 .
Baxter-Jones AD , Faulkner RA , Forwood MR , et al. Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass . J Bone Miner Res. 2011 ; 26 : 1729 – 1739 .
Maggioli C , Stagi S. Bone modeling, remodeling, and skeletal health in children and adolescents: mineral accrual, assessment and treatment . Ann Pediatr Endocrinol Metab. 2017 ; 22 : 1 – 5 .
Golden NH , Abrams SA ; Committee on Nutrition . Optimizing bone health in children and adolescents . Pediatrics . 2014 ; 134 : e1229 – e1243 .
Ralston SH , de Crombrugghe B. Genetic regulation of bone mass and susceptibility to osteoporosis . Genes Dev. 2006 ; 20 : 2492 – 2506 .
Weaver CM , Gordon CM , Janz KF , et al. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations [published correction appears in Osteoporos Int. 2016;27(4):1387] . Osteoporos Int. 2016 ; 27 : 1281 – 1386 .
Stiles J , Jernigan TL. The basics of brain development . Neuropsychol Rev. 2010 ; 20 : 327 – 348 .
Konrad K , Firk C , Uhlhaas PJ. Brain development during adolescence: neuroscientific insights into this developmental period . Dtsch Arztebl Int. 2013 ; 110 : 425 – 431 .
Mills KL , Goddings AL , Herting MM , et al. Structural brain development between childhood and adulthood: convergence across four longitudinal samples . Neuroimage. 2016 ; 141 : 273 – 281 .
Lenroot RK , Giedd JN. Brain development in children and adolescents: insights from anatomical magnetic resonance imaging . Neurosci Biobehav Rev. 2006 ; 30 : 718 – 729 .
Peterson MR , Cherukuri V , Paulson JN , et al. Normal childhood brain growth and a universal sex and anthropomorphic relationship to cerebrospinal fluid . J Neurosurg Pediatr. 2021 ; 28 : 458 – 468 .
De Bellis MD , Keshavan MS , Beers SR , et al. Sex differences in brain maturation during childhood and adolescence . Cereb Cortex. 2001 ; 11 : 552 – 557 .
Johnson SB , Blum RW , Giedd JN. Adolescent maturity and the brain: the promise and pitfalls of neuroscience research in adolescent health policy . J Adolesc Health. 2009 ; 45 : 216 – 221 .
Immordino-Yang MH , Darling-Hammond L , Krone C. The Brain Basis for Integrated Social, Emotional, and Academic Development. How emotions and social relationships drive learning . Washington, DC: The Aspen Institute National Commission on Social, Emotional, and Academic Development. 2018 . Available at: https://www.aspeninstitute.org/publications . Accessed May 11, 2022.
Dumontheil I. Development of abstract thinking during childhood and adolescence: the role of rostrolateral prefrontal cortex . Dev Cogn Neurosci. 2014 ; 10 : 57 – 76 .
Flege JE , Munro MJ , MacKay IR. Factors affecting strength of perceived foreign accent in a second language . J Acoust Soc Am . 1995 ; 97 : 3125 – 3134 .
Giedd JN , Blumenthal J , Jeffries NO , et al. Brain development during childhood and adolescence: a longitudinal MRI study . Nat Neurosci. 1999 ; 2 : 861 – 863 .
Diamond A. Executive functions . Handb Clin Neurol. 2020 ; 173 : 225 – 240 .
Anderson P. Assessment and development of executive function (EF) during childhood . Child Neuropsychol. 2002 ; 8 : 71 – 82 .
Spear LP. Adolescent neurodevelopment . J Adolesc Health. 2013 ; 52 : S7 – S13 .
Mills KL , Goddings AL , Clasen LS , et al. The developmental mismatch in structural brain maturation during adolescence . Dev Neurosci. 2014 ; 36 : 147 – 160 .
Kelley JC , Crabtree N , Zemel BS. Bone density in the obese child: clinical considerations and diagnostic challenges . Calcif Tissue Int. 2017 ; 100 : 514 – 527 .
Das JK , Salam RA , Thornburg KL , et al. Nutrition in adolescents: physiology, metabolism, and nutritional needs . Ann N Y Acad Sci. 2017 ; 1393 : 21 – 33 .
Trumbo P , Schlicker S , Yates AA , et al. ; Food and Nutrition Board of the Institute of Medicine, The National Academies . Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids [published correction appears in J Am Diet Assoc . 2003;103(5):563] . J Am Diet Assoc . 2002 ; 102 : 1621 – 1630 .
Chugani HT. Positron emission tomography scanning: applications in newborns . Clin Perinatol. 1993 ; 20 : 395 – 409 .
Grande Covián F. El metabolismo energético del cerebro en la infancia [Energy metabolism of the brain in children (author’s transl)] . An Esp Pediatr . 1979 ; 12 : 235 – 244 .
Kalhan SC , Kiliç I. Carbohydrate as nutrient in the infant and child: range of acceptable intake . Eur J Clin Nutr. 1999 ; 53 ( suppl 1 ): S94 – S100 .
European Food Safety Authority (EFSA) . Overview on Dietary Reference Values for the EU population as derived by the EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Summary of Dietary Reference Values – version 4. September 2017 . Available at: https://www.efsa.europa.eu/en/topics/topic/dietary-reference-values. Accessed May 11, 2022.
Branca F , Vatueña S. Calcium, physical activity and bone health–building bones for a stronger future . Public Health Nutr. 2001 ; 4 : 117 – 123 .
Heaney RP , Abrams S , Dawson-Hughes B , et al. Peak bone mass . Osteoporos Int. 2000 ; 11 : 985 – 1009 .
Sarafrazi N , Wambogo EA , Shepherd JA. Osteoporosis or low bone mass in older adults: United States, 2017–2018 . NCHS Data Brief . 2021 ;( 405 ): 1 – 8 .
Fragility Fractures - Epidemiology . Nyon, Switzerland: International Osteoporosis Foundation; 2021 . Available at: https://www.osteoporosis.foundation/health-professionals/fragility-fractures/epidemiology . Accessed May 11, 2022.
Prentice A , Schoenmakers I , Laskey MA , et al. Nutrition and bone growth and development . Proc Nutr Soc. 2006 ; 65 : 348 – 360 .
Georgieff MK , Ramel SE , Cusick SE. Nutritional influences on brain development . Acta Paediatr. 2018 ; 107 : 1310 – 1321 .
GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019 . Lancet 2020 ; 396 : 1223 – 1249 .
Camaschella C. Iron deficiency . Blood 2019 ; 133 : 30 – 39 .
Pivina L , Semenova Y , Doşa MD , et al. Iron deficiency, cognitive functions, and neurobehavioral disorders in children . J Mol Neurosci. 2019 ; 68 : 1 – 10 .
Lozoff B. Iron deficiency and child development . Food Nutr Bull. 2007 ; 28 : S560 – S571 .
Larson LM , Phiri KS , Pasricha SR. Iron and cognitive development: what is the evidence? Ann Nutr Metab. 2017 ; 71 ( suppl 3 ): 25 – 38 .
Briend A , Khara T , Dolan C. Wasting and stunting—similarities and differences: policy and programmatic implications . Food Nutr Bull. 2015 ; 36 : S15 – S23 .
Schoenbuchner SM , Dolan C , Mwangome M , et al. The relationship between wasting and stunting: a retrospective cohort analysis of longitudinal data in Gambian children from 1976 to 2016 . Am J Clin Nutr . 2019 ; 110 : 498 – 507 .
Fernald LCG , Prado E , Kariger P , et al. A Toolkit for Measuring Early Childhood Development in Low and Middle-Income Countries. 2017 International Bank for Reconstruction and Development, The World Bank, Washington DC. License: CC BY 3.0 IGO. Available at: https://openknowledge.worldbank.org/handle/10986/29000 . Accessed May 11, 2022.
Crookston BT , Penny ME , Alder SC , et al. Children who recover from early stunting and children who are not stunted demonstrate similar levels of cognition . J Nutr. 2010 ; 140 : 1996 – 2001 .
Sudfeld CR , McCoy DC , Danaei G , et al. Linear growth and child development in low- and middle-income countries: a meta-analysis . Pediatrics . 2015 ; 135 : e1266 – e1275 .
Walker SP , Chang SM , Powell CA , et al. Early childhood stunting is associated with poor psychological functioning in late adolescence and effects are reduced by psychosocial stimulation . J Nutr . 2007 ; 137 : 2464 – 2469 .
Sánchez A. The structural relationship between early nutrition, cognitive skills and non-cognitive skills in four developing countries . Econ Hum Biol. 2017 ; 27 : 33 – 54 .
Fink G , Rockers PC. Childhood growth, schooling, and cognitive development: further evidence from the Young Lives study . Am J Clin Nutr . 2014 ; 100 : 182 – 188 .
Caleyachetty R , Thomas GN , Kengne AP , et al. The double burden of malnutrition among adolescents: analysis of data from the Global School-Based Student Health and Health Behavior in School-Aged Children surveys in 57 low- and middle-income countries . Am J Clin Nutr. 2018 ; 108 : 414 – 424 .
Schott W , Aurino E , Penny ME , et al. The double burden of malnutrition among youth: trajectories and inequalities in four emerging economies . Econ Hum Biol. 2019 ; 34 : 80 – 91 .
Andersen CT , Stein AD , Reynolds SA , et al. Stunting in infancy is associated with decreased risk of high body mass index for age at 8 and 12 years of age . J Nutr . 2016 ; 146 : 2296 – 2303 .
World Health Organization. Noncommunicable Disease Surveillance, Monitoring and Reporting. Global School-based Student Health Survey . Available at: https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/global-school-based-student-health-survey. Accessed May 11, 2022.
NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in body–mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults . Lancet . 2017 ; 390 : 2627 – 2642 .
NCD Risk Factor Collaboration (NCD-RisC) . Height and body–mass index trajectories of school-aged children and adolescents from 1985 to 2019 in 200 countries and territories: a pooled analysis of 2181 population-based studies with 65 million participants . Lancet . 2020 ; 396 : 1511 – 1524 .
Best C , Neufingerl N , Del Rosso JM , et al. Can multi-micronutrient food fortification improve the micronutrient status, growth, health, and cognition of schoolchildren? A systematic review . Nutr Rev. 2011 ; 69 : 186 – 204 .
Ng M , Fleming T , Robinson M , et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013 [published correction appears in Lancet . 2014;384(9945):746] . Lancet . 2014 ; 384 : 766 – 781 .
Christian P , Smith ER. Adolescent undernutrition: global burden, physiology, and nutritional risks . Ann Nutr Metab. 2018 ; 72 : 316 – 328 .
Darnton-Hill I , Nishida C , James WP. A life course approach to diet, nutrition and the prevention of chronic diseases . Public Health Nutr. 2004 ; 7 : 101 – 121 .
McLean E , Cogswell M , Egli I , et al. Global Nutrition Report . Chapter 3. Development Initiatives Poverty Research Ltd 2018. 2018 . https://globalnutritionreport.org/reports/global-nutrition-report-2018/. Accessed May 11, 2022.
McLean E , Cogswell M , Egli I , et al. Worldwide prevalence of anaemia, WHO Vitamin and Mineral Nutrition Information System, 1993–2005 . Public Health Nutr. 2009 ; 12 : 444 – 454 .
Singh V , West KP Jr . Vitamin A deficiency and xerophthalmia among school-aged children in Southeastern Asia . Eur J Clin Nutr. 2004 ; 58 : 1342 – 1349 .
Bailey RL , West KP Jr , Black RE. The epidemiology of global micronutrient deficiencies . Ann Nutr Metab. 2015 ; 66 : 22 – 33 .
Kumssa DB , Joy EJ , Ander EL , et al. Dietary calcium and zinc deficiency risks are decreasing but remain prevalent . Sci Rep. 2015 ; 5 : 10974 .
Andersson M , Takkouche B , Egli I , et al. Current global iodine status and progress over the last decade towards the elimination of iodine deficiency . Bull World Health Organ. 2005 ; 83 : 518 – 525 .
Rogers LM , Cordero AM , Pfeiffer CM , et al. Global folate status in women of reproductive age: a systematic review with emphasis on methodological issues . Ann NY Acad Sci. 2018 ; 1431 : 35 – 57 .
Palacios C , Gonzalez L. Is vitamin D deficiency a major global public health problem? J Steroid Biochem Mol Biol. 2014 ; 144 ( Pt A ): 138 – 145 .
Pettifor JM. Calcium and vitamin D metabolism in children in developing countries . Ann Nutr Metab. 2014 ; 64 ( suppl 2 ): 15 – 22 .
De-Regil LM , Jefferds ME , Sylvetsky AC , et al. Intermittent iron supplementation for improving nutrition and development in children under 12 years of age . Cochrane Database Syst Rev 2011 ; 2011 : CD009085 .
Sachdev H , Gera T , Nestel P. Effect of iron supplementation on mental and motor development in children: systematic review of randomised controlled trials . Public Health Nutr. 2005 ; 8 : 117 – 132 .
Roberts JL , Stein AD. The impact of nutritional interventions beyond the first 2 years of life on linear growth: a systematic review and meta-analysis . Adv Nutr. 2017 ; 8 : 323 – 336 .
Martorell R , Khan LK , Schroeder DG. Reversibility of stunting: epidemiological findings in children from developing countries . Eur J Clin Nutr. 1994 ; 48 ( suppl 1 ): S45 – S57 .
Victora CG , Adair L , Fall C , et al. Maternal and child undernutrition: consequences for adult health and human capital [published correction appears in Lancet . 2008;371(9609):302] . Lancet . 2008 ; 371 : 340 – 357 .
Watkins KL , Bundy DAP , Jamison DT , et al. Evidence of impact of interventions on health and development during middle childhood and school age. In: Bundy DAP , Silva ND , Horton S , Jamison DT , Patton GC , eds. Child and Adolescent Health and Development . 3rd ed. Washington, DC : The International Bank for Reconstruction and Development/the World Bank ; 2017 : 99 – 105 .
Gasparetto M , Guariso G. Crohn’s disease and growth deficiency in children and adolescents . World J Gastroenterol. 2014 ; 20 : 13219 – 13233 .
Boersma B , Houwen RH , Blum WF , et al. Catch-up growth and endocrine changes in childhood celiac disease. Endocrine changes during catch-up growth . Horm Res. 2002 ; 58 ( suppl 1 ): 57 – 65 .
Abrams SA , Mushi A , Hilmers DC , et al. A multinutrient-fortified beverage enhances the nutritional status of children in Botswana . J Nutr . 2003 ; 133 : 1834 – 1840 .
Ash DM , Tatala SR , Frongillo EA Jr , et al. Randomized efficacy trial of a micronutrient-fortified beverage in primary school children in Tanzania . Am J Clin Nutr . 2003 ; 77 : 891 – 898 .
Sokolovic N , Selvam S , Srinivasan K , et al. Catch-up growth does not associate with cognitive development in Indian school-age children . Eur J Clin Nutr. 2014 ; 68 : 14 – 18 .
Crookston BT , Schott W , Cueto S , et al. Postinfancy growth, schooling, and cognitive achievement: young lives . Am J Clin Nutr. 2013 ; 98 : 1555 – 1563 .
Georgiadis A , Benny L , Duc LT , et al. Growth recovery and faltering through early adolescence in low- and middle-income countries: determinants and implications for cognitive development . Soc Sci Med. 2017 ; 179 : 81 – 90 .
Golden MH. Is complete catch-up possible for stunted malnourished children? Eur J Clin Nutr . 1994 ; 48 ( suppl 1 ): S58 – S70; discussion S71 .
Kalkwarf HJ , Khoury JC , Lanphear BP. Milk intake during childhood and adolescence, adult bone density, and osteoporotic fractures in US women . Am J Clin Nutr . 2003 ; 77 : 257 – 265 .
Jacob CM , Hardy-Johnson PL , Inskip HM , et al. A systematic review and meta-analysis of school-based interventions with health education to reduce body mass index in adolescents aged 10 to 19 years . Int J Behav Nutr Phys Act. 2021 ; 18 : 1 .
Singhal J , Herd C , Adab P , et al. Effectiveness of school-based interventions to prevent obesity among children aged 4 to 12 years old in middle-income countries: a systematic review and meta-analysis . Obes Rev. 2021 ; 22 : e13105 .
Kyere P , Veerman JL , Lee P , et al. Effectiveness of school-based nutrition interventions in sub-Saharan Africa: a systematic review . Public Health Nutr. 2020 ; 23 : 2626 – 2636 .
United Nations Children’s Fund (UNICEF) . Nutrition, for Every Child: UNICEF Nutrition Strategy 2020–2030 . New York : UNICEF . 2020 . Available at: https://www.unicef.org/media/92031/file/UNICEF%20Nutrition%20Strategy%202020-2030.pdf . Accessed May 11, 2022.
United Nations Children’s Fund (UNICEF) . Programming Guidance: Nutrition in Middle Childhood and Adolescence . New York, NY : UNICEF . 2021 . Available at: https://www.unicef.org/media/106406/file . Accessed May 11, 2022.
Tapert SF , Schweinsburg AD. The human adolescent brain and alcohol use disorders . Recent Dev Alcohol. 2005 ; 17 : 177 – 197 .
Lee FS , Heimer H , Giedd JN , et al. Mental health. Adolescent mental health—opportunity and obligation . Science. 2014 ; 346 : 547 – 549 .
- malnutrition
- science of nutrition
- middle childhood
- school-age child
- growth and development
| Month: | Total Views: |
|---|---|
| November 2022 | 375 |
| December 2022 | 167 |
| January 2023 | 189 |
| February 2023 | 244 |
| March 2023 | 326 |
| April 2023 | 342 |
| May 2023 | 350 |
| June 2023 | 570 |
| July 2023 | 541 |
| August 2023 | 493 |
| September 2023 | 482 |
| October 2023 | 676 |
| November 2023 | 661 |
| December 2023 | 501 |
| January 2024 | 506 |
| February 2024 | 560 |
| March 2024 | 789 |
| April 2024 | 798 |
| May 2024 | 742 |
| June 2024 | 564 |
| July 2024 | 807 |
| August 2024 | 494 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1753-4887
- Print ISSN 0029-6643
- Copyright © 2024 International Life Sciences Institute
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Login to your account
If you don't remember your password, you can reset it by entering your email address and clicking the Reset Password button. You will then receive an email that contains a secure link for resetting your password
If the address matches a valid account an email will be sent to __email__ with instructions for resetting your password
| Property | Value |
|---|---|
| Status | |
| Version | |
| Ad File | |
| Disable Ads Flag | |
| Environment | |
| Moat Init | |
| Moat Ready | |
| Contextual Ready | |
| Contextual URL | |
| Contextual Initial Segments | |
| Contextual Used Segments | |
| AdUnit | |
| SubAdUnit | |
| Custom Targeting | |
| Ad Events | |
| Invalid Ad Sizes |

- Submit Member Login
Access provided by
From Reflection to Action…
Download started
- Add to Mendeley

Get full text access
Log in, subscribe or purchase for full access.
Article metrics
Related articles.
- Download Hi-res image
- Download .PPT
- Access for Developing Countries
- Articles & Issues
- Articles In Press
- Current Issue
- List of Issues
- Supplements
- For Authors
- Author Guidelines
- Submit Your Manuscript
- Statistical Methods
- Guidelines for Authors of Educational Material Reviews
- Permission to Reuse
- About Open Access
- Researcher Academy
- For Reviewers
- General Guidelines
- Methods Paper Guidelines
- Qualitative Guidelines
- Quantitative Guidelines
- Questionnaire Methods Guidelines
- Statistical Methods Guidelines
- Systematic Review Guidelines
- Perspective Guidelines
- GEM Reviewing Guidelines
- Journal Info
- About the Journal
- Disclosures
- Abstracting/Indexing
- Impact/Metrics
- Contact Information
- Editorial Staff and Board
- Info for Advertisers
- Member Access Instructions
- New Content Alerts
- Sponsored Supplements
- Statistical Reviewers
- Reviewer Appreciation
- New Resources
- New Resources for Nutrition Educators
- Submit New Resources for Review
- Guidelines for Writing Reviews of New Resources for Nutrition Educators
- Podcast/Webinars
- New Resources Podcasts
- Press Release & Other Podcasts
- Collections
- Society News
The content on this site is intended for healthcare professionals.
- Privacy Policy
- Terms and Conditions
- Accessibility
- Help & Contact

Society Member Access
SNEB Members, full access to the journal is a member benefit. Login via the SNEB Website to access all journal content and features.
- Institutional Access: Log in to ScienceDirect
- Existing Subscriber: Log in
- New Subscriber: Claim access with activation code. New subscribers select Claim to enter your activation code.
Academic & Personal
Corporate r&d professionals.
- Full online access to your subscription and archive of back issues
- Table of Contents alerts
- Access to all multimedia content, e.g. podcasts, videos, slides

ecoliteracy.org
A New Philosophy for Nutrition Education
It is time for a new philosophy of nutrition education that informs our children about their personal health and the future of our planet.

I have just returned from the last of a series of meetings with health educators to establish the first mandated health education standards for California's public school system.
This group was brought together as a result of a state law, enacted in 2005, mandating content standards in the curriculum area of health education. The task at hand was to create standards defining "what a student should know and be able to do" as result of a quality health education program. The group set a goal to develop a cutting-edge document that addresses the needs of schools in the twenty-first century. There was certain agreement among this group of health experts that nutrition was a critical content area to be included in health education standards. However, the group process of establishing performance indicators reinforced my belief that the content area of "nutrition" needs some careful thought and redefinition.
Current California State Education Code specifies that nutrition education content in the health curriculum should be designed to help students learn the following:
- Nutritional knowledge, including but not limited to, the benefits of healthy eating, essential nutrients, nutritional deficiencies, principles of healthy weight management, the use and misuse of dietary supplements, and safe food preparation, handling, and storage.
- Nutrition-related skills, including, but not limited to, planning a healthy meal, understanding and using food labels, and critically evaluating nutrition information, misinformation, and commercial food advertising.
- How to assess their own personal eating habits, set goals for improvement, and achieve those goals by using the Food Guide Pyramid, Dietary Guidelines for Americans, Nutrition Fact Labels, and the Physical Activity Pyramid.
I believe it is time to articulate a new philosophy of nutrition education, one that reflects the urgency and critical need to inform our children about the impact of their food choices on their personal health, the health of our society, and the future of our planet. An argument in favor of a new era for nutrition education is also supported by a diverse international group of scholars and experts in food and nutrition working on a project entitled "New Nutrition Science." This group unanimously agreed that now is the time to add social and environmental dimensions to the definition and practice of nutrition science, while preserving all that is basic and vital in the biological dimension of the classic nutritional sciences.
Nutrition as a biological science was developed by Justus von Liebig at the University of Giessen, Germany in the mid-nineteenth century. In 2001, a series of international meetings began to re-explore the philosophy of nutrition. These scholarly gatherings led to the adoption in 2005 of the Giessen Declaration. It recommends a redefinition of nutrition that moves beyond nineteenth-century priorities such as industrial expansion to the priorities and principles of the twenty-first century, including conservation and preservation.
The Giessen Declaration supports the work of many in embracing a new and more holistic view of the interdependent, complex, processes involved in human dietary patterns. Such a view of nutrition takes an integrative systems approach to connecting individual understanding, motivation, and skills with ecological factors such as culture and physical environment, as compounded by additional impacts from related public policies that shape food systems and supplies.
The Giessen Declaration (1) includes the following principles:
Nutrition science needs to incorporate a comprehensive understanding of food systems. These shape and are shaped by biological, social, and environmental relationships and interactions. How food is grown, processed, distributed, sold, prepared, cooked, and consumed is crucial to its quality and nature, and to its effect on well-being and health, society, and the environment.
In the twentieth century, food production was transformed by heavy farm machinery and industrial chemistry, and now perhaps also will be by biotechnology. Food processing, including refrigeration, has enabled the supply of a wide range of foods across seasons and continents. Food manufacturing, retailing, and distribution are now increasingly concentrated in fewer hands. Traditional cuisines are being replaced by new eating patterns framed by new technologies, ways of living, and economic structures.
Nutrition science can and should engage with the development of technologies and with their impact on food systems. These profoundly affect the relationship between food and the health of people, populations, and the planet, and will continue to do so. These are additional reasons why it is time to reformulate nutrition science to include social and environmental as well as biological dimensions....
The overall principles that should guide nutrition science are ethical in nature. Its principles should also be guided by the philosophies of co-responsibility and sustainability, by the life-course and human rights approaches, and by understanding of evolution, history, and ecology.
During the development of this project, Mark Wahlqvist, the president of the International Union of Nutritional Sciences, stated that "the new nutrition science has a context of a new world for all of the sciences, which themselves are on the threshold of momentous change….Science will be required to acknowledge its social responsibility and its duty to work and act in the best interests of all people and of the planet as a whole."
As a member of the California Health Education Standards Advisory Panel, I submitted the following definition of nutrition science, as stated in the Giessen Declaration, and requested that it be incorporated into the list of definitions that will be included in the Health Education Standards document:
Nutrition science is defined as the study of food systems, foods and drinks and their nutrients, and other constituents; and of their interactions within and between all relevant biological, social, and environmental systems.
The purpose of nutrition science is to contribute to a world in which present and future generations fulfill their human potential, live in the best of health, and develop, sustain, and enjoy an increasingly diverse human, living, and physical environment.
Nutrition science should be the basis for food and nutrition policies. These should be designed to identify, create, conserve, and protect rational, sustainable, and equitable communal, national, and global food systems in order to sustain the health, well-being, and integrity of humankind, and of the living and physical worlds.
The Center for Ecoliteracy’s Rethinking School Lunch program and curricula are leading the way in actualizing the new nutrition science vision and lofty ideals. It is time to join together, with a sense of urgency, to shape the legislation, policies, and actions that will infuse this message into the mainstream educational system.
- The Giessen Declaration. Public Health Nutrition . September 2005; 8(6A): 783-786.
SUPPORT EDUCATION FOR THE SUSTAINABILITY OF PEOPLE AND THE PLANET
More like this.


Feeding Our KIds the Right Foods… and Inspiring Them to Eat!
Schools around the country are taking bold steps to add whole, local, and healthy foods to their school meals.

The Importance of Nutrition Education and Why It Is Key for Educational success
Most people already connect nutrition and health, but what about health and educational goals?

By Feeding Young People Well, We Nourish Our Own Future
Author and farmer Michael Ableman has found the solution to revolutionizing school food.
Ecoliteracy in your Inbox!
Get ideas, inspiration, and knowledge to help you teach and model sustainable practices in your school community.
We never sell or share your private information.
Nutrition & Students Academic Performance Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
It is argued that educators and policy makers must consider nutrition as a critical ingredient in the development of educational interventions principally designed to enhance the participation and academic performance of students across the world (Galal & Hulett 2003, p. 11). Recently, more than ever, academics, educators and health professionals are in agreement that nutrition plays a significant role on a range of variables of school performance, including but not limited to “…enrolment, attendance, grade repetition, behaviour cognition, psychosocial well-being, and achievement levels” (Grantham-McGregor & Olney 2006, p. 105). Nutritional status, specifically overall diet quality is a variable of substantial importance for students as it influences intelligence and scholastic achievement (Ivanovic et al 2008, p. 19), as well as cognition and behavior (Florence, Asbridge & Veugellers 2008, p. 209).
Extant literature demonstrates that although parents, educators, and health professionals continue to tout the interdependence between what students eat and their educational achievement, evidence for this association is not always obvious, not mentioning that recurrent biases on both sides of the argument often override data when this topic is brought to the attention of the relevant stakeholders (Taras 2005, p. 199). More importantly, very few studies have cared to analyze this issue from the cost perspective despite the fact that cost concerns are known to impinge on the availability, affordability, and accessibility of healthy food for students not only in Australia but also globally (Wong et al 2011, p. 11). The present study seeks to fill these two gaps in the literature.
According to one particular study, undernourished school-going children “…have been shown to have decreased attendance, attention, and academic performance, as well as experience more health problems compared to well-nourished children” (Florence et al 2008, p. 210). More resoundingly, preventive supplementation studies suggest a causal relationship between iron-anemia in early childhood on the one hand and poor cognition, late school enrolment, classroom behavioral challenges, poor school achievement, and increased drop-out rates from school on the other hand (Grantham-McGregor & Olney 2006, p. 105).
But while these studies may post conclusive results on school-going children (Pollitt, Gersovitz & Gargiulo 1978, p 478), the same cannot be validated on university student populations in the absence of exhaustive studies (Unwin 2004, p. 144). More importantly, mature students are in charge of their nutrition uptake depending on their level of awareness (Goldberg 1998, p. 99), financial endowment (Wong et al 2011, p. 11), and behavioral orientations (Murray et al 2007, p. 590). It is indeed true that even if food security is regarded to be high in Australia (Wong et al 2011 p. 8), access to a healthy diet may often be limited for this group of the population due to the variables already mentioned, leading to poor dietary intake. This view is reinforced by Cameron and Madden (2011), who suggest that “…the relatively high cost of certain foods compatible with healthy eating and the lower price of others has been suggested as one of many barriers to achieving nutritional goals.” It is therefore imperative to evaluate how students’ compatibility with healthy eating is impacted by the cost of food and, ultimately, how this association affects their academic performance.
The study will utilize Heider’s (1958) psychological theory of attribution to evaluate how nutritional status affects students’ performance. Available literature demonstrates that “…attribution theory is concerned with how individuals interpret events and how this relates to their thinking and behavior” (University of Twente 2010, para. 2). In the context of the research question, it will be assumed that students attribute their performance to some innate variables such as their character, attitude, or personality (internal attribution), or to the inference by some external variables such as dietary status and cost of food (external attribution). This model is justifiable as it will assist the investigator to unearth existing evidence linking students’ dietary intake, cost implications, and their ability to learn through attribution.
Cameron, SJ & Madden, DM 2011, ‘The cost of a basket of food compatible with healthy eating guidelines are higher than a comparable basket of standard food’, Journal of Human Nutrition & Dietetics , vol. 24 no. 4, pp. 380-381.
Florence, MD, Asbridge, M & Veugellers, PJ 2008, ‘Diet quality and academic performanc, Journal of School Health , vol. 78 no. 4, pp. 209-215.
Galal, O & Hulett, J 2003, ‘The relationship between nutrition and children’s educational performance: A focus on the United Arab Emirates’, Nutrition Bulletin , vol. 28 no. 1, pp. 11-20.
Goldberg, JP 1998, ‘The recommended dietary allowances: Can they inform the development of standards of academic achievements?’, Applied Measurement in Education, vol. 11 no. 1, pp. 97-105.
Grantham-McGregor, S & Olney, DK 2006, ‘School feeding, cognition, and school achievement’, Current Medical Literature: Paediatrics , vol. 19 vol. 4, pp. 105-111.
Ivanovic, D, Rodriguez, MP, Perez, H, Alvear, J, Diaz, N, Leyton, B…Ivanovic, R 2008, ‘Twelve-year follow-up study of the impact of nutritional status at the onset of elementary school on later eeducational situation of Chilean school-age children’, European Journal of Clinical Nutrition , vol. 62 no. 1, pp. 18-31.
Murray, NG, Low, BJ, Holus, C, Cross, AW & Davis, SM 2007, ‘Coordinated school health programs and academic achievement: A systematic review of the literature’, Journal of School Health , vol. 77 no. 9, pp. 589-600.
Pollitt, E, Gersovitz, N & Gargiulo, M 1978, ‘Educational benefits of the United States school feeding program: A critical review of the literature’, American Journal of Public Health , vol. 68 no. 5, pp. 477-481.
Taras, H 2005, ‘Nutrition and student performance at school’, Journal of School Health , vol. 75 no. 6, pp. 199-213.
University of Twente 2010, Attribution theory , Web.
Unwin, J 2004, ‘Celebrating the achievement of young people in nutrition’, Nutrition Bulletin , 29 no 2, pp. 143-145.
Wong, KC, Coveney, J, Ward, P, Muller, R, Carter, P, verity, F & Tsourtos, G 2011, ‘Availability, affordability and quality of a healthy food basket in Adelaide, South Australia’, Nutrition & Dietetics , vol. 68 no. 1, pp. 8-14.
- Community Teaching Work Plan
- Students' Performance and Nutrition: Is There a Relation?
- Suicide and Fundamental Attribution Theory
- US Nutrition Policy: Pros and Cons of the Policy
- Childhood Obesity and Type 2 Diabetes
- Acculturation and Eating Disorders in Western Countries
- Issues of Methodology Nutrition, Implications of Iodine
- Nutritional Assessment for Cancer Patients
- Dietary Intake: 3-Day and 24-Hour Models
- Nutrition: the Anthropometric Measurements
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, May 4). Nutrition & Students Academic Performance. https://ivypanda.com/essays/nutrition-amp-students-academic-performance/
"Nutrition & Students Academic Performance." IvyPanda , 4 May 2022, ivypanda.com/essays/nutrition-amp-students-academic-performance/.
IvyPanda . (2022) 'Nutrition & Students Academic Performance'. 4 May.
IvyPanda . 2022. "Nutrition & Students Academic Performance." May 4, 2022. https://ivypanda.com/essays/nutrition-amp-students-academic-performance/.
1. IvyPanda . "Nutrition & Students Academic Performance." May 4, 2022. https://ivypanda.com/essays/nutrition-amp-students-academic-performance/.
Bibliography
IvyPanda . "Nutrition & Students Academic Performance." May 4, 2022. https://ivypanda.com/essays/nutrition-amp-students-academic-performance/.

Essay on Food and Nutrition
Students are often asked to write an essay on Food and Nutrition in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Food and Nutrition
Importance of food and nutrition.
Food and nutrition are essential for life. They provide the energy we need to grow, work, play, think, and learn.
The Role of Food
Food is much more than just fuel. It contains vital nutrients like vitamins, minerals, proteins, carbohydrates, and fats, which our body needs to function correctly.
Nutrition and Health
Nutrition is about how food affects our health. A balanced diet helps to maintain a healthy weight, reduces the risk of diseases like diabetes, heart disease, and cancer, and promotes overall well-being.
In conclusion, food and nutrition are vital for our health and well-being. It’s important to eat a balanced diet to stay healthy.
250 Words Essay on Food and Nutrition
Introduction to food and nutrition, the role of nutrients.
Nutrients are classified into macronutrients and micronutrients. Macronutrients, including carbohydrates, proteins, and fats, are needed in large amounts and provide the energy necessary for daily activities. Micronutrients, such as vitamins and minerals, are required in smaller quantities but are crucial for various physiological functions like immune response and bone health.
Food Choices and Health
Our food choices significantly impact our health. A balanced diet comprising all nutrients in appropriate proportions promotes good health and helps prevent diseases. Conversely, unhealthy eating habits can lead to conditions like obesity, heart disease, and diabetes. The concept of ‘food as medicine’ is gaining traction, emphasizing the therapeutic potential of natural foods.
Nutrition Science and Society
The science of nutrition has societal implications. It can guide public health policies, influence food production practices, and shape societal attitudes towards food and health. Nutrition education can empower individuals to make informed food choices, thereby promoting public health at large.
In conclusion, food and nutrition are intertwined aspects of health. Understanding their interplay can help us make informed dietary choices, promoting overall wellbeing and preventing disease. The study of nutrition is not merely a biological or chemical analysis but a comprehensive exploration of how our food choices shape our health and society.
500 Words Essay on Food and Nutrition
Food and nutrition are fundamental aspects of our lives that influence our health, wellness, and longevity. They are interconnected fields of study that examine the relationship between diet, health, and disease. Nutrition focuses on how dietary intake impacts health, while food science explores the physical, biological, and chemical makeup of food.
The Importance of Balanced Nutrition
Food quality and nutritional value.
The quality of the food we consume significantly impacts its nutritional value. Highly processed foods, while convenient and often tasty, frequently contain high levels of sugars, salts, and unhealthy fats. These can lead to health issues like obesity, heart disease, and diabetes. On the other hand, whole foods like fruits, vegetables, lean proteins, and whole grains are nutrient-dense and promote good health.
Role of Diet in Disease Prevention
There’s a growing body of evidence linking diet and disease. High intake of saturated and trans fats, sugars, and sodium is associated with an increased risk of chronic diseases. Conversely, diets rich in fiber, lean proteins, and unsaturated fats can help prevent conditions like heart disease, diabetes, and certain cancers. Furthermore, certain nutrients have specific protective effects. For instance, antioxidants found in fruits and vegetables can neutralize harmful free radicals, reducing the risk of chronic diseases.
Nutrition and Sustainability
Conclusion: the future of food and nutrition.
In the future, personalized nutrition, based on individual genetic makeup, lifestyle, and gut microbiome, may play a significant role in health management. Additionally, innovative food technologies like cellular agriculture could provide sustainable and ethical food sources. As we continue to unravel the complexities of food and nutrition, it’s clear that they will remain central to our health and well-being. This underscores the importance of education in these fields, encouraging informed dietary choices and fostering a healthier society.
That’s it! I hope the essay helped you.
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
- Skip to main content
- Skip to secondary menu
- Skip to primary sidebar
- Skip to footer
A Plus Topper
Improve your Grades
Nutrition Essay | Essay on Nutrition for Students and Children in English
February 12, 2024 by Prasanna
Nutrition Essay: The section of science that deals with the interpretation of nutrients and food in the animal system to sustain a healthy life and to keep health issues at check is known as ‘nutrition.’ The topic of nutrition is vulnerably proportional to the economic stability of a society or a country at a broader aspect.
A necessity that keeps life running at the cost of money, to which a noticeable chunk of the society is deprived but remains unattended to, is also ‘nutrition.’
You can also find more Essay Writing articles on events, persons, sports, technology and many more.
Long and Short Essays on Nutrition for Students and Kids in English
We are providing students with essay samples on a long essay of 500 words and a short essay of 150 words on the topic nutrition for reference.
Long Essay on Nutrition 500 Words in English
Long Essay on Nutrition is usually given to classes 7, 8, 9, and 10.
As the name suggests, ‘nutrition’ includes in itself’ nutrients’ which can be broadly classified as carbohydrates, proteins, fats, vitamins, minerals, roughage, and water. A balanced amount of these nutrients in the right proportions constitute a healthy diet.
The words’ balanced’ and ‘right proportions’ mentioned previously are key to life when it comes to consuming nutrients. ‘Optimum Nutrition’ is defined as eating the right amount of nutrients in a proper schedule to achieve the best performance and longest possible lifetime in good health. The importance of nutrition can be visibly highlighted by the increasing number of nutrient deficiency diseases such as night blindness, scurvy, cretinism, anemia, and nutrient excess health-threatening conditions like obesity, metabolic syndrome, and other cardiovascular anomalies.
Undernutrition in underdeveloped and developing countries has been marked by malnutrition due to lack of even the basic staple nutrients causing diseases like marasmus and kwashiorkor. Animal nutrition on the molecular level comes from nitrogen, carbon, and hydrogen compounds. Nutrients are the building blocks of the food chain, which interlink to form food webs and influence world food production via biodiversity.
Similarly, plant nutrition is referred to as the chemicals that are necessary for plant growth and other physiological processes in plants like metabolism, transport, photosynthesis, etc. Nutrients essential for plants are obtained from the soil, air, sunlight, and as a whole from the earth; thus, the nutrients can be recycled and renewed, making it easily available for sustenance of life.
Fatigue, tiredness, and apathy are common among the working class as well as students. To feel refreshed, motivated as well as reenergized, all we require is the proper nutrition for our systems. Nutrition helps an individual attain optimal health throughout life as well as boost self-esteem.
Eating a balanced diet improves a person’s health and well-being and reduces risks of major causes of death. The other benefits of nutrition include a healthy heart, strength in teeth and bones, maintains good brain health, boosts immunity, bolsters the body to fight against diseases, keeps higher energy levels, and keeps the bodyweight at check. With such a minimum as maintaining our diet comes the strength of independence or self-dependence. The topic of nutrition has gained its importance by being studied and researched over for years. Nutrition is taught as a subject in various levels of education, and professions such as farmers, scientists, nutritionists, dietitians, health counselors, and doctors who form the pillar of our society are all based on nutrition fundamentals.
Progressive research works from various parts of the world on ‘nutrition’ has helped in aiding health conditions for the living, yet a big section of society is not reached out for proper food supplies. With the current progressive rate of scientific enhancement in the field of nutrition, resulting in increasing food production, we should be able to reach out to those who are dying due to the lack of something as basic as food, which should be available to everyone equally.
Short Essay on Nutrition 150 Words in English
Short Essay on Nutrition is usually given to classes 1, 2, 3, 4, 5, and 6.
‘Nutrition’ is one of the fundamentals of living that can be defined as the assimilation of food into living systems that help life function daily.
The classification of nutrition can vary from plants to animals, but they are interlinked by the food chains that form the ecosystem’s structural framework.
The components of nutrition include carbohydrates, proteins, fats, fibers, vitamins, minerals, water, and roughage when consumed in the right proportions, gives it the name of ‘balanced diet.’ Likewise, in plants, chemicals being obtained through absorption, transpiration, and photosynthesis are the nutrients that help in their internal processes.
The benefits of following a good nutritional diet plan ranges from good physical health to proper well-being and ensure a good immune system. Good nutrition with proper and regular exercise can assure a person a disease-free future. Even during ailment, proper nutrition can help cure a patient faster and safer. Hence adequate nutrition is a key to a healthy life and a necessity that should be looked after at any cost.
10 Lines on Nutrition in English
- Nutrition is a natural demand for every source of life on earth.
- Being deprived of nutrition is as severe as being deprived of any other fundamental rights.
- Lack of nutrition can give rise to lethal diseases.
- The knowledge of the classification of nutrients and their biological systems’ roles should be known to all.
- The benefits of proper nutrition ensure physical and mental well-being.
- Malnutrition has always been an issue adding to the rise in global hunger for years, as reported by the United Nations.
- As reported, 1.5 million children die annually due to the lack of proper nutrition.
- The Human Body’s primary requirement is nutrition. It would be impossible to sustain life without it.
- Studies on nutrition should be encouraged.
- Lack of nutrition gives rise to social disparity and discrimination.
FAQ’s on Nutrition Essay
Question 1. What are the benefits of proper nutrition?
Answer: Proper nutrition helps build the immune system of the body and maintain good physical and mental health.
Question 2. What is a balanced diet?
Answer: A balanced diet includes all types of the necessary nutrients in the right amount at proper intervals, helping maintain the various human and plant organ systems.
Question 3. What are the results due to a lack of nutrition?
Answer: The lack of proper nutrition can severely result in malnutrition, which is currently a cause of global hunger.
Question 4. What food should be consumed daily?
Answer: A diet that includes all of the fundamental nutrients and water in the right amount should be consumed daily with regular exercise.
- Picture Dictionary
- English Speech
- English Slogans
- English Letter Writing
- English Essay Writing
- English Textbook Answers
- Types of Certificates
- ICSE Solutions
- Selina ICSE Solutions
- ML Aggarwal Solutions
- HSSLive Plus One
- HSSLive Plus Two
- Kerala SSLC
- Distance Education
III. CONCLUSIONS AND RECOMMENDATIONS
Conclusions
131. The Meeting recognized that good nutrition is fundamental for children’s current and future health, as well as their development and learning. The benefits of developing healthy dietary and lifestyle patterns from an early age onwards can positively impact on people’s nutrition and health throughout their adult lives, and enhance the productivity of individuals and nations. Nutrition education is an important element in an overall strategy aimed at improving food security and preventing all forms of malnutrition. Schools (from pre-school to secondary) are ideal settings for promoting lifelong healthy eating habits and lifestyles.
132. Most countries in the region implement school health and nutrition programmes, including school feeding, deworming, vitamin and mineral supplementation, etc. Innovative, creative and effective school nutrition education programmes exist in some countries in the region. However, these are often small-scale and implemented as pilot projects, focus on children with special needs and prioritize the transfer of knowledge over the promotion of active learning and the creation of appropriate attitudes, life skills and behaviors. Generally, nutrition education is not systematically integrated into school curricula in the region.
Recommendations for country action
133. In order to build a comprehensive and sustainable school nutrition programme that addresses all forms of malnutrition, the Meeting recommended that countries:
- Consolidate and strengthen ongoing school based nutrition programmes, aiming at improved nutritional status and learning of school children and creating an appropriate learning environment through nutrition education, school gardening and school meals, nutritional assessment, clean water and sanitation, as well a physical activity education.
- Apply a multi-disciplinary and multi-stakeholder holistic approach to support effective school based nutrition programmes and policies at national and local levels.
- Promote the active involvement of parents, communities and local government in the development and implementation of school nutrition programmes.
- Advocate for the integration of nutrition education into the school curriculum for all age groups.
- Promote the integration of nutrition training into the course curriculum of teacher’s training institutes.
- Review existing teaching/learning materials on school nutrition education and promote the adaptation of available, or the development of new materials in line with local needs and conditions.
- Promote the establishment of school gardens as an integral part of school nutrition programmes.
- Explore opportunities for appropriate public private partnerships to support health and nutrition education and improvements in the school environment.
- Explore funding opportunities among bilateral, multi-lateral donors and NGOs.
- Encourage countries to work towards making all schools nutrition-friendly with adequate political commitment and funding.
- Ensure that nutrition education in schools always applies the tri-partite curriculum approach (i.e. link nutrition education in the classroom with learning in the school environment, home and community).
- Nutrition education should always employ a wide range of hands-on teaching/learning methods.
Recommendations for FAO action
134. Initiate the establishment of a coordinating mechanism for standardising data collection on school-age children (i.e. food consumption, dietary and eating patterns, anthropometry and physical activity) at the regional level.
135. Organise a follow-up satellite meeting on School based Nutrition at the forthcoming International Congress on Nutrition (Bangkok, 4-9 October 2009).
136. Disseminate the nutrition education materials developed by FAO.
137. Explore opportunities for translating FAO materials into additional languages.
138. Explore opportunities for providing technical assistance in the development and implementation of school nutrition projects in interested countries and identify funding support through FAO’s Technical Cooperation Programme or bilateral trust funds.
139. Promote sharing of information and materials on school based nutrition among ANFN members.
140. Facilitate provision of assistance to countries in the establishment of M & E system for monitoring progress on school based nutrition.
Agenda item 8: Adoption of report and closing
141. The draft report of the Meeting was reviewed by the participants and adopted.
142. In conclusion, Biplab K. Nandi thanked the participants and guests for their active participation and valuable inputs to the Meeting. He expressed optimism that the outputs of the Meeting specifically the action plans at the country level would bring forward school nutrition education for sustainable food and nutrition security.
Technical Meeting of the Asia-Pacific Network for Food and Nutrition on School Based Nutrition
17 – 20 July 2007, Bangkok, Thailand
LIST OF PARTICIPANTS
| Mirza Altaf Hossain Executive Director Bangladesh Applied Nutrition & Human Resource Development Board Ministry of Agriculture Sech Bhaban, 22, Manik Mia Avenue Sher-e-Bangla Nagar, Dhaka 1207 Telephone: (880-2) 9117862/8110798 Facsimile: (880-2) 8110798 Email: | |
| Sanjib Kumar Saha PRA Promoters' Society – Bangladesh House # 8/A/8, (3 Floor) Road # 14 (New) Dhanmondi, Dhaka Bangladesh Telephone: (880-2)-9128744 Mobile: 880-01711152344 Facsimile: (880-2)-8113446 Email: | |
| Chhavyroth So Vice Chief of the Technical Office School Health Department Ministry of Education, Youth and Sport No. 169 Norodom Blvd, Sangkat Beong Keng Kang I, Khan Chamka Morn Phnom Penh Telephone: (+855 23) 218408, Mobile: (+855 12) 694607 Facsimile: (+855 23) 218408 Email: | |
| Yoshiko Ogawa No. 5, Street No. 370 Boeung Keng Kang Phnom Penh Telephone: (+855 23) 726422 Facsimile: (+855 23) 221560 Email: | |
| Fengying Zhai Deputy Director National Institute of Nutrition and Food Safety Chinese Center for Disease Control and Prevention Secretary General Chinese Nutrition Society 29 Nan Wei Road Beijing 100050 Telephone: (8610) 83132503l; mobile: 13501099588 Facsimile: (8610)83132909 Email: | |
| Ma Jun Deputy Director Professor Institute of Child and Adolescent Health Peking University 38 Xueyuan Road Beijing 100083 Telephone: 86(10)-82801624 86-13641010885 Facsimile: 86(10)82801178 Email: | |
| Shashi P. Gupta Technical Adviser Food and Nutrition Board Ministry of Women and Child Development Government of India (Room No. 105, 2 floor) Jeevan Deep Building, Sansad Marg New Delhi 110001 Telephone: (91-11) (O) 23362519, (R) (91-11) 26863063 Facsimile: (91-11) 23362519 Email: | |
| P.K Mohanty Deputy Educational Adviser, Room No 326-C Wing Ministry of Human Resource Development Shastri Bhawan New Delhi 110001 Telephone: (91-11) 91-11-23383432 Email: | |
| Hardinsyah Professor and Dean Faculty of Human Ecology Bogor Agricultural University Jl. Kampur Gedung FEMA W1-W2 Kampus IPB Darmaga, Bogor 16680 Telephone: (62-251) 642 092 Facsimile: (62-251) 629 882 Email: | |
| Nata Irawan SH. MSi Director Socio Cultural Empowerment Directorate General Community and Regional Empowerment Department of Internal Affairs Telephone: 0816822412/021 - 7990419 Email: | |
| Bounthom Phengdy Head of Health and Nutrition Promotion Division Department of Hygiene and Prevention Ministry of Health Vientiane Telephone: (856) 21 416787; (856) 20 5618246 Facsimile: (856) 21 214010 Email: | |
| Sithath Outhaithany IE Team Leader Secretariat, National School Health Task Force Deputy Chief Primary Education Division Department of General Education Ministry of Education Telephone: (856) 250946, Mobile: (856-20) 5819799 Facsimile: (856) 250946 Email: | |
| Indira Sharma Professor Foods and Nutrition Head, Central Dept of Home Science Padma Kanya Multiple Campus, (TU) Bagbazar, Kathmandu Telephone: (977 1) 4225209 Facsimile: (977 1) 434907 Email: (R) | |
| Indra Bahadur Shrestha Programme Director Food for Education Project Ministry of Education and Sports Naxal Katmandu Telephone: (977 1) 4431895/4431853 Facsimile: (977 1) 4430650 Email: | |
| Maria Antonia G. Tuazon Director Regional Training Programme on Food and Nutrition Planning and Institute of Human Nutrition and Food College of Human Ecology University of the Philippines Los Banos U.P. Los Banos, College Laguna 4031 Telephone: (63-49) 5362364/5362918 Facsimile: (63-49)-5362445 Email: | |
| Magdalene Portia T. Cariaga Nutritionist-Dietitian II Department of Education DepEd Complex, Meralco Avenue Pasig City Manila Telephone: (+632) 632-13-61 ext. 2092 Facsimile: (+632) 633 7245 Email: | |
| Chandrani L. Piyasena Head Nutrition Department Medical Research Institute P.O. Box 527 Colombo 00800 Telephone: (94-11) 2695999 Facsimile: (94-11) 2691495 Email: | |
| M.P.H.Silva Deputy Director of Education (Nutrition) Provincial Department of Education Green Path Colombo – 07. Telephone: 00 94 11 2690478 Facsimile: 00 94 11 2693894 Email: | |
| Pattanee Winichagoon Associate Professor Deputy Director for Academic Affairs Institute of Nutrition, Mahidol University (INMU) Salaya, Nakhon Pathom, Thailand, 73170 Telephone: (+66-2) (DL) 889-2168, 8002380 ext. 313 Facsimile: (+66-2) 441-9344 Email: | |
| Nantaporn Viravathana Academic Adviser Office of Her Royal Highness Princess Maha Chakri Sirindhorn’s Projects, Chitralada Villa, Dusit Palace Bangkok 10303 Telephone: (+66-2) 282 6511, 281 3921 Facsimile: (+66-2) 281 3923 Email:
| |
| Assistant Professor Department of Biochemistry Phramongkutklao College of Medicine 315 Rajavithi Road Bangkok 10400 Telephone: (+66-2) 3547797, mobile (081) 8371500 Facsimile: (+66-2) 3547797 Email: | |
| Ladda Mo-suwan Associate Professor Department of Pediatrics Faculty of Medicine Prince of Songkla University Hat Yai, Songkhla 90110 Telephone: (+66-2) 7445-1273 Facsimile: (+66-2) 7421-2900 E-mail: | |
| Nguyen Cong Khan Director The National Institute of Nutrition 48 Tang Bat Ho Hanoi Telephone: (84-4) 9716058, Facsimile: (84-4) 9717885 Email: | |
| Kraisid Tontisirin Senior Adviser Institute of Nutrition Mahidol University at Salaya Putthamonthon Nakorn Prathom 73170 Telephone: (+662) 9380621/5134112/5115151 Mobile: (+6687) 717-0621 Facsimile: (+662) 9383604 Email: | |
| Andrew Colin Bell Short Term Professional Noncommunicable Diseases WHO Western Pacific Region U.N. Avenue, Manila, Philippines 1000 Manila Telephone: (632) 5289860 (direct), 5288001 (general) Facsimile: (632) 5260279 Email: | |
| Simon Baker Chief, HIV/AIDS Coordination and School Health Unit Principal Regional Office for Asia and the Pacific (PROAP) Mom Luang Pin Malakul Contennial Building 920 Sukhumvit Road, Klongtoey, Prakanong Bangkok 10110 Telephone: (622) 3910577 Facsimile: (622) 3910866 Email: | |
| Uraiporn Chittchang Asst. Professor Head of Community Nutrition Section Institute of Nutrition Mahidol University at Salaya Putthamonthon Nakorn Prathom 73170 Telephone: (+66-2) 8002380 ext.312/(DL) 8892168 Facsimile: (+66-2) 4419344 Email: | |
| Ellen Muehlhoff Senior Nutrition Officer Nutrition and Consumer Protection Division FAO Headquarters 00153 Rome Italy Telephone: Email: | |
| Peter Glasauer Nutrition and Consumer Protection Division FAO Headquarters 00153 Rome Italy Telephone: (+3906) 57053775 Email: | |
| Malcolm Hazelman Senior Extension, Education and Communication Officer FAO Regional Office for Asia and the Pacific Maliwan Mansion, 39 Phra Atit Road Bangkok 10200 Telephone: (+662) 6974145 Facsimile: (+662) 6974445 Email: | |
| Biplab K. Nandi Senior Food and Nutrition Officer FAO Regional Office for Asia and the Pacific Maliwan Mansion, 39 Phra Atit Road Bangkok 10200 Telephone: (+662) 6974143 Facsimile: (+66-2) 6974445 or 6974405 Email: | |
| Peter Sousa Hoejskov APO – Food Quality and Safety FAO Regional Office for Asia and the Pacific Maliwan Mansion, 39 Phra Atit Road Bangkok 10200 Telephone: (+662) 6974198 Facsimile: (+66-2) 6974445 Email: | |
| Natcha Thearapati Secretary FAO Regional Office for Asia and the Pacific Maliwan Mansion, 39 Phra Atit Road Bangkok 10200 Telephone: (+66-2) 6974265 Facsimile: (+66-2) 6974445 or 6974405 Email: |
Appendix II
OPENING ADDRESS By He Changchui Assistant Director-General and Regional Representative for Asia and the Pacific
delivered at the
Distinguished participants, Representatives from WHO and UNESCO FAO colleagues from Headquarters and the regional office, Ladies and Gentlemen
It is indeed a pleasure for me to address this important Technical Meeting of the Asia-Pacific Network for Food and Nutrition on School Based Nutrition. On behalf of FAO Director-General Jacques Diouf and on my own behalf, I welcome all of you to this meeting organized by the FAO Regional Office for Asia and the Pacific.
There have been major changes in the nutrition scenario in the Asia- Pacific region. Although the region is still facing problems related to undernutrition and food insecurity, significant proportions of the people of the region are confronted with the double burden of malnutrition and diet-related chronic diseases. Obesity, diabetes, coronary heart diseases, hypertension and certain forms of cancers have indeed been recognized as main causes of premature death and disability not only in industrialized countries but also in many developing countries that are becoming more and more prone to such life-style and diet-related health problems.
FAO recognizes the important contribution that schools can make in countries’ efforts to overcome food insecurity and such types of malnutrition problems. To support these efforts, FAO in collaboration with other international organizations develops and promotes innovative strategies and materials that assist countries to plan and implement school based nutrition education. The organization of the present consultation is indeed timely and relevant in this context.
Schools are potentially excellent settings for nutrition education. Children consume at least one or two meals daily on school grounds. The school environment can strongly influence children’s eating behaviours, whether through the examples provided by teachers and other adults, the food served in the cafeteria and classroom, or through exposure to peer habits. Effective nutrition education helps shape these environmental factors and assists students in developing the skills needed to select healthy diets. Given that eating habits have a profound impact on health in childhood and adulthood, schools provide a logical venue for ensuring that nutrition education reaches all school-age children, and even beyond, to their family members. It has been recognized that nutrition education plays an important role in an overall strategy for improving children’s eating habits. A well-designed curriculum can focus on developing skills in food selection and preparation rather than just imparting information about the relationship between diet and health.
There is potential for the school meals programme to assume a more active role in nutrition education. It may be a good idea if schools consider taking steps toward including educational cafeteria programmes as well as classroom work in school nutrition education.
Because eating habits developed during childhood have the potential to last a lifetime, it is important for children to learn about the benefits of good nutrition. Education to establish healthy eating habits in life can assure that individuals have the information and skills they need to protect and enhance their own health and the health of their families. One can think of establishing “Team Nutrition” to help schools implement the School Meals Initiative. The mission of “Team Nutrition” could be to improve the health and education of young people by creating innovative public and private partnerships that promote food choices for a healthful diet through media, schools, families, and the community. “Team Nutrition” can work simultaneously through two initiatives which include training and technical assistance to school food service personnel, and nutrition education for children.
Another concept which has tremendous potential towards nutrition promotion is establishing School Gardens. School Gardens are powerful tools for improving child nutrition and education. They have the potential to improve food security and human nutrition at the household level through replication in the home. FAO encourages schools to create moderate-sized learning gardens, producing a variety of fruits and vegetables using simple techniques so that teachers and parents can easily manage the garden and students can apply gardening techniques in their home. Improving the nutritional value of school meals by supplementing them with food rich in micronutrients, fresh from the School Garden is one of many benefits that School Gardens can offer.
The goal of nutrition education is to motivate people to eat a healthy diet. Children are an important audience for nutrition education because a healthy diet is essential for their normal growth and development, and because children are establishing food patterns that carry into adulthood. Good nutrition promotes not only better physical health and reduced susceptibility to disease, but has also been demonstrated to contribute to cognitive development and academic success. Left to their own devices, children will not automatically select healthy foods. Their innate preference for sweet foods makes them particularly vulnerable to the highly sugared cereals, soda, and candy that are marketed to them virtually from birth. In order to develop lifelong healthy eating patterns, children need to be introduced to a variety of nutritious foods in a positive manner.
Distinguished Participants
Ladies and Gentleman
In collaboration with WHO and Education International, FAO co-published a document entitled Health Nutrition: An Essential Element of a Health-Promoting School . Implemented in southeastern China, FAO worked with WHO and the Education Development Centre to assist six pilot schools in developing nutrition education and services. The experiences gained in this project are described in two journal articles, namely Nutrition as an entry point for health promotion schools: lessons from China and Creating health-promoting schools in China with a focus on nutrition . In fact, the pilot projects proved to be so successful that the local governments have decided to expand the Health-Promoting Schools project into 50 additional schools in 11 cities across Zhejiang Province. A comprehensive Planning Guide to assist curriculum developers to plan nutrition education and activities that incorporate local nutrition issues and needs is forthcoming soon. A companion training manual will help prepare professionals to facilitate the curriculum planning and implementation process. Keeping this spirit in view, I suggest the meeting considers the following key action points during your discussions: (1) Compulsory Nutrition Education in the School Curriculum; (2) Inclusion of Comprehensive Nutrition Education Topics highlighting the relationship between diet and health; (3) Coordination of Nutrition Education at all national fora; (4) Providing more Resources for Nutrition Education; (5) Strengthening School Meals Programme; and (6) Introducing School Garden Programme.
I am pleased to share with you that two recently concluded projects in Bangladesh and Lao PDR have demonstrated that School Gardening amalgamated with nutrition education can be powerful tools for promoting horticulture and nutrition.
I am also happy to see that there are as many as 26 participants from 11 countries (Bangladesh, Cambodia, China, India, Indonesia, Lao PDR, Nepal, Philippines, Sri Lanka, Thailand and Viet Nam). Besides there are colleagues from international organization like WHO and UNESCO. I am confident that a meeting like this will generate rich deliberations and I am looking forward to the outcomes of the meeting.
I now declare the Technical Meeting of Asia-Pacific Network for Food and Nutrition on School Based Nutrition ”open.
I thank you all and wish you a pleasant stay in Bangkok.
Appendix III
|
|
0830 hrs Registration
| 0900 - 0930 |
Biplab K. Nandi, Secretary, ANFN, and Senior Food and Nutrition Officer, FAO Regional Office for Asia and the Pacific (RAP), Bangkok |
|
| |
|
ADG/RR, FAO Regional Office for Asia and the Pacific | |
| Photo Session / Refreshment | |
| 1010 - 1040 |
Objectives, adoption of provisional agenda, timetable and organization of the Consultation |
| 1040 – 1100 |
Simon Baker, Chief, HIV/AIDS Coordination and School Health Unit, UNESCO Principal Regional Office for Asia and the Pacific (PROAP) |
| 1100 – 1130 |
Dr. Andrew Colin Bell, Technical Officer, Noncommunicable Diseases, WHO Western Pacific Region |
| 1130 - 1230 |
(4 groups; with country presentations) |
| 1230 - 1330 | Lunch hosted by ADG/RR, FAO RAP |
| 1330 - 1430 | (contd.) |
| 1430 – 1445 | , Group 1 |
| 1445 – 1500 | presentation on the theme, Group 2 |
| 1500 – 1515 | presentation on the theme, Group 3 |
| 1515 – 1530 | presentation on the theme, Group 4 |
| 1530 - 1600 | Coffee break |
| 1600 – 1700 |
|
| 1700 - 1715 |
|
| 1715 - 1745 | Meeting of the Drafting Committee |
| 0830 - 0900 |
Brainstorming (in groups) |
| 0900 - 0930 | |
| 0930 - 1000 |
Peter Glasauer, Nutrition Officer, FAO Headquarters |
| 1000 - 1030 | Coffee break |
| 1030 - 1100 |
Ellen Muehlhoff, Senior Nutrition Officer, FAO Headquarters |
| 1100 - 1130 |
Biplab K. Nandi, Senior Food And Nutrition Officer, FAORAP |
| 1130 - 1200 |
|
| 1200 - 1300 | Lunch |
|
|
| 1300 – 1325 | – Thailand |
| 1325 – 1350 | – Philippines |
| 1350 – 1415 |
|
| 1415 – 1440 | Bangladesh |
| 1440 – 1510 | Coffee break |
| 1510 – 1535 | – India |
| 1535 - 1600 | – Cambodia |
| 1600 – 1630 |
|
| 1630 – 1645 |
|
| 1645 - 1715 |
|
| 1715 – 1745 | Meeting of the Drafting Committee |
| 0830 – 1030 |
(as presented under agenda item 2; four working groups) |
|
| |
| 1030 -1230 |
|
| 1230 – 1330 | Lunch |
| 1330 - 1500 |
(four working groups; and country teams) |
| 1500 - 1530 | Coffee break |
| 1530 - 1700 |
(10+5 minutes per group outputs; +5 minutes per country action plan) |
| 1700 -1730 | Meeting of the Drafting Committee |
| 0830 – 1200 | to Institute of Nutrition, Mahidol University, Bangkok The Drafting Committee simultaneously prepares the of the Consultation |
| 1200 - 1300 | Lunch |
| 1300 – 1415 |
|
| 1415 – 1430 |
|
| 1430 - 1445 |
|
Appendix IV
Technical Meeting of the Asia-Pacific Network for Food and Nutrition
on School based Nutrition
Guide for group work on
Agenda Item 2 : Country Presentations on the nutrition situation of school age children and school based health and nutrition programmes (including nutrition education)
Group work (4 groups) with country presentations of group members and preparation of summary for subsequent presentation and discussion in plenary.
1. describe the current country situation in respect of the points dealt with in the questionnaire and the outline given below, referring to any relevant documentation
2. raise questions (e.g. is nutrition education effective ?)
3. identify important issues and needs (e.g. need for teacher education, parent attitudes)
Participants base their presentations on their completed questionnaires.
Session format : Four groups, each representing three (two) countries.
- Each country describes its situation, which is summarized on PP slides or on a poster. Questions and issues are identified and noted on separate PP slides/posters.
- The group Rapporteur makes a plenary presentation.
- The slides/posters are displayed for future reference
- Documents are added to the document exhibition.
Outline for country presentation:
A. (1) the nutritional and health status of school-age children and (2) factors that influence children’s food intake and nutritional practices
B. the response from the different sectors in terms of direct health and nutrition interventions (e.g. school feeding, de-worming, vitamin supplementation, health monitoring)
C. the response in terms of school based nutrition education , re-emphasising its importance in affecting behaviour and reaching future generations, and touching on the important parameters for effective NE (place in curriculum, time allocated, needs-based behaviour-oriented approach, whole-school policy, links to family and community, use of school gardens, staff development).
Outline for PowerPoint master slide / poster
Country: ……………………
A1. Summary of nutritional and health status of school-age children
A2. Factors influencing children’s food intake and nutritional practices
B. Inventory of existing direct health and nutrition interventions
C. Features of existing school based nutrition education programmes

Appendix IX
Agenda Item 5: Group work
Review of ongoing country school health and nutrition programmes (as presented under agenda item 2); four working groups
DISCUSSION TOPICS
Working from the needs and issues identified in the country presentations (Agenda item 2), groups review the ongoing health and nutrition programmes in their countries in various aspects, identifying strengths, priority needs, opportunities and challenges.
Working Group 1: Curriculum content: what should be learned?
Review ongoing school health and nutrition programmes in your countries from the point of view of curriculum content
Working from the situation and issues identified in the country presentations,
- outline the principles on which curriculum content for nutrition education should be decided (e.g. priority needs, general knowledge, local conditions?)
- suggest what kinds of learning objectives should be given priority (knowledge, attitudes, practical skills, behaviour, all four?)
- indicate what areas are well covered by existing programmes and which areas need further development.
Working Group 2: Curriculum implementation: how can NE be integrated?
Review on-going school health and nutrition programmes in your countries from the point of view of curriculum implementation
- describe existing processes for curriculum review at local or national level and attendant challenges
- suggest the most effective ways of establishing new curriculum in nutrition education (What sectors should be involved? What stakeholders should be consulted and how? What approval procedures are necessary? What kind of needs analysis is indicated?)
- suggest how new nutrition education topics can best be integrated into the existing curriculum (a cross-cutting issue across the curriculum, local/national action, formal vs informal options, stand-alone or integrated into other subjects) and what obstacles present themselves
- say if nutrition education should/could be incorporated into existing examination/certification structures.
Working Group 3: The tripartite approach: how can it be implemented?
Review on-going school health and nutrition programmes in your countries from the point of view of implementing the tripartite approach
Working from the situation and issues identified in the country presentations, indicate how far the tripartite approach is already implemented, how amenable the education system is to this strategy, what areas most need improvement and what strategies might be most effective. Take each element in turn:
- the whole-school approach: individual school health and nutrition policy and mission statement; staff development and awareness of their status as role-models; hygiene and sanitation measures in school grounds; establishment of school gardens and their use in nutrition education; integration of nutrition education with direct health and nutrition interventions such as school feeding, deworming, vitamin supplements; approaches to snacks and snack vendors
- involvement of the family – as a resource and support, as a source of information for children and for the school, as receivers of messages, as helpers with homework
- involvement of the community – as a resource and support, as a source of information and as an object of study.
Working Group 4: Methodology and materials:
Review on-going school health and nutrition programmes in your countries from the point of view of teaching methodology and teaching materials
- describe the methodological approach which is likely to be most effective in nutrition education
- identify essential and desirable elements in learning/teaching materials for nutrition education, including the role of learning materials in teacher development
- identify the strengths of present teaching staff and materials writers and suggest in what areas capacity needs to be developed
- identify appropriate institutional frameworks for such capacity-building (e.g. pre-service and in-service education, certification for teachers, organizations and conferences, writing workshops), including the establishment of regional networks for capacity building.

Appendix XIV
NAME: ________________________
COUNTRY: ________________________
Please write 2-3 paragraphs of the nutrition situation and ICN/WFS follow up activities in the context of MDGs of your country
(to be included into the proceedings/report)
TITLE: ________________________
Please write 3-4 paragraphs about the lesson learned and best practice on nutrition education in schools that you presented.
Nutrition Education for Children
Introduction.
Healthy eating is necessary for the development and good health of children between the ages of 3-15. The learning institutions are determined to promote and educate children on healthy eating (Marcano-Olivier et al., 2021). However, children between the ages 3-15 are still engaging in unhealthy nutrition practices (Weihrauch-Blüher et al., 2023). Thus, there is a need to develop an integrated program to address the nutrition needs of children that demonstrates high chances of effectiveness and efficiency in its delivery. The main aim of the paper carry out a literature review on nutrition education interventions for children in the ages 3-15 and identify the approaches to educate children in the ages 3-15 on nutrition. The topic is essential in the health promotion of the target population to guarantee their well-being in their adult life. Therefore, the paper is set to address nutrition education for children by developing an integrated educational program aimed at the promotion of healthy eating habits among children ages 3-15, by evaluating the program’s effectiveness in the enhancement of food choices and nutritional knowledge.
Summary of Articles
The article by Marcano-Olivier et al., (2021) identified the need to identify the adjustment in the children’s nutritional content after the implementation of the Dudes healthy eating initiative. The study notes that the effectiveness of healthy eating habits is always actualized in primary schools. The Dudes program is demonstrated as an intervention that is multicomponent with the capacity to be adopted at the national and regional levels within Ireland and England. The program is instrumental in the promotion of vegetable and fruit consumption through the application of rewards, repeated tasting, and role modeling (Marcano-Olivier et al., 2021). Role modeling is crucial in modifying consumption behavior, repeated tasting is linked with intensified expressed consumption of a food item and the rewards are linked to the desirability and affordability of the food items. The interventions considered by the programs are teacher-led in the classroom settings and others in the homes in the immediate dining rooms. Moreover, the study concludes that changes that are short-term based on dietary habits realized over 2 months can be significant and robust.
Pulimeno et al., (2020) identify schools as an appropriate setting that can promote the wellbeing and health of young people. The outcome of the study shows that student well-being promotion can significantly decrease unhealthy outcomes while at the same time enhancing children’s academic achievements (Pulimeno et al., 2020). It is acknowledged that about 80% of all heart disease cases, type 2 diabetes, and strokes can be avoided through health education. Pulimeno et al., (2020) conclude that primary schools should have health promotion integration into the ordinary learning and teaching practices to have improved health.
In another study by Adeoya, Akinwusi & Nagatomi, (2023) the authors acknowledge that the number of people who cannot afford to eat healthy foods has increased to about 3.1 billion with the majority being children in 2022. The food choices considered by children are established to be impacting their well-being, development, and nutritional health. The meals and school surroundings are required to complement dietary messages that are healthy to realize optimal effects (Adeoya, Akinwusi & Nagatomi, 2023). Besides, children below the age of 15 are noted to be having difficulty in understanding the link existing between the school mi-day meal choice and health. They are in most cases unable to establish the sources of minerals, vitamins, and proteins.
Approaches To Educate the Target Population about the Topic
The approaches to educating the target population include the typical experimental learning approaches to increase nutritional knowledge, vegetable consumption, fruit consumption, and decreased energy and food intake. The experimental approach involves interventions that are school-based including campaigns in social marketing, dietary improvement policies, environmental interventions, nutrition learning programs, nutrition-friendly initiatives, and curriculum evaluations and initiatives. The approaches will consider the culture of the target population through the development of feeding practices that are culturally responsive to recognize the children’s families’ cultural beliefs associated with feeding (Daniels, (2019). The feeding programs will have to take into consideration the customs, beliefs, and values that are accepted by the parents to attract support from the parents and guardians in ensuring the program realizes its objective. The lifestyle changes will be promoted through the use of a flexible schedule where the parents will have to adhere to the timing for snacks, dinner, and lunch. The mechanism will be crucial in reassuring parents that their children are consuming enough quantities and reinforcing the desired behaviors among the children (Dalal et al., (2022). The children will have to eat after about four to five hours.
Moreover, the health promotion strategies that will be involved include educational meetings, educational materials, visits that are educational outreach based, and tailored intervention for the marginalized groups of children in the ages 3-15. Most of the promotion strategies will be implemented in the school settings surroundings and a few will be implemented in the residential areas of the children (Wolfenden et al., 2020). The implementation strategies will substantially improve the program, and practices implemented by childcare services that encourage obesity prevention, physical activity, and healthy eating.
In summary, addressing nutrition education for children by developing an educational program aimed at the promotion of healthy eating habits among children the ages 3-15, by evaluating the program’s effectiveness in the enhancement of food choices and nutritional knowledge is essential in identifying a viable nutrition option that can address the health needs of children. The majority of the nutrition education interventions implemented are teacher-led in the classroom settings and others in the homes in the immediate dining rooms. The student’ well-being promotion can significantly decrease unhealthy outcomes while at the same time enhancing children’s academic achievements reducing the occurrence of about 80% of all heart disease cases, type 2 diabetes, and strokes. Children between the ages of 3 and 15 can be effectively educated on nutrition through an experimental approach that involves interventions that are school-based including campaigns in social marketing, dietary improvement policies, environmental interventions, nutrition learning programs, nutrition-friendly initiatives, and curriculum evaluations and initiatives.
Adeoya, A. A., Akinwusi, A. T., & Nagatomi, R. (2023). Effectiveness of nutrition education in enhancing knowledge and attitude of pupils on choice of school mid‐day meal in Ibadan, Nigeria. Food Science & Nutrition .
Dalal, M., Cazorla-Lancaster, Y., Chu, C. G., & Agarwal, N. (2022). Healthy From the Start—Lifestyle Interventions in Early Childhood. American Journal of Lifestyle Medicine , 16 (5), 562-569.
Daniels, L. A. (2019). Feeding practices and parenting: A pathway to child health and family happiness. Annals of Nutrition and Metabolism , 74 (Suppl. 2), 29-42.
Marcano-Olivier, M., Sallaway-Costello, J., McWilliams, L., Horne, P. J., Viktor, S., & Erjavec, M. (2021). Changes in the nutritional content of children’s lunches after the Food Dudes healthy eating programme. Journal of Nutritional Science , 10 , e40.
Pulimeno, M., Piscitelli, P., Colazzo, S., Colao, A., & Miani, A. (2020). School as ideal setting to promote health and wellbeing among young people. Health promotion perspectives , 10 (4), 316.
Weihrauch-Blüher, S., Huizinga, O., Joisten, C., Pflanz, J., Torbahn, G., Wiegand, S., … & Hauner, H. (2023). Changes in lifestyle and body weight in children and adolescents during the COVID-19 pandemic: A representative survey of parents in Germany. Obesity Facts , 16 (3), 301-312.
Wolfenden, L., Barnes, C., Jones, J., Finch, M., Wyse, R. J., Kingsland, M., … & Yoong, S. L. (2020). Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database of Systematic Reviews , (2).
Cite This Work
To export a reference to this article please select a referencing style below:
Related Essays
Effects of caffeine on sleep, services of primary health care centers, advanced levels of clinical inquiry and systematic reviews, exploring the intersection of technology and human experience, effects of nurse burnout, the role of planaria as a model organism in understanding drug effects and human health, popular essay topics.
- American Dream
- Artificial Intelligence
- Black Lives Matter
- Bullying Essay
- Career Goals Essay
- Causes of the Civil War
- Child Abusing
- Civil Rights Movement
- Community Service
- Cultural Identity
- Cyber Bullying
- Death Penalty
- Depression Essay
- Domestic Violence
- Freedom of Speech
- Global Warming
- Gun Control
- Human Trafficking
- I Believe Essay
- Immigration
- Importance of Education
- Israel and Palestine Conflict
- Leadership Essay
- Legalizing Marijuanas
- Mental Health
- National Honor Society
- Police Brutality
- Pollution Essay
- Racism Essay
- Romeo and Juliet
- Same Sex Marriages
- Social Media
- The Great Gatsby
- The Yellow Wallpaper
- Time Management
- To Kill a Mockingbird
- Violent Video Games
- What Makes You Unique
- Why I Want to Be a Nurse
- Send us an e-mail
- Open access
- Published: 27 February 2024
Effect of nutrition education intervention on nutrition knowledge, attitude, and diet quality among school-going adolescents: a quasi-experimental study
- Sagar Raut 1 ,
- Dirghayu KC 2 ,
- Devendra Raj Singh 3 ,
- Raja Ram Dhungana 4 ,
- Pranil Man Singh Pradhan 5 &
- Dev Ram Sunuwar 6 , 7
BMC Nutrition volume 10 , Article number: 35 ( 2024 ) Cite this article
5272 Accesses
1 Citations
10 Altmetric
Metrics details
Nutrition education is being used to encourage school adolescents to adopt healthy eating habits. To the best of our knowledge, very little study has been undertaken in Nepal to examine the effectiveness of nutrition education programs. This study aimed to assess the effect of nutrition education on nutritional knowledge, attitude, and diet quality among school-going adolescents in selected private schools in Nepal.
A quasi-experimental study was conducted among 226 students aged 12 − 19 years of two selected private schools in Banepa municipality of Nepal. Students ( n = 113) from the first school were assigned to intervention and the same number of students from the second school were enrolled in the study as the control. Over 12 weeks, students in the intervention group received one hour of nutrition education in the form of mini-lectures and interactive discussions, whilst students in the control group received no education. The student’s two-sample t-test was used to compare two groups and to assess the effectiveness of the nutrition education program.
Between the intervention and control group, the magnitude of difference in knowledge score was 1.80 (95% CI: 1.11 − 2.49), emotional eating was 0.98 (95% CI: 0.42 − 1.54), uncontrolled eating was 3.60 (95% CI: 2.10 − 5.09), and cognitive restraint of eating was 2.26 (95% CI: 1.51 − 3.01).
Conclusions
A tailored health education intervention was found to be effective in increase nutritional knowledge and attitude among school-going adolescents. Adopting nutrition education interventions as part of public health school intervention builds positive knowledge, attitudes, and healthy eating habits in school-going adolescents.
Peer Review reports
Introduction
Adolescence is a critical time in a human’s life for promoting healthy choices and lifestyle behaviors to prevent risk factors of chronic diseases [ 1 , 2 ]. Individuals aged between 10 and 19 years are considered adolescents [ 3 ]. The adolescent population constitutes 1.2 billion worldwide, making up 16% of the world’s population [ 4 ]. During adolescence, individuals are nutritionally vulnerable as their growth faces spurts of changes and if nutritional requirements are not met properly it might lead to malnutrition in later life [ 5 ]. To meet this increased demand, sufficient intake of both macro and micronutrients is crucial at this stage [ 6 ]. Nutritional knowledge plays an important role in influencing healthy food habits which ensures their nutrient needs during adolescence and later life [ 7 , 8 ]. The basis for creating attitudes toward foods, nutrition, and health, as well as human eating behaviors, is nutrition knowledge [ 9 ]. To encourage adolescents to adopt healthy lifestyle practices, it is necessary to create a suitable environment at school and home [ 10 ]. Multiple components such as social, economic, and environmental factors must be considered to tackle childhood malnutrition [ 11 ].
However, evidence suggested that low education levels contributed to false perception, which was found to be one of the precipitating factors for nutritional deficiencies among adolescents [ 12 ]. People are more prone to changes in their lifestyle during adolescence, which may later affect their lives [ 13 ]. Understanding the benefits of good nutrition, and the value of a diverse diet as healthy eating habits at an early age could determine dietary practices later in the future [ 14 ]. As the schools have the potential of involving adolescent students, they are often considered for implementing education programs [ 15 ]. Educational program enhance knowledge, attitude, and practice for acquiring healthy behaviors among adolescents in schools or communities [ 16 , 17 ].
Despite the efforts made by government and other agencies to promote healthy food choices in schools and public places, studies have shown that adolescents have poor knowledge, attitudes, and practices about malnutrition and dietary intake [ 8 , 18 ]. It is often reported that adolescent in developing countries like Nepal has either lacked adequate nutrition knowledge or is influenced by misleading information to decide on healthy choices related to dietary habits [ 2 , 19 ]. There is a significant increment in the adolescent adaptation to eating unhealthy food due to a lack of knowledge, unavailability, unaffordability, false perception of healthy foods, and socioeconomic boundaries [ 20 , 21 ]. Today, quality diet choice among adolescent has drastically declined after the introduction of unhealthy fast food or processed food into the market [ 22 ].
The environment at school is the main target for conducting education programs as they involve a large number of children and adolescents [ 15 ]. Likewise, students may adopt and maintain healthy eating habits with the support of a nutrition education program that emphasizes the benefits of nutrition [ 21 ]. Nutrition education is a critical component of any strategy aimed at changing behavior and promoting healthy eating habits [ 23 ]. It is important to empower school students to cope with this tremendous burden and bridge the gap regarding the rising issue of falsification, as well as adolescent food choices and the health consequences that follow. This can only be achieved by providing them with proper nutrition knowledge, promoting healthy snack habits, and changing their overall attitudes toward healthy eating habits. The Government of Nepal runs the School Health Nutrition Program (SHNP) to improve the health and nutritional status of school-aged children [ 24 ]. However, very few comprehensive educational programs targeting the nutritional concerns of adolescents with the scientific assessment of nutrition knowledge, attitude, and dietary habits are being implemented in Nepal. Therefore, this study aimed to investigate the effect of a nutrition education intervention on nutritional knowledge, attitude, and diet quality among school-going adolescents in selected private schools located in the urban settings of Nepal.
Study design and setting
This school-based quasi-experimental study was conducted among 12 − 19 years school-going adolescents in grades 6 to 10 in two private schools in Banepa Municipality, Kavrepalanchok district of Nepal. Banepa is located about 25 km to the east of Kathmandu the capital city of Nepal. This study was conducted between February 2020 and July 2020. The study was reported using Transparent Reporting of Evaluations with Non-randomized Designs (TREND) guidelines [ 25 ].
Participants
Study participants included 226 school-going adolescents, aged 12 − 19 years who were studying in grades 6 to 10 (Fig. 1 ). Those students who were able to answer the questionnaire items from grade 6 to grade 10 were present on the day of data collection were included in this study. Adolescents with medical conditions, such as physical and psychological issues, as well as those who were reluctant to participate and were absent on program days, were excluded from the study.
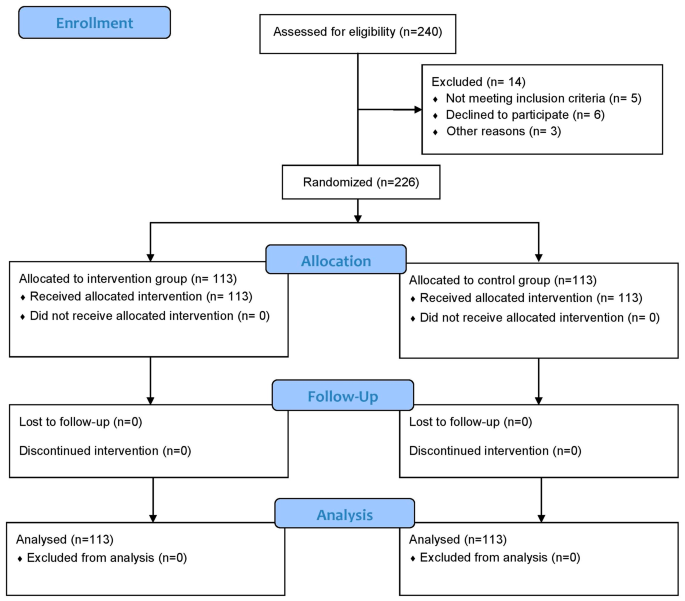
Flow diagram of the study
The primary outcome of this study was to measure the change in nutrition knowledge of participants after a 12-week nutrition educational intervention, and the secondary outcomes were to evaluate change in nutrition attitude and diet quality among school-going adolescents.
Intervention
In the intervention group, students were assigned to receive a nutrition education package, whereas the control group received no instruction regarding nutrition education, and they responded to questions based on regular health and nutrition education dissemination through the school curriculum/textbook. Follow-up data were collected after 12 weeks of nutrition education intervention. As per the nutrition education package, we provided 45 min of nutrition education sessions a day per week for intervention group in each grade (grade 6–10). Therefore, the students in the different grades received nutrition education session separately.
During the intervention phase, trained nutritionists/dietitians provided nutrition education to the intervention group using educational materials such as posters, leaflets, pamphlets, educational videos, and PowerPoint. The education package was developed by academic researchers and all materials reviewed by a multi-disciplinary expert group consisting of an academician and a dietitian before the intervention. A one-hour mini-lecture and interactive discussion session were conducted in the classroom. All the educational activities were carried out in the respective classroom for each section. The nutrition education sessions lasted approximately one hour in each class for five days and were held at the time of enrollment. Information and educational materials (posters, leaflets, pamphlets, educational videos, and PowerPoint) were handed out at the end of each session. The control group on the other hand did not receive the education package.
The nutrition education package contained important information on healthy eating habits, eating disorders in adolescents, food labels, knowledge of a balanced diet, and the consequences of poor eating habits. The origins and key roles of macro-and micronutrients, as well as the recommended dietary intake of various food items for teenagers and the principles of my plate, were also highlighted during the nutrition education session [ 26 ]. Follow-up visits were undertaken every four weeks to ensure the progression of healthy eating habits and a better understanding of nutrition.
Sample size
The sample size was determined using effect size estimations of the difference in means between two independent groups using nutrition knowledge as the primary outcome variable, with a significance level (two-tailed) of 0.05 and a statistical power of 90%. Based on a similar study conducted by Fahlman et al. (2008) [ 27 ] where, the proportion of the nutritional knowledge score in the intervention and control groups was 0.49 and 0.39, respectively. The final sample size was 226 (113 participants in the intervention group and 113 participants in the control group, respectively) with a 10% non-response rate. The sample size was calculated using a test comparing two means in Stata/MP version 14.1 (StataCorp LP, College Station, Texas).
Recruitment
A list of private schools was obtained from Banepa Municipality. Each school has approximately 350 adolescents enrolled. Of 20 schools, only two private schools were chosen purposively chosen because the adolescent students in the two schools were adequate to meet the required sample size. The allocation of the intervention and control groups among the two schools was determined through the use of flipping a coin(Fig. 2 ). A complete list of sections/classes for each school was compiled with the help of a school’s administration registry. All students in grades 6 to 10 who were willing to participate in the study were enrolled individually from the two schools for both the intervention ( n = 113) and control ( n = 113) groups. The average number of students in each of the schools was around 350; however, the total number of students included in the study ( n = 113 for each group) is less than the total number of students enrolled in the schools ( N = 350). We approached all students to participate in the study, although the study sample size was determined to be 113 for each group. Among them, a few students dropped out due to loss of follow-up, unwillingness to give consent, absence on the day of enrollment, and illness. Thus, not all students were included in the study.

Map showing study area. The map was created using ArcGIS desktop version 10.8. The shape file of the administrative districts and location for Nepal was obtained from the Government of Nepal, Ministry of Land Management, and Survey Department website and was publicly available for unrestricted use
Data collection tools and techniques
Data was collected by postgraduate (MSc. Nutrition and Dietetics) students who were provided with three days of training that included the objective of the study, data collection procedure, sampling method, ethical aspects of the study, and data entry techniques. Face-to-face interviews were conducted using pre-tested semi-structured questionnaires. Baseline interviews lasted almost 30 min in each school, and post-test data collection was conducted after 12 weeks of nutrition education intervention. All the tools were originally developed in the English language. Further, the tools were translated into the Nepali language and back translated into English to ensure the validity (and reliability) of the tool. Pretesting of the tools was carried out among 28 students from the neighboring school of Banepa Municipality.
The socio-demographic information includes age, sex, grade, religion, ethnicity, parent’s occupation, and parent’s education. The nutrition knowledge, attitude, and diet quality questionnaires were adapted from a previous study [ 21 ] and then translated into Nepali. The research committee and faculty members reviewed the pre-tested questionnaire to establish its validity and reliability. The questionnaire was revised appropriately based on their feedback. The Nepali version of the nutrition knowledge, attitude, and diet quality questionnaire had acceptable internal consistency (Cronbach’s alpha of 0.62, 0.72, and 0.61, respectively). However, the internal consistency of a score/scale is good at ≥ 0.7, and findings of ≥ 0.6 have also been deemed satisfactory or acceptable [ 28 , 29 ].
Nutrition knowledge levels were determined based on eighteen questions (Q1 − Q18). The short form of the Food Frequency Questionnaire for Polish Children (SF-FFQ4PolishChildren) was adopted first in English and developed by Whati et al. [ 30 ], then translated into Nepali and modified to fit the Nepalese context. Correct answers were scored one point, while wrong or “don’t know” answers and missing data were given zero. The points of each respondent were totaled and examined further.
Attitudes toward nutrition were determined using a three-factor eating questionnaire (TFEQ13) designed specifically for youngsters. We utilized a simplified version of the questionnaire (TFEQ10) used by Hamulka et al. [ 21 ]., which consisted of only ten statements that further modified and verified the questionnaire for Nepalese settings. Three subscales, in a shortened version, were developed: emotional eating (Q1, Q3), Uncontrolled Eating (Q2, Q4, Q5, Q6, Q8), and Cognitive Restraint of Eating (Q7, Q9, Q10). Each subscale’s score was determined as the total of points allocated to respondents’ responses. All the responses were scored such that the responder may pick one of four options for each question: “definitely yes” (3 points), “rather yes” (2 points), “rather not” (1 point), and “absolutely not” (0 points).
Participants were asked to specify their usual frequency of consumption for the past 12 months for breakfast and school meals and nine food items such as dairy products, fish, vegetables, fruits, fruits or mixed fruit-veggie juices, fast foods, sweetened carbonated drinks, energy drinks, and sweets or confectionery [ 21 ]. It consisted of 11 questions. The diet quality scores were used for pro-Healthy Diet Index (pHDI), which were obtained by adding the daily frequencies of specific food items (as previously described) and expressing them as a percentage (range: 0 to 100). The diet quality scores were established (a priori approach) based on usual food frequency consumption within the last 12 months [ 21 ].
Data management and analysis
The collected data were entered into EpiData software 3.1v and transferred into Stata/MP version 14.1 (StataCorp LP, College Station, Texas) for statistical analysis. The Chi-squared test was used to compare socio-demographic factors in the intervention and control groups at baseline. The student’s two-sample t-test was used to compare post-intervention magnitude of changes in nutrition knowledge, nutrition attitude, and diet quality scores between the intervention and control groups. To estimate changes between the control and intervention groups at baseline and follow-up, the Difference in Differences (DID) analysis was performed [ 31 , 32 ]. We did not randomly assign the participants in the control and intervention group due to the nature of quasi-experimental study design. So, we used DID methods expecting to control heterogeneity between treatment and control group and achieve better exchangeability. In addition, there was a chance of both information and selection bias, which DID help minimize such bias by comparing changes in outcomes within each group. The statistical significance was considered at p -value < 0.05 and 95% confidence intervals (CIs).
Ethical considerations
The ethical approval for this study was obtained from the Ethical Review Board (ERB) of the Nepal Health Research Council (Ref.no 1976). Formal permission was also obtained from the respective private schools. Written informed consent was obtained from all parents or legal guardians for eligible participants. The data collector also shared the objectives of the study with each participant before the baseline data collection and nutrition education. Participants and their parents or legal guardian were informed about voluntary participation, their right to refusal at any point, and the confidentiality of their identity.
A total of 226 participants were categorized into intervention ( n = 113) and control ( n = 113) groups. All the participants completed the study. The average (SD) age of the participants was 14.8 (1.2) years. There was no significant difference between the intervention and control groups in terms of socio-demographic variables such as age, sex, religion, and parental education. However, significant differences between these groups were observed in ethnicity, family type, and parental occupation (Table 1 ).
In this study, Fig. 3 a and b, and Fig. 3 c depicted the comparison of nutrition knowledge, attitude, and diet quality scores, respectively between intervention and control groups at baseline and follow-up of the study. The intervention group had a higher median score than the control group at the follow-up. (Fig. 3 a), (Fig. 3 b) and (Fig. 3 c).
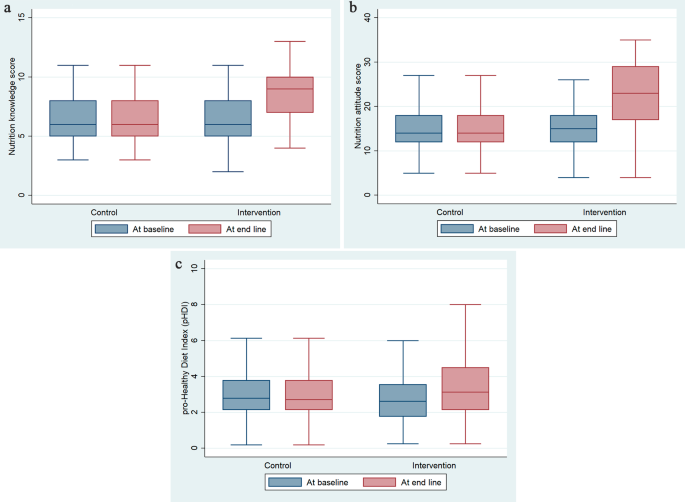
a . Effectiveness of education intervention on students’ nutrition knowledge. b . Effectiveness of education intervention on students’ nutrition attitude. c . Effectiveness of education intervention on students’ diet quality
At the end of 12 weeks of nutrition education intervention, the magnitude of changes in knowledge score between the intervention and control group was 1.80 with the nutrition education intervention (95% CI: 1.11 − 2.49). The difference was 0.98 (95% CI: 0.42 − 1.54) for emotional eating, 3.60 (95% CI: 2.10 − 5.09) for uncontrolled eating, and 2.26 (95% CI: 1.51 − 3.01) for cognitive restraint of eating (Table 2 ).
This study demonstrated that educational intervention was effective to improve nutrition knowledge, attitude, and diet quality among school-going adolescents. As the burden of diet-related diseases continue to surge worldwide [ 33 , 34 ], nutrition education interventions as part of public health school intervention may have implications to improve the overall nutritional status among school-going adolescents.
In the current study, there was a significant improvement in the mean nutrition knowledge score of 1.80 after the implementation of the intervention compared to the control group. This finding is in line with previous studies [ 16 , 18 , 35 , 36 ]. Likewise, a systematic review based on Sub-Saharan Africa (SSA) provides evidence in favor of the positive impact of nutrition education on nutrition knowledge, where nutrition knowledge improved from 45.4 to 58.8% in the intervention group compared to the control group [ 37 ]. Furthermore, another study found that nutrition knowledge increased significantly soon after the nutrition education intervention and six months thereafter [ 38 ]. In addition, students with nutrition education intervention showed higher nutritional knowledge scores. The improvement in knowledge scores could be explained by the participants’ improved understanding and awareness regarding the role of a healthy diet and healthy eating behavior on their health and nutrition status [ 18 ]. As the burden of diet-related disorders continues to rise worldwide, investing in high-quality research to determine nutrition knowledge is a foresighted approach [ 33 ]. Nutrition education is used to encourage school adolescents to adopt healthy eating habits for the rest of their lives [ 18 ]. Also, successful nutrition education intervention should include content and teaching strategies that are suitable for the children and address change in the environment [ 39 ].
In our study, students in the intervention group had significantly improved emotional eating as well as cognitive restraint of eating scores. An increase in cognitive level leads to healthier eating and remarkably higher food and nutrition knowledge [ 40 ]. Evidence suggested that school-based health intervention programs could significantly influence eating behaviors and help adolescents adopt healthy eating practices [ 21 , 41 ], which could be the reason for the significant improvement in the nutrition attitude of the participants of our study which might be connected with the way of presenting nutrition topics and the improvement in the learners’ nutrition knowledge, attitude as well as practice [ 33 ].
With the mixed results in the available literature [ 42 , 43 ], the results of this study support changed lifestyle habits and improved diet quality of the targeted participants. Further to this another intervention study conducted observed no significant improvements in diet quality [ 44 ]. These inconsistent results might be contributed to the variety of approaches adopted, duration of intervention, efficacy, intervention quality, research ethics endorsed, and the overall methodology applied to achieve the desired objectives [ 42 , 43 ]. Moreover, the poor availability of diverse food items due to seasonal factors might influence the practice of improved diet quality [ 45 ].
The strength of this study was the educational approach, which was relatively simple, short-term, and contextualized in a Nepalese setting thus making it feasible to implement. This study was using a quasi-experimental design that included both an intervention and a control group. This study included an analysis of the difference in difference using a linear regression model between the two groups. This information can be used to develop targeted nutrition education programs that are integrated into the academic curriculum. Despite its strength, this study had a few limitations. Since the study used quasi-experimental study design, participants were not randomly assigned that leads to lack of exchangeability. As the study participants were confined to two private schools in the urban area and the subsequent selection of the participants were made based on their willingness to participate in the study, study findings should cautiously be generalized to other settings. Likewise, information collected through face-to-face interviews might be prone to social desirability bias. However, we have included cross-validation questions e necessary in the tools to minimize the potential social desirability bias. In addition, compliance with nutrition education was not assessed in this study.
This study concludes that the nutrition education intervention was effective to enhance the nutritional knowledge and attitude among school-going adolescents in Nepal. The findings of this study indicate that nutrition education in secondary schools is a good approach to improving adolescent nutrition knowledge, attitudes, and diet quality. Adopting a tailored nutrition education intervention program as part of government administered public health school intervention incorporating interactive discussions and knowledge of food habits is beneficial to building positive attitudes towards the importance of nutrition, enhancing nutrition knowledge, and supporting healthy eating in school-going adolescents.
Data availability
The datasets used during the current study are available from the corresponding author upon reasonable request.
Abbreviations
Confidence interval
Confidence intervals
Difference in difference
Difference in Differences
Ethical Review Board
Pro-Healthy Diet Index
Food Frequency Questionnaire for Polish Children
School Health Nutrition Program
Sub-Saharan Africa
Three-factor eating questionnaire
Reporting of Evaluations with Non-randomized Designs
World Health Organization (WHO). Global action plan for the prevention and control of noncommunicable diseases 2013–2020. 2013. doi:978 92 4 1506236.
Moitra P, Madan J, Verma P. Impact of a behaviourally focused nutrition education intervention on attitudes and practices related to eating habits and activity levels in Indian adolescents. Public Health Nutr. 2021;24:2715–26.
Article PubMed PubMed Central Google Scholar
World Health Organization (WHO). Adolescent health. 2022. https://www.who.int/health-topics/adolescent-health#tab=tab_1 . Accessed 9 May 2022.
United Nations Children’s Fund. Adolescents Statistics - UNICEF DATA. 2019. https://data.unicef.org/topic/adolescents/overview/ . Accessed 1 Apr 2022.
Christian P, Smith ER. Adolescent undernutrition: global burden, physiology, and nutritional risks. Ann Nutr Metab. 2018;72:316–28. https://doi.org/10.1159/000488865
Article CAS PubMed Google Scholar
Biesalski Hans K, Jana T. Micronutrients in the life cycle: requirements and sufficient supply. NFS J. 2018;11:1–11.
Article Google Scholar
Chaudhary A, Sudzina F, Mikkelsen BE. Promoting healthy eating among young people—a review of the evidence of the impact of school-based interventions. Nutrients. 2020;12:1–34. https://doi.org/10.3390/NU12092894
Micha R, Karageorgou D, Bakogianni I, Trichia E, Whitsel LP, Story M et al. Effectiveness of school food environment policies on children’s dietary behaviors: a systematic review and meta-analysis. PLoS ONE. 2018;13.
Bauer JM, Reisch LA. Behavioural insights and unhealthy dietary choices: a review of current evidence. J Consum Policy 2018 421. 2018;42:3–45. https://doi.org/10.1007/S10603-018-9387-Y
Singh DR, Sunuwar DR, Dahal B, Sah RK. The association of sleep problem, dietary habits and physical activity with weight status of adolescents in Nepal. BMC Public Health. 2021;21:1–17. https://doi.org/10.1186/S12889-021-10985-5/TABLES/3
Trude ACB, Kharmats AY, Jones-Smith JC, Gittelsohn J. Exposure to a multi-level multi-component childhood obesity prevention community-randomized controlled trial: patterns, determinants, and implications. Trials. 2018;19. https://doi.org/10.1186/S13063-018-2663-Y
Querol SE, Iqbal R, Kudrna L, Al-Khudairy L, Gill P. The double burden of malnutrition and associated factors among south Asian adolescents: findings from the global school-based student health survey. Nutrients. 2021;13. https://doi.org/10.3390/NU13082867
Bakrania, Shivit; Ghimire, Anita; Balvin, Nikola (2018). Bridging the Gap to Understand Effective Interventions for Adolescent Well-being: An evidence gap map on protection, participation, and financial and material well-being in low- and middle-income countries, Miscellanea, UNICEF Office of Research - Innocenti, Florence. https://www.unicef-irc.org/publications/pdf/evidence_gap_map_adolescent_well_being_report.pdf
Birch L, Savage JS, Ventura A. Influences on the development of children’s eating behaviours: from infancy to adolescence. Can J Diet Pract Res. 2007;68:s1. /pmc/articles/PMC2678872/ . Accessed 1 Apr 2022.
Story M, Kaphingst KM, French S. The role of schools in obesity prevention. Futur Child. 2006;16:109–42. https://doi.org/10.1353/FOC.2006.0007
Sharif Ishak SIZ, Chin YS, Mohd Taib MN, Chan YM, Mohd Shariff Z. Effectiveness of a school-based intervention on knowledge, attitude and practice on healthy lifestyle and body composition in Malaysian adolescents. BMC Pediatr. 2020;20. https://doi.org/10.1186/S12887-020-02023-X
Jacob CM, Hardy-Johnson PL, Inskip HM, Morris T, Parsons CM, Barrett M, et al. A systematic review and meta-analysis of school-based interventions with health education to reduce body mass index in adolescents aged 10 to 19 years. Int J Behav Nutr Phys Act. 2021;18:1–22. https://doi.org/10.1186/S12966-020-01065-9/FIGURES/3
Rani MA, Shriraam V, Zachariah R, Harries AD, Satyanarayana S, Tetali S, et al. Does a nutrition education programme change the knowledge and practice of healthy diets among high school adolescents in Chennai. India? Health Educ J. 2013;72:733–41.
Rathi N, Riddell L, Worsley A. Parents’ and teachers’ views of food environments and policies in Indian private secondary schools. Int J Environ Res Public Health. 2018;15. https://doi.org/10.3390/IJERPH15071532
Tavassoli E, Vardanjani A, Reisi M, Javadzade H, Pour Z. The effect of nutrition education on knowledge, attitude, and performance about junk food consumption among students of female primary schools. J Educ Health Promot. 2015;4:53.
Hamulka J, Wadolowska L, Hoffmann M, Kowalkowska J, Gutkowska K. Effect of an education program on nutrition knowledge, attitudes toward nutrition, diet quality, lifestyle, and body composition in Polish teenagers. The ABC of healthy eating project: design, protocol, and methodology. Nutrients. 2018;10.
Wadolowska L, Kostecka M, Kowalkowska J, Jeruszka-Bielak M, Tomaszewska M, Danielewicz A et al. Sustainability of a multi-component education program (Abc of healthy eating) after three months and nine months: the socioeconomic context in improving nutrition knowledge in Polish teenagers. Nutrients. 2021;13.
Sunuwar DR, Sangroula RK, Shakya NS, Yadav R, Chaudhary NK, Pradhan PMS. Effect of nutrition education on hemoglobin level in pregnant women: a quasi-experimental study. PLoS ONE. 2019;14.
Government of Nepal, Ministry of Health and Population, Ministry of Education. Joint Action Plan 2071/72-2076/77 School Health and Nutrition. 2016.
Des Jarlais DC, Lyles C. Crepaz N&, the trend group. Standards for reporting non-randomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Heal Heal. 2004;99:1075–80.
Google Scholar
US Department of Agriculture. USDA MyPlate. https://www.myplate.gov/ . Accessed 10 Feb 2023.
Fahlman MM, Dake JA, McCaughtry N, Martin J. A pilot study to examine the effects of a nutrition intervention on nutrition knowledge, behaviors, and efficacy expectations in middle school children: research article. J Sch Health. 2008;78:216–22.
Article PubMed Google Scholar
Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychom 1951 163. 1951;16:297–334. https://doi.org/10.1007/BF02310555
Taber KS. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ. 2018;48:1273–96. https://doi.org/10.1007/S11165-016-9602-2/TABLES/1
Whati LH, Senekal M, Steyn NP, Nel JH, Lombard C, Norris S. Development of a reliable and valid nutritional knowledge questionnaire for urban South African adolescents. Nutrition. 2005;21:76–85. https://doi.org/10.1016/J.NUT.2004.09.011
Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. JAMA. 2014;312:2401–2. https://doi.org/10.1001/JAMA.2014.16153
Oli N, Vaidya A, Eiben G, Krettek A. Effectiveness of health promotion regarding diet and physical activity among Nepalese mothers and their young children: the heart-health associated research, dissemination, and intervention in the community (HARDIC) trial. Glob Health Action. 2019;12. https://doi.org/10.1080/16549716.2019.1670033
Spronk I, Kullen C, Burdon C, O’Connor H. Relationship between nutrition knowledge and dietary intake. Br J Nutr. 2014;111:1713–26. https://doi.org/10.1017/S0007114514000087
Worsley A. Nutrition knowledge and food consumption: can nutrition knowledge change food behaviour? Asia Pac J Clin Nutr. 2002;11(Suppl 3):579–85. https://doi.org/10.1046/J.1440-6047.11.SUPP3.7.X
Asakura K, Mori S, Sasaki S, Nishiwaki Y. A school-based nutrition education program involving children and their guardians in Japan: facilitation of guardian-child communication and reduction of nutrition knowledge disparity. Nutr J. 2021;20:1–13. https://doi.org/10.1186/S12937-021-00751-Z/TABLES/3
De Villiers A, Steyn NP, Draper CE, Hill J, Gwebushe N, Lambert EV, et al. Primary school children’s nutrition knowledge, self-efficacy, and behavior, after a three-year healthy lifestyle intervention (HealthKick). Ethn Dis. 2016;26:171. https://doi.org/10.18865/ED.26.2.171
Kyere P, Veerman JL, Lee P, Stewart DE. Effectiveness of school-based nutrition interventions in sub-saharan Africa: a systematic review. Public Health Nutr. 2020;23:2626–36.
Chojnacka A, Górnicka M, Szewczyk K. Long-term effect of one-time nutritional education in school on nutritional knowledge of early school-aged children. Rocz Panstw Zakl Hig. 2021;72:155–64.
Teo CH, Chin YS, Lim PY, Masrom SAH, Shariff ZM. School-based intervention that integrates nutrition education and supportive healthy school food environment among Malaysian primary school children: a study protocol. BMC Public Health. 2019;19:1427. https://doi.org/10.1186/s12889-019-7708-y
Brown R, Seabrook JA, Stranges S, Clark AF, Haines J, O’Connor C, et al. Examining the correlates of adolescent food and nutrition knowledge. Nutrients. 2021;13:2044. https://doi.org/10.3390/nu13062044
Contento IR, Manning AD, Shannon B. Research perspective on school-based nutrition education. J Nutr Educ. 1992;24:247–60.
Al-Khudairy L, Loveman E, Colquitt JL, Mead E, Johnson RE, Fraser H, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev. 2017;6. https://doi.org/10.1002/14651858.CD012691
Mead E, Brown T, Rees K, Azevedo LB, Whittaker V, Jones D, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. 2017;6. https://doi.org/10.1002/14651858.CD012651
Berry DC, McMurray R, Schwartz TA, Skelly A, Sanchez M, Neal M, et al. Rationale, design, methodology and sample characteristics for the family partners for health study: a cluster randomized controlled study. BMC Public Health. 2012;12. https://doi.org/10.1186/1471-2458-12-250
Crane TE, Latif YA, Wertheim BC, Kohler LN, Garcia DO, Rhee JJ, et al. Does season of reported dietary intake influence diet quality? Analysis from the women’s health initiative. Am J Epidemiol. 2019;188:1304. https://doi.org/10.1093/AJE/KWZ087
Download references
Acknowledgements
We would like to thank all the participants who provided their valuable time, response, and participation in the study. We are grateful to all the teachers and students of the respective schools for their facilitation, and cooperation in undertaking this research.
This research received no specific financial support from any funding agencies.
Author information
Authors and affiliations.
Department of Nutrition and Dietetics, College of Applied Food and Dairy Technology, Purbanchal University, Lalitpur, Nepal
Public Health Promotion and Development Organization, Kathmandu, Nepal
Dirghayu KC
School of Human and Health Sciences, University of Huddersfield, Huddersfield, UK
Devendra Raj Singh
Faculty of Medicine Nursing and Health Sciences, Monash University, Melbourne, Australia
Raja Ram Dhungana
Department of Community Medicine, Maharajgunj Medical Campus, Institute of Medicine, Kathmandu, Nepal
Pranil Man Singh Pradhan
Department of Nutrition and Dietetics, Nepal Armed Police Force Hospital, Kathmandu, Nepal
Dev Ram Sunuwar
Department of Nutritional Science, University of Michigan School of Public Health, Ann Arbor, USA
You can also search for this author in PubMed Google Scholar
Contributions
Sagar Raut (SR), Dirghayu KC (DKC), Devendra Raj Singh (DRSi), Raja Ram Dhungana (RRD), Pranil Man Singh Pradhan (PMSP), Dev Ram Sunuwar (DRSu). Conceived and designed the study: SR, DKC, DRSi, RRD, PMSP, and DRSu. Tools translation to the Nepali language: SR and DRSu. Data collection: SR and DRSu. Analyzed the data: SR and DRSu. Writing and editing the manuscript: SR, DKC, DRSi, RRD, PMSP, and DRSu. Critical revision of the manuscript: SR, DKC, DRSi, RRD, PMSP, and DRSu. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Dev Ram Sunuwar .
Ethics declarations
Ethical approval and consent to participate.
All methods of this study were carried out under the Declaration of Helsinki’s ethical principle for medical research involving human subjects. The ethical clearance for this study was obtained from the Ethical Review Board (ERB) at the Nepal Health Research Council (Ref: 1976). Formal permission was also obtained from the respective private schools. Written informed consent was obtained from all parents or legal guardians for eligible participants. The data collector also shared the objectives of the study with each participant before the baseline data collection and nutrition education. Participants and their parents or legal guardian were informed about voluntary participation, their right to refusal at any point, and the confidentiality of their identity.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Raut, S., KC, D., Singh, D.R. et al. Effect of nutrition education intervention on nutrition knowledge, attitude, and diet quality among school-going adolescents: a quasi-experimental study. BMC Nutr 10 , 35 (2024). https://doi.org/10.1186/s40795-024-00850-0
Download citation
Received : 10 February 2023
Accepted : 19 February 2024
Published : 27 February 2024
DOI : https://doi.org/10.1186/s40795-024-00850-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescence
- Diet Quality
- Nutrition Education
BMC Nutrition
ISSN: 2055-0928
- General enquiries: [email protected]

COMMENTS
Nutrition education is one of the most complex and complicated areas of health care. the most difficult task is to motivate and persuade the target audience to follow dietary patterns and change their lifestyles. Best practices are based on motivation and emotional appeal aimed to influence the mind and feelings of listeners and students.
US students receive less than 8 hours of required nutrition education each school year, 9 far below the 40 to 50 hours that are needed to affect behavior change. 10,11 Additionally, the percentage of schools providing required instruction on nutrition and dietary behaviors decreased from 84.6% to 74.1% between 2000 and 2014. 9. Given the ...
that health and balanced nutrition education has a positive effect on students' nutritional habits, body structure and academic achievement. The aim of this study is to determine whether the nutrition education program has an effect on students' nutritional attitudes and behaviors, sports attitudes and performance, and academic achievement.
A good and balanced diet has proven to have a significant effect on the physical and mental development of the child, especially in their early life. Studies have shown that good nutrition enhances school performance and learning abilities. Nutrition education is important in the early stages because is a key element to promoting lifelong ...
1. Introduction. Nutrition‐related health conditions, such as obesity, Type 2 diabetes, and hypertension are becoming prevalent in children (Goran et al., 2003, Kelsey et al., 2014).Children with these conditions often suffer physical discomfort, ill-health, lower self‐esteem, poorer academic outcomes and negative socio-emotional (van Geel et al., 2014, Reilly and Kelly, 2011).
Get a custom essay on Nutrition Education for School-Age Children. One more essential theme outlined in the literature is the implementation of physical activity in schools to prevent and decrease overweight and obesity in children. In the recent article, Stephens, Black, Chapman, Velazquez, and Rojas (2016) reveal the low interest of students ...
What is effective nutrition education? Per Contento,Nutrition education is any combination of educational strategies, accompanied by environmental supports, designed to facilitate voluntary adoption of food choices and other food- and nutrition-related behaviors conducive to health and well-being. Nutrition education is delivered through multiple venues and involves activities at the ...
1. school nutrition policies 2. awareness and capacity building of the school community 3. nutrition and health promoting curricula 4. supportive school environment for good nutrition 5. supportive school nutrition and health services. Review methodology and evidence identified
Nutrition in Middle Childhood and Adolescence. 112 UNICEF's Programmatic Guidance for Nutrition in Middle Childhood and Adolescence includes specific priorities of nutritious foods, healthy food environments in schools and beyond, micronutrient supplementation and deworming, nutrition education in school curricula, and healthy dietary ...
Advocacy is a major part of SNEB's mission, and advocating for funding for nutrition education research and programs is a high priority. The SNEB Advisory Committee on Public Policy actively encourages members to learn about priority issues, offering tips on working with decision-makers and weekly policy updates to help inform and motivate ...
An argument in favor of a new era for nutrition education is also supported by a diverse international group of scholars and experts in food and nutrition working on a project entitled "New Nutrition Science." This group unanimously agreed that now is the time to add social and environmental dimensions to the definition and practice of ...
Nutrition Education Essays. College Diet Solutions. Possible Solutions The possible solutions to the diet challenge experienced by college students are discussed as a multi-varied approach is given to initiate positive changes in students' dietary behaviors. The first solution is having nutrition education programs in colleges as a reaction ...
Get a custom essay on Nutrition & Students Academic Performance. Extant literature demonstrates that although parents, educators, and health professionals continue to tout the interdependence between what students eat and their educational achievement, evidence for this association is not always obvious, not mentioning that recurrent biases on ...
250 Words Essay on Food and Nutrition Introduction to Food and Nutrition. Food and nutrition are integral elements of human existence, playing a pivotal role in our health and wellbeing. ... Nutrition education can empower individuals to make informed food choices, thereby promoting public health at large. In conclusion, food and nutrition are ...
Long Essay on Nutrition is usually given to classes 7, 8, 9, and 10. As the name suggests, 'nutrition' includes in itself' nutrients' which can be broadly classified as carbohydrates, proteins, fats, vitamins, minerals, roughage, and water. A balanced amount of these nutrients in the right proportions constitute a healthy diet.
Nutrition education is an important element in an overall strategy aimed at improving food security and preventing all forms of malnutrition. Schools (from pre-school to secondary) are ideal settings for promoting lifelong healthy eating habits and lifestyles. 132. Most countries in the region implement school health and nutrition programmes ...
Conclusion. In conclusion, nutrition is an essential component of health that impacts both physical and mental well-being. While the benefits of a balanced diet are well-documented, challenges such as food accessibility, socioeconomic factors, and misinformation can hinder individuals from achieving optimal nutrition.
1450 Words6 Pages. Nutrition Education. Nutritional education is define as a formal process to instruct or train a patient/client in a skill or to impart knowledge to help patient/clients in a voluntary way manage or modify food choices and eating behavior to maintain or to improve health (1).Nutrition education can be delivered using a variety ...
Introduction Healthy eating is necessary for the development and good health of children between the ages of 3-15. The learning institutions are determined to promote and educate children on healthy eating (Marcano-Olivier et al., 2021). However, children between the ages 3-15 are still engaging in unhealthy nutrition practices (Weihrauch-Blüher et al., 2023). Thus, there is […]
Nutrition education is being used to encourage school adolescents to adopt healthy eating habits. To the best of our knowledge, very little study has been undertaken in Nepal to examine the effectiveness of nutrition education programs. This study aimed to assess the effect of nutrition education on nutritional knowledge, attitude, and diet quality among school-going adolescents in selected ...
In conclusion, the importance of food and nutrition cannot be overstated. Their impact on physical health, mental well-being, and overall quality of life is significant. It is crucial to prioritize food and nutrition in order to achieve optimal health and well-being. By making informed food choices and ensuring a balanced diet, individuals can ...